Disorders of the Foot and Ankle
SECTION 1 BIOMECHANICS OF THE FOOT AND ANKLE
SECTION 2 PHYSICAL EXAMINATION OF THE FOOT AND ANKLE
SECTION 3 RADIOGRAPHIC EVALUATION OF THE FOOT AND ANKLE
SECTION 5 JUVENILE AND ADOLESCENT HALLUX VALGUS
SECTION 7 LESSER-TOE DEFORMITIES
SECTION 8 HYPERKERATOTIC PATHOLOGIES
SECTION 11 NEUROLOGIC DISORDERS
I. Interdigital Neuritis (Morton Neuroma)
IV. Anterior Tarsal Tunnel Syndrome
V. Sequelae of Upper Motor Neuron Disorders
This chapter provides a review of adult foot and ankle disorders and deformities. Pediatric and congenital deformities are covered in Chapter 3, Pediatric Orthopaedics.
section 1 Biomechanics of the Foot and Ankle
The primary functions of the foot and ankle are to provide support and forward ambulation.
1. Ankle mortise is formed by the tibial plafond, medial malleolus, and lateral malleolus (Figure 6-1).
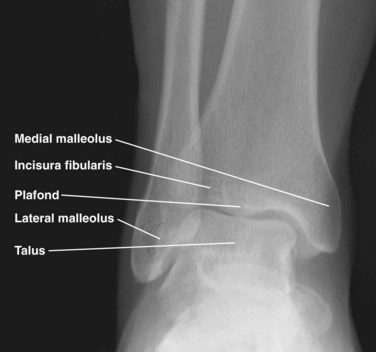
Figure 6-1 Anteroposterior radiograph of the ankle.
2. Mortise articulates with the dome of the talus.
3. Mortise widens and ankle becomes more stable in dorsiflexion due to shape of talar dome (wider anteriorly).
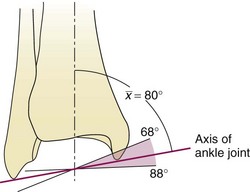
4. A simplified model of the ankle joint has a horizontal axis from anteromedial to posterolateral and a coronal axis from superomedial directed distally and laterally to the tip of the fibula (between the malleoli) (Figure 6-2).
5. Responsible for most sagittal plane motion of the foot and ankle
6. 23 to 48 degrees plantar flexion
1. Distal fibula—convex medial surface
2. Incisura fibularis—concave surface of distal lateral tibia
3. Fibula rotates (~2 degrees) within incisura during ankle motion and ambulation. Ankle dorsiflexion results in external rotation and proximal translation of the fibula.
4. Mortise widens 1 to 1.5 mm during motion from plantar flexion to dorsiflexion.
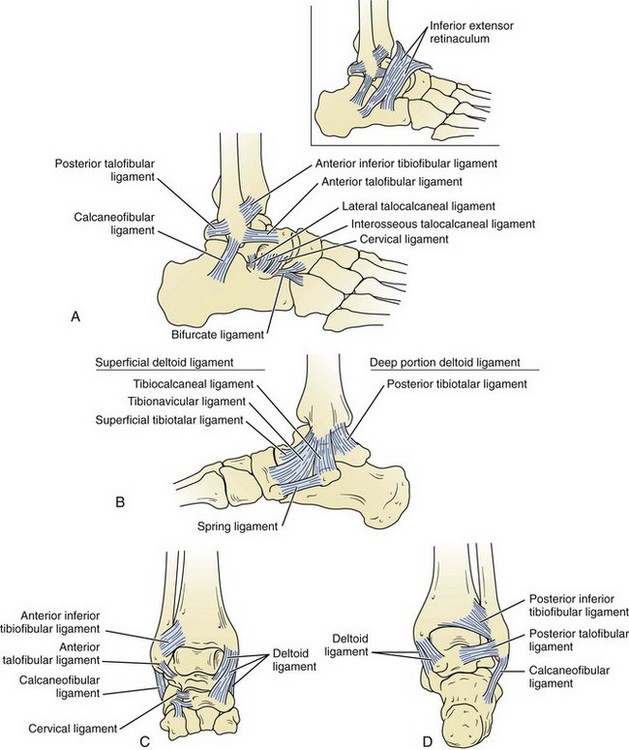
C Ligamentous anatomy (Figure 6-3)
1. The lateral ankle ligaments function as a restraint to varus forces at the ankle.
 The anterior talofibular ligament originates from the anteroinferior aspect of the lateral malleolus, 1 cm proximal to its tip, and extends to the lateral aspect of the talar neck.
The anterior talofibular ligament originates from the anteroinferior aspect of the lateral malleolus, 1 cm proximal to its tip, and extends to the lateral aspect of the talar neck.
 The calcaneofibular ligament extends from the tip of the lateral malleolus to the lateral aspect of the calcaneus.
The calcaneofibular ligament extends from the tip of the lateral malleolus to the lateral aspect of the calcaneus.
 The posterior talofibular ligament extends from the posterior lateral malleolus to the posterolateral talus.
The posterior talofibular ligament extends from the posterior lateral malleolus to the posterolateral talus.
 The anterior talofibular ligament is the weakest ankle ligament, and the posterior talofibular ligament is the strongest.
The anterior talofibular ligament is the weakest ankle ligament, and the posterior talofibular ligament is the strongest.
2. The distal tibiofibular joint (ankle syndesmosis) and fibula provide stability against lateral talar translation.
3. Deltoid ligament complex—main stabilizer of the ankle during stance
 The deep deltoid ligament extends from the apex of the medial malleolus to the medial talar body. It functions primarily to resist lateral talar translation.
The deep deltoid ligament extends from the apex of the medial malleolus to the medial talar body. It functions primarily to resist lateral talar translation.
 The superficial deltoid ligament extends from the distal medial malleolus to the navicular bone, sustentaculum tali of the calcaneus, medial talus, and spring ligament. It functions primarily to resist valgus ankle force (i.e., talar tilt).
The superficial deltoid ligament extends from the distal medial malleolus to the navicular bone, sustentaculum tali of the calcaneus, medial talus, and spring ligament. It functions primarily to resist valgus ankle force (i.e., talar tilt).
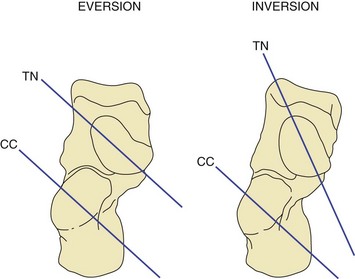
1. The hindfoot includes the talus, calcaneus, and cuboid. The subtalar, calcaneocuboid (CC), and talonavicular (TN) joints are included (Figure 6-4). The hindfoot functions in inversion and eversion.

Figure 6-4 Lateral radiograph of the foot.
E The midfoot begins at the articulation between the navicular and the cuneiforms along with cuboid and the fourth and fifth metatarsals. The midfoot also includes the tarsometatarsal (TMT) joints.
F The forefoot includes all structures distal to the TMT joints (Figure 6-5).

Figure 6-5 Anteroposterior radiograph of the foot.
G The CC and TN joints are collectively referred to as the midtarsal, transverse tarsal, or Chopart joint.
1. This joint is important for providing stability of the hindfoot and midfoot to produce a rigid lever at heel-rise.
2. During heel-strike (hindfoot valgus, forefoot abduction, and dorsiflexion of the ankle), the transverse tarsal joints are parallel and supple, adapting to the uneven ground.
3. During toe-off (hindfoot varus, forefoot adduction, and plantar flexion of the ankle), these joints become divergent and lock, providing stiffness to the foot for forward propulsion (Figure 6-6).
H The collective TMT joint complex is referred to as the Lisfranc joint.
I The foot is also divided into three columns.
1. The medial column includes the first metatarsal, the medial cuneiform, and the navicular.
2. The middle column includes the second and third metatarsals, the middle cuneiform, and the lateral cuneiform.
3. The lateral column includes the fourth and fifth metatarsals and the cuboid.
4. The lateral column has the most sagittal mobility, and the middle column has the least.
5. The sagittal mobility of the lateral column imparts the flexibility necessary for walking on uneven ground.
6. The rigidity of the middle column allows for a rigid lever arm during push-off.
J The foot has longitudinal and transverse arches. Stability of these arches is provided by a combination of the bony architecture, ligamentous attachments, and muscle forces.
K Ligamentous stability to the midfoot is provided through longitudinal and transverse ligaments on the plantar and dorsal aspects of each joint.
1. The plantar ligaments are thicker and stronger than their dorsal counterparts.
2. The primary stabilizer of the longitudinal arch is the interosseous ligaments and not the plantar fascia. The plantar fascia is a secondary stabilizer.
L The Lisfranc joint complex has a specialized bony and ligamentous structure, providing stability to this joint.
1. The middle cuneiform ends more proximally than the medial and lateral cuneiforms. The second metatarsal therefore extends more proximally than the surrounding metatarsals. This “keystone” effect imparts inherent bony stability.
2. Dorsal and plantar ligaments extend from the second metatarsal to each of the three cuneiforms.
3. The largest and strongest of these ligaments is the Lisfranc ligament, traveling from the medial cuneiform to the base of the second metatarsal.
M The midfoot provides an important bridge between the hindfoot and forefoot. It provides both flexibility and stability necessary for normal gait and other activities.
A The bony forefoot comprises the metatarsals and phalanges.
B The first metatarsal is the widest and shortest and bears 50% of the weight during gait.
C The second metatarsal is usually the longest and experiences more stress than the other lesser metatarsals.
D The lesser toes are controlled by a balance among them.
E The intrinsic tendons pass plantar (providing a flexion force) to the MTP joint axis proximally and pass dorsal to the axis distally (providing an extension force).
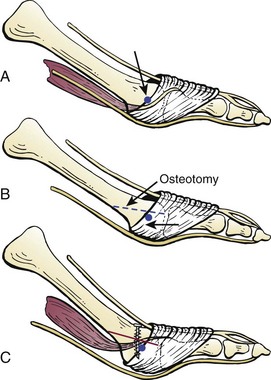
1. Plantar migration of this axis after a Weil (oblique shortening) osteotomy of the metatarsal leads to a “cock-up” toe. The tendons are now relatively dorsal to the MTP axis of rotation (Figure 6-7).
2. Loss of intrinsic function as seen in hereditary and motor sensory neuropathy or diabetic neuropathy predictably leads to claw toes.
III FOOT POSITIONS VERSUS FOOT MOTIONS
A Foot positions are defined in a manner different from that of foot motions.
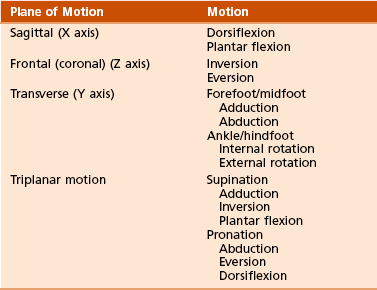
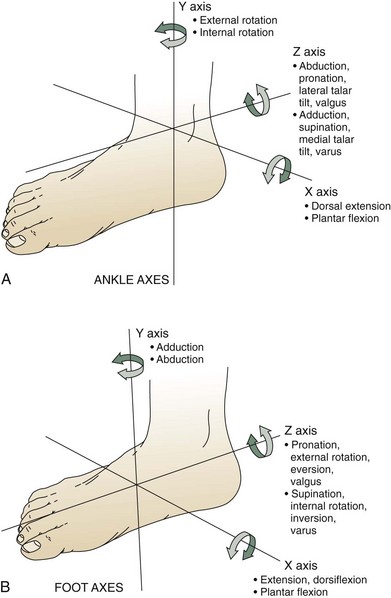
C Foot motions in the three axes of rotation are illustrated in Figure 6-8 and summarized in Table 6-1.
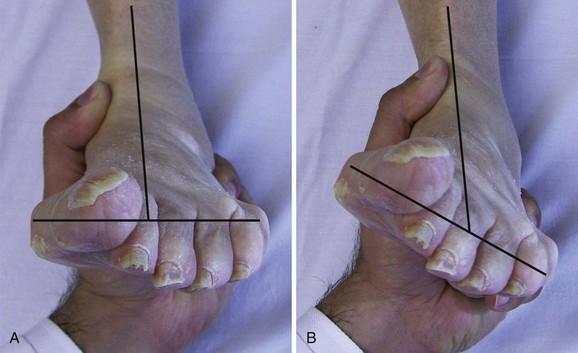
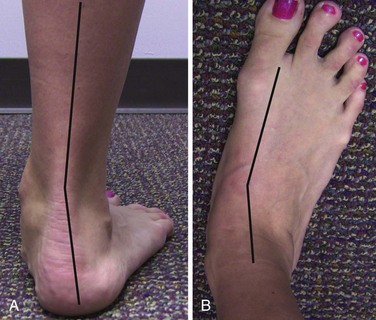
1. The critical assessment is to determine the relationship of the forefoot to the hindfoot.
2. If the heel is in a neutral position (subtalar neutral), the forefoot should be parallel with the floor to meet the ground flush (plantigrade).
 If the first ray is elevated, the forefoot is in varus position. If the first ray is flexed, the forefoot is in valgus position. This should not be confused with hindfoot varus or valgus.
If the first ray is elevated, the forefoot is in varus position. If the first ray is flexed, the forefoot is in valgus position. This should not be confused with hindfoot varus or valgus.
 For example, in a long-standing flatfoot deformity the heel is valgus and the forefoot has compensated by going into varus or supinating to keep the flat to the ground.
For example, in a long-standing flatfoot deformity the heel is valgus and the forefoot has compensated by going into varus or supinating to keep the flat to the ground.
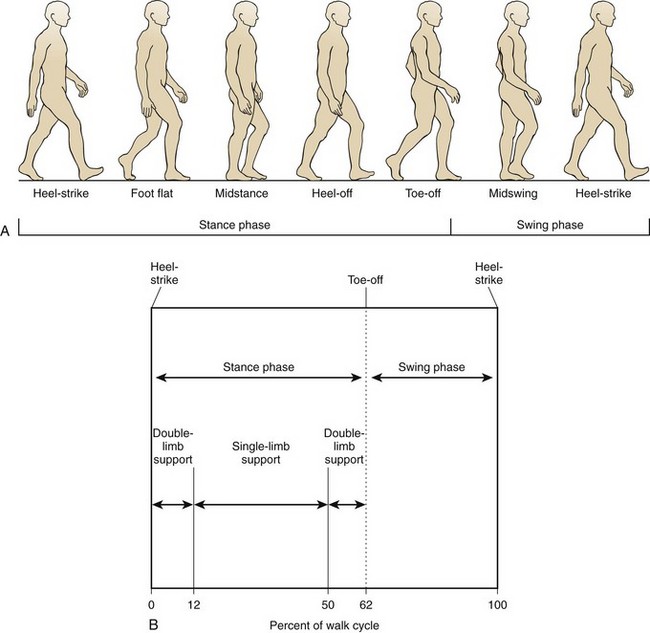
A One full gait cycle, from heel-strike to heel-strike, is termed a “stride.”
1. Each stride is composed of a stance phase (heel-strike to toe-off, 62% of the cycle) and a swing phase (toe-off to heel-strike, 38% of the cycle) (Figure 6-10).
2. Walking is defined by a period of double-limb support in addition to always having one foot in contact with the ground throughout the gait cycle.
3. Ground reaction forces are approximately 1.5 times body weight during walking and 3 to 4 times body weight during running.
 This difference is due to the increased load after the float phase of running, in which there is no foot in contact with the ground.
This difference is due to the increased load after the float phase of running, in which there is no foot in contact with the ground.
4. As the speed of gait increases, the stance phase decreases.
B Soft tissue contributions to gait mechanics
 Gastrocnemius-soleus complex—concentric contraction
Gastrocnemius-soleus complex—concentric contraction
 In addition, as the foot progresses from heel-strike to toe-off, the following changes allow the foot to convert from a flexible shock absorber to a rigid propellant.
In addition, as the foot progresses from heel-strike to toe-off, the following changes allow the foot to convert from a flexible shock absorber to a rigid propellant.
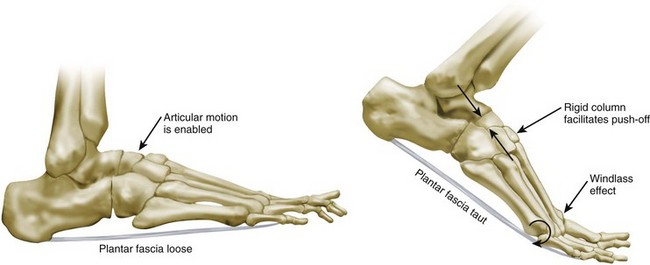
 The plantar fascia, which attaches to the plantar medial heel and runs the length of the arch to the bases of each proximal phalanx, is tightened as the MTP joints extend. The longitudinal arch is accentuated.
The plantar fascia, which attaches to the plantar medial heel and runs the length of the arch to the bases of each proximal phalanx, is tightened as the MTP joints extend. The longitudinal arch is accentuated.
 The hindfoot supinates, with firing of the posterior tibial tendon.
The hindfoot supinates, with firing of the posterior tibial tendon.
 The transverse tarsal joint locks and provides a rigid lever arm for toe-off.
The transverse tarsal joint locks and provides a rigid lever arm for toe-off.
section 2 Physical Examination of the Foot and Ankle
A The foot and ankle should be inspected for
2. Callouses—areas of abnormally increased pressure
3. Signs of peripheral vascular disease—lack of hair, increased skin pigmentation (hemosiderin deposition)
4. Swelling—symmetric (likely systemic etiology) versus asymmetric (trauma, venous thrombosis, cellulitis, osteomyelitis, focal musculoskeletal etiology) (Figure 6-12)
5. Ecchymosis—plantar ecchymosis associated with tarsometatarsal injury (Lisfranc injury) (Figure 6-13)
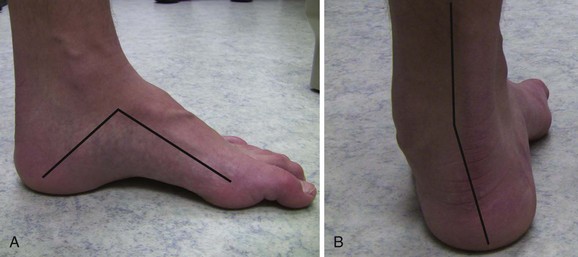
 Cavovarus—elevated longitudinal arch with hindfoot varus and plantar-flexed first ray (Figure 6-14)
Cavovarus—elevated longitudinal arch with hindfoot varus and plantar-flexed first ray (Figure 6-14)
 Pes planus—flat longitudinal arch with hindfoot valgus (Figure 6-15)
Pes planus—flat longitudinal arch with hindfoot valgus (Figure 6-15)
A Palpate the dorsalis pedis and posterior tibial pulses. If they are not present, consider noninvasive studies.
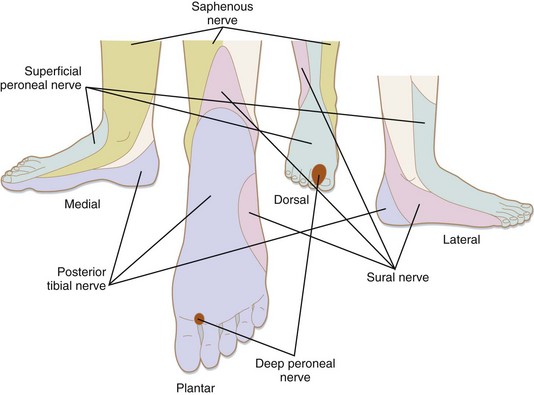
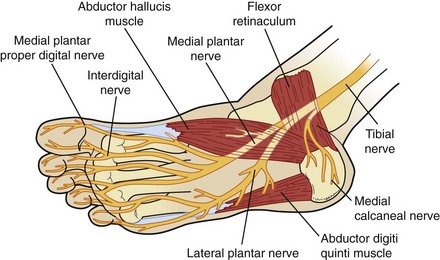
A The sensory examination should assess the following five cutaneous nerves that supply the feet (Figure 6-17).
1. Saphenous—medial ankle and hindfoot
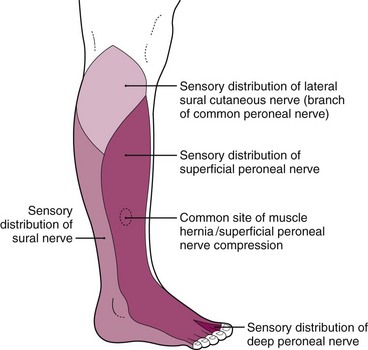
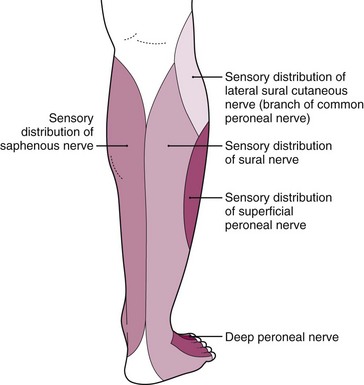
2. Superficial peroneal (Figure 6-18)
3. Deep peroneal—first dorsal web space
4. Sural—posterolateral border of the leg and the lateral border of the foot (Figure 6-19)
B Inability to sense a Semmes-Weinstein 5.07 monofilament is consistent with neuropathy.
A When assessing strength, keep in mind the relation the tendon has to the axis of the ankle. For example, if it passes medially and posteriorly, the function of that structure will be to provide plantar flexion and inversion (tibialis posterior).
B When assessing motor function of the foot and ankle, the following muscles should be tested.
1. Tibialis anterior—ankle dorsiflexion, L3-4
2. Extensor hallucis longus—great-toe extension, L4-5
3. Peroneus longus and brevis—hindfoot eversion, L5-S1
C It is important to remember that neurologic deficits can be secondary to more proximal pathology (e.g., central nervous system, spinal cord, nerve root).
A Palpation of the tendinous and bony anatomy of the foot and ankle is facilitated by its subcutaneous nature. A detailed examination can typically reproduce the patient’s source of pain, allowing the examiner to identify the cause without the need for supplementary studies.
B The courses of all tendons are checked both at rest and during contraction for swelling, nodules, and subluxation.
C A Tinel sign should be sought for
1. Tibial nerve at the tarsal tunnel
2. Superficial peroneal nerve as it exits the fascia of the lateral compartment (anterolateral leg)
3. Deep peroneal nerve (anterior tarsal tunnel syndrome) at the anterior ankle and hindfoot; may be compressed at the inferior extensor retinaculum
D The web space can be palpated for evidence of interdigital neuromas with an associated Mulder sign.
1. With dorsal pressure applied to the web space, the metatarsal heads are compressed with the contralateral hand. An audible click, along with radiating pain into the affected toes, is a positive sign.
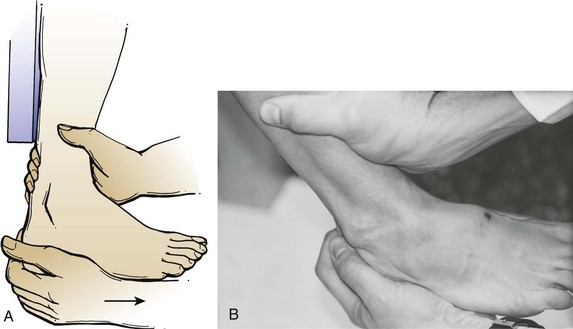
E Stability of the lateral ankle ligaments can be assessed with the anterior drawer and varus talar tilt tests (Figure 6-21).
A Both passive and active range of motion (ROM) should be compared with the contralateral side.
B There is a high rate of variability of normal motion of the joints of the foot and ankle, with no defined absolute normal.
C Range of motion that is limited to the contralateral side or is painful is abnormal.
D Increased ROM, specifically ankle dorsiflexion, is critical to identify because that can be associated with an Achilles tendon rupture.
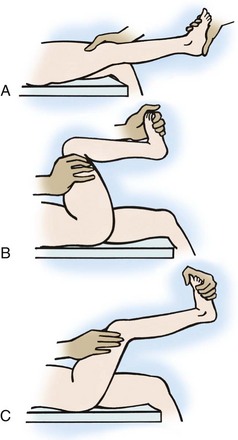
E Silfverskiöld test (difference in ankle dorsiflexion with knee flexed versus extended) can help differentiate between gastrocnemius and Achilles contracture (Figure 6-22).
section 3 Radiographic Evaluation of the Foot and Ankle
I WEIGHT-BEARING VIEWS—should be obtained when possible
A The standard views of the ankle are
3. Mortise (a view of 15 degrees of internal rotation along the transmalleolar axis)
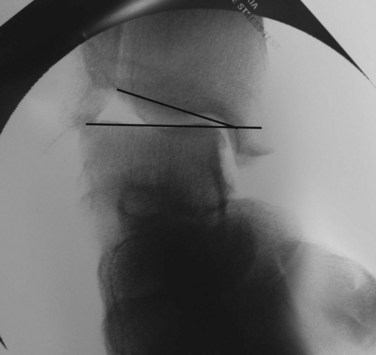
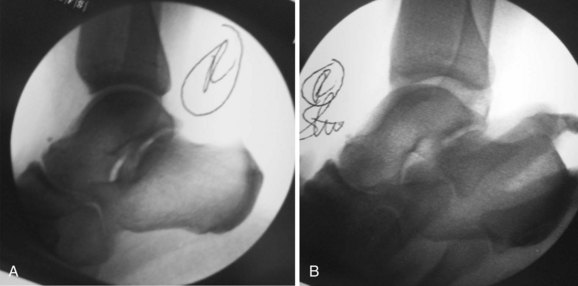
4. Gravity or manual external rotation stress is critical in the evaluation of suspected deltoid ligament (supination–external rotation stage IV [SER IV]) and syndesmotic injuries (Figure 6-23).
5. Anterior drawer and talar tilt views are helpful in cases of suspected ankle instability (Figures 6-24 and 6-25).
B Special views are provided when the clinical presentation warrants it (Table 6-2).
Table 6-2
Special Radiographic Views of the Foot and Ankle
| View | Specific Purpose |
| Canale view—15-degree internal rotation for foot | Talar neck view for fracture |
| Harris view—axial heel view | Calcaneus fractures |
| Sesamoid view—axial sesamoid view | Sesamoid fracture or arthritis |
| Broden view—tibiocalcaneal (subtalar) medial oblique views at 10-degree variations | Posterior, medial, and anterior facets of subtalar joint for fracture or arthritis |
C Comparison views of the contralateral foot or ankle are not routinely ordered but can be helpful.
A Computed tomography (CT) of the foot and ankle is especially useful for complex fractures (pilon, calcaneus, talus, midfoot, Lisfranc) and tarsal coalition.
B Magnetic resonance imaging (MRI) aids the evaluation of osteochondral defects, osteonecrosis, neoplasm, and other soft tissue pathologies.
C Bone scans are sensitive for the identification of stress fractures.
D Indium-tagged white blood cell (WBC) scans are both sensitive and specific in the detection of osteomyelitis.
section 4 Adult Hallux Valgus
A Hallux valgus is defined as a lateral deviation of great toe with medial deviation of first metatarsal.
B The pathophysiology of hallux valgus is likely multifactorial.
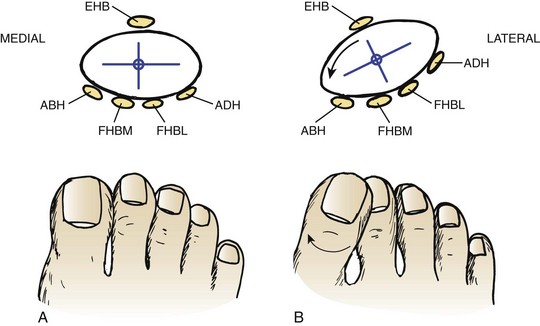
B Proximal phalanx drifts laterally, leading to the following conditions:
1. Plantar-lateral migration of abductor hallucis; change in position causes the muscle to plantarflex and pronate the phalanx.
2. Stretching of the extensor hood of the extensor hallucis longus
3. Lateral deviation of the extensor hallucis longus and flexor hallucis longus (FHL), causing a muscular imbalance and deforming force for valgus progression and pronation of the great toe (Figure 6-27)
C First metatarsal head moves medially off the sesamoids, increasing the intermetatarsal angle (IMA).
D Secondary contracture of the lateral capsule, adductor hallucis, lateral metatarsal-sesamoid ligament, and intermetatarsal ligament
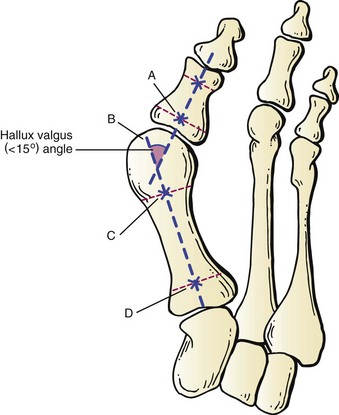
1. Multiple measurements can be obtained from standard radiographs that guide treatment options.
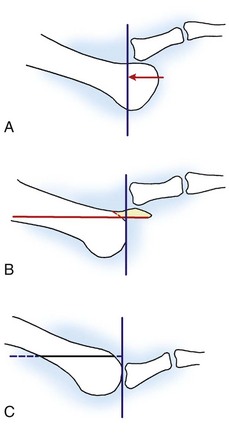
 Hallux valgus angle (HVA)—angle formed by line along first metatarsal shaft and line along shaft of proximal phalanx (Figure 6-28)
Hallux valgus angle (HVA)—angle formed by line along first metatarsal shaft and line along shaft of proximal phalanx (Figure 6-28)
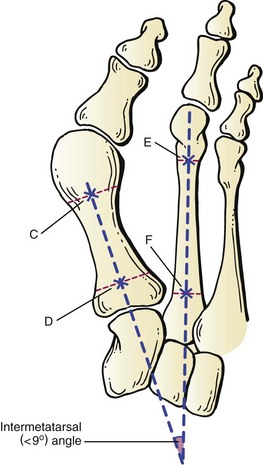
 First-second IMA—angle formed by line along first metatarsal shaft and line along second metatarsal shaft (Figure 6-29)
First-second IMA—angle formed by line along first metatarsal shaft and line along second metatarsal shaft (Figure 6-29)
 Hallux valgus interphalangeus (HVI) angle—angle formed by line along shaft of proximal phalanx and line along shaft of distal phalanx (Figure 6-30)
Hallux valgus interphalangeus (HVI) angle—angle formed by line along shaft of proximal phalanx and line along shaft of distal phalanx (Figure 6-30)
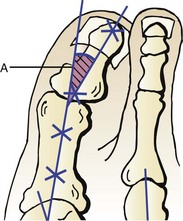
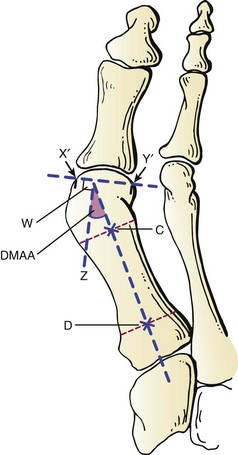
 Distal metatarsal articular angle (DMAA)—angle formed by line along the articular surface of the first metatarsal and line perpendicular to axis of the first metatarsal (Figure 6-31)
Distal metatarsal articular angle (DMAA)—angle formed by line along the articular surface of the first metatarsal and line perpendicular to axis of the first metatarsal (Figure 6-31)
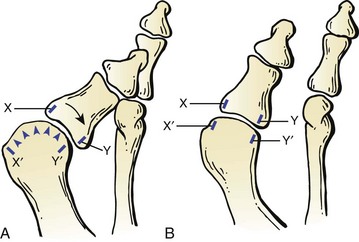
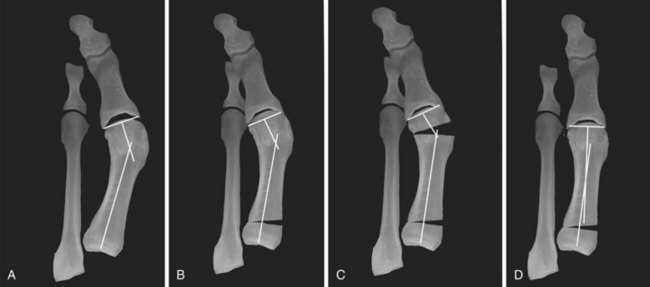
2. The congruency of the first MTP joint should be determined (Figure 6-32).
 Congruency is determined by comparing the line connecting the medial and lateral edge of the first metatarsal head articular surface with the similar line for the proximal phalanx.
Congruency is determined by comparing the line connecting the medial and lateral edge of the first metatarsal head articular surface with the similar line for the proximal phalanx.
3. The position of the sesamoids should be noted. In more severe or chronic deformities, the sesamoids are frequently displaced laterally.
4. Presence of first MTP joint and first metatarso-cuneiform joint degenerative changes should be noted.
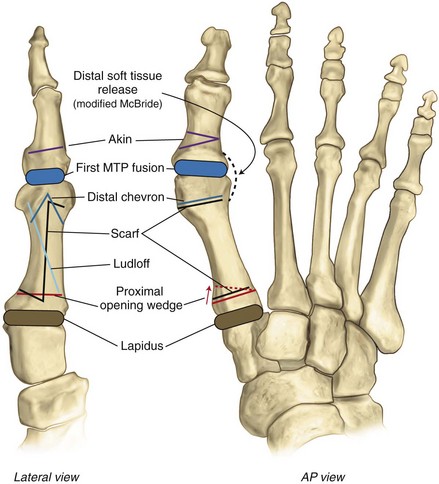
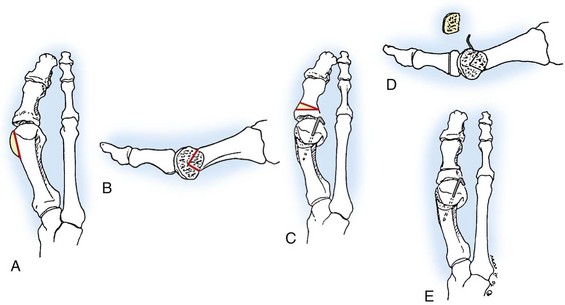
III SURGICAL PROCEDURES (Figure 6-33)
A The appropriate surgical procedure is dictated by the abnormal radiographic angular measurements in concordance with underlying clinical abnormalities.
1. The patient’s physical examination and associated pathology dictates the appropriate surgical procedure regardless of the angular measurements.
 MTP fusion required—The IMA will correct with realignment of the first MTP; concomitant metatarsal osteotomy is NOT required (Figure 6-34).
MTP fusion required—The IMA will correct with realignment of the first MTP; concomitant metatarsal osteotomy is NOT required (Figure 6-34).
 Lapidus (first tarsometatarsal realignment arthrodesis) required
Lapidus (first tarsometatarsal realignment arthrodesis) required
2. Procedures never appropriate in isolation (high recurrence rate)
 Distal soft tissue release (modified McBride)
Distal soft tissue release (modified McBride)
 Isolated osteotomy without associated soft tissue correction
Isolated osteotomy without associated soft tissue correction
3. Algorithmic approach to identifying the appropriate surgical intervention (Box 6-1)
 All patients should undergo a soft tissue release with all associated osteotomies and first TMT arthrodesis (Lapidus).
All patients should undergo a soft tissue release with all associated osteotomies and first TMT arthrodesis (Lapidus).
 IMA is 13 degrees or less, AND HVA is 40 degrees or less.
IMA is 13 degrees or less, AND HVA is 40 degrees or less.
 IMA is greater than 13 degrees, OR HVA is greater than 40 degrees.
IMA is greater than 13 degrees, OR HVA is greater than 40 degrees.
 Instability of the first TMT/joint laxity
Instability of the first TMT/joint laxity
 Distal medial closed-wedge metatarsal osteotomy in addition to what is required based on the angular measurements (Figure 6-36)
Distal medial closed-wedge metatarsal osteotomy in addition to what is required based on the angular measurements (Figure 6-36)
section 5 Juvenile and Adolescent Hallux Valgus
A Several critical factors separate these patients from adult patients with hallux valgus deformity.
B Recurrence of the deformity after surgical correction is the most common complication (Figure 6-38).
C Proximal osteotomy is performed through the medial cuneiform in patients with an open first metatarsal physis.
1. If arthrodesis of the first TMT is required for laxity, surgical intervention is delayed until physeal closure.
D The deformity is secondary to underlying bony and ligamentous anatomy that must be addressed to prevent recurrence.
1. Varus of the first metatarsal with a large IMA is commonly present.
2. DMAA is typically increased.
4. Ligamentous laxity may be present, and a history of Ehlers-Danlos or Marfan syndrome should be elicited.
5. The family history is frequently positive for hallux valgus.
1. Single, double, or triple osteotomies are required to correct the deformity, applying the same principles as described for the evaluation of adult hallux valgus.
2. In cases of ligamentous laxity—A first TMT arthrodesis substitutes for a proximal osteotomy to correct the IMA. The first metatarsal physeal plate must be closed.
section 6 Hallux Varus
A Medial deviation of the great toe is most often an iatrogenic deformity secondary to overcorrection of hallux valgus.
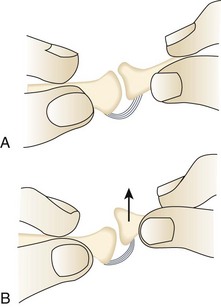
A Dependent upon if the deformity is flexible (reducible) or rigid (irreducible)
B Flexible deformity can be corrected with a soft tissue procedure.
1. Release of the abductor hallucis muscle and fascia
2. Transfer of a portion of the extensor hallucis longus (EHL) or brevis tendon under the transverse intermetatarsal ligament to the distal metatarsal neck (taken from lateral to medial) (Figure 6-40)
C Fixed deformity or a deformity with limited first MTP motion is treated with a first MTP arthrodesis.
section 7 Lesser-Toe Deformities
A Static stability of the lesser toes is provided by the congruency of the MTP and interphalangeal joints.
1. The plantar plate, which comprises the plantar aponeurosis and capsule, provides a soft tissue block to metatarsal head depression and prevents hyperextension of the MTP joint.
2. Persistent hyperextension at the MTP joint may lead to attenuation and weakening of the plantar structures.
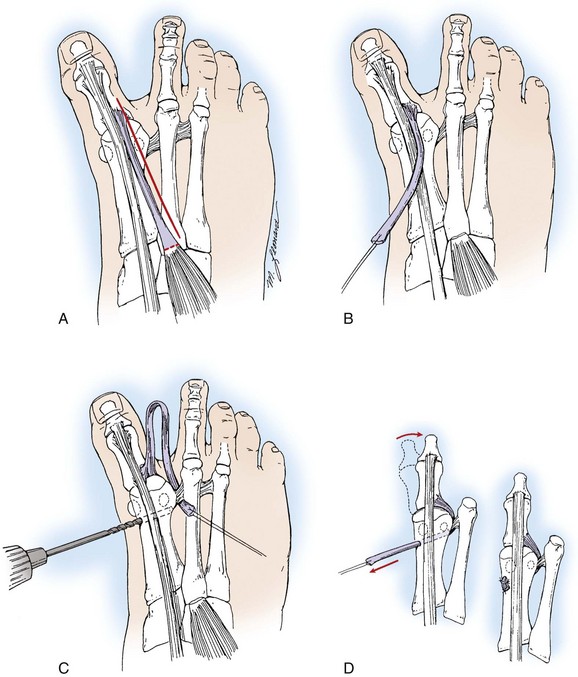
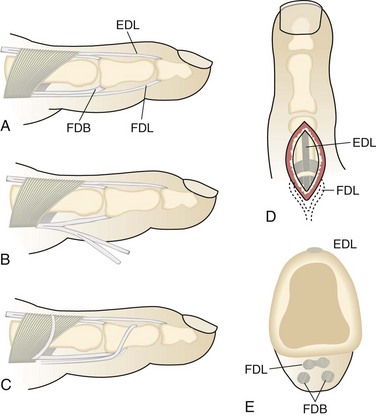
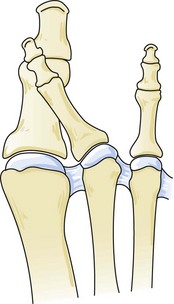
B Dynamic stability is provided by the various tendons that insert on the lesser toes (Figure 6-41).
1. The EDL is the primary extensor of the MTP joint.
 The tendon runs through a sling over the dorsal surface of the MTP joint before splitting into a central slip that inserts on the middle phalanx and two dorsolateral slips that reconverge to insert at the base of the distal phalanx.
The tendon runs through a sling over the dorsal surface of the MTP joint before splitting into a central slip that inserts on the middle phalanx and two dorsolateral slips that reconverge to insert at the base of the distal phalanx.
 The distal extensor effect of the EDL is neutralized when the proximal phalanx is dorsiflexed, as in hammer-toe or claw-toe deformities.
The distal extensor effect of the EDL is neutralized when the proximal phalanx is dorsiflexed, as in hammer-toe or claw-toe deformities.
2. The extensor digitorum brevis extends the PIP joints and inserts on the lateral aspect of the EDL tendon on all but the fifth toe.
3. The FDL is the primary plantar flexor of the distal interphalangeal (DIP) joints because it inserts on the plantar aspect of the distal phalanges. It also weakly plantar flexes the MTP joints.
4. The flexor digitorum brevis splits at the level of the MTP joint and inserts on the plantar lateral aspects of the middle phalanges. The flexor digitorum brevis is the primary plantar flexor of the PIP joints.
5. The intrinsic muscles of the foot include the lumbricals, which originate from the FDL tendon and insert on the extensor sheath over the MTP joints, and four dorsal and three plantar interossei muscles, which insert on the medial aspect of the proximal phalanges.
C The extrinsic muscles (EDL and FDL) overpower the intrinsic muscles in positioning the lesser toes in hammer- and claw-toe deformities, with the EDL driving MTP joint extension and the FDL driving PIP and DIP joint flexion.
D The EDL also is a weak antagonist to flexion at the interphalangeal joints, and likewise the FDL is a weak antagonist to extension at the MTP joint.
E Dorsiflexion of the proximal phalanx at the MTP joint neutralizes these weak antagonist effects and accentuates the developing deformity.
F Lesser-toe deformities occur much more commonly in women (up to 5 : 1 ratio), thought to be secondary to wearing high-fashion shoes that constrict the forefoot and maintain the MTP joints in hyperextension.
1. A hammer deformity most commonly involves the second toe because of its relative length compared to the remainder of the lesser toes. A short toe box will cause the second toe to buckle and extend at the MTP joint.
2. Chronic positioning of the MTP joint in hyperextension will attenuate the static plantar structures, allowing depression of the metatarsal head, migration of the fat pad distally, and imbalance of the dynamic forces on the toe as described above.
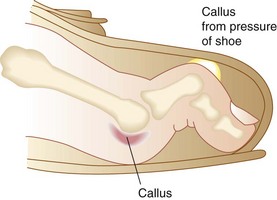
A The characteristic hammer-toe deformity is flexion of the PIP joint. With weight bearing, the MTP joint will appear dorsiflexed; however, this should correct with elevation of the foot off the ground (Figure 6-42).
B The term “complex” hammer toe refers to concomitant dorsiflexion of the MTP joint that does not correct and is more appropriately termed and treated as a claw toe.
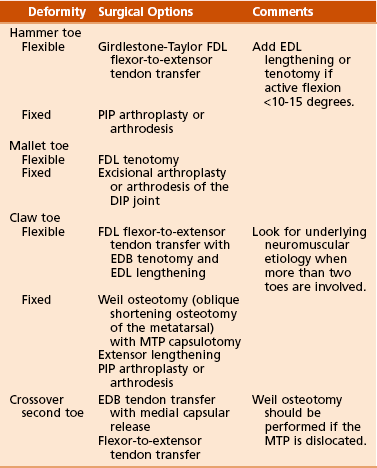
C Treatment is dependent upon the flexibility of the deformity (Table 6-3).
 Nonoperative—Protective padding, shoes with tall toe boxes, and corrective hammer-toe splints are effective.
Nonoperative—Protective padding, shoes with tall toe boxes, and corrective hammer-toe splints are effective.
 Operative—flexor tenotomy or flexor-to-extensor tendon transfer
Operative—flexor tenotomy or flexor-to-extensor tendon transfer
III CLAW-TOE DEFORMITY (INTRINSIC MINUS TOE)
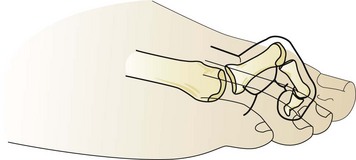
A Characterized by flexion of the PIP and DIP joints in the setting of fixed hyperextension of the MTP joint (Figure 6-44)
1. Clawing typically involves multiple toes and is often bilateral.
2. Cavus deformity, neuromuscular diseases that affect the balance of the extrinsic and intrinsic musculature, inflammatory arthropathies that lead to attenuation of soft tissue structures and instability of the MTP joint, and trauma have all been implicated in the etiology of claw toes.
3. Claw toes are a noted complication of compartment syndrome involving the deep compartments of the foot.
B Treatment is dependent upon the flexibility of the deformity (see Table 6-3).
 Nonoperative—shoe modification, padding over any prominent or painful callosities, and use of orthotics to off-load and support a potentially painful, plantarly subluxed metatarsal head
Nonoperative—shoe modification, padding over any prominent or painful callosities, and use of orthotics to off-load and support a potentially painful, plantarly subluxed metatarsal head
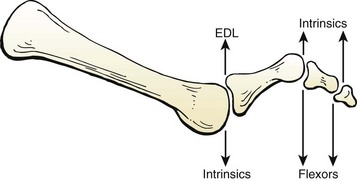
 Operative—Flexor-to-extensor tendon transfer of the FDL alters the function of the FDL to function as an intrinsic and maintain correction (Figure 6-45). Lengthening of the EDL and extensor digitorum brevis is typically required.
Operative—Flexor-to-extensor tendon transfer of the FDL alters the function of the FDL to function as an intrinsic and maintain correction (Figure 6-45). Lengthening of the EDL and extensor digitorum brevis is typically required.
 Nonoperative—shoe modification, padding over any prominent or painful callosities, and use of orthotics to off-load and support a potentially painful, plantarly subluxed metatarsal head
Nonoperative—shoe modification, padding over any prominent or painful callosities, and use of orthotics to off-load and support a potentially painful, plantarly subluxed metatarsal head
 Operative—PIP arthroplasty or arthrodesis along with MTP joint capsulotomy and extensor lengthening
Operative—PIP arthroplasty or arthrodesis along with MTP joint capsulotomy and extensor lengthening
A A mallet toe consists of an isolated flexion deformity at the DIP joint (Figure 6-47).
V CROSSOVER-TOE DEFORMITY (see Table 6-3)
A Multiplanar instability of the second toe may cause the toe to lie dorsomedially relative to the hallux (Figure 6-48).
B Commonly referred to as a crossover second toe, this deformity
1. Requires disruption of the plantar plate—KEY component
2. Requires attenuation of the lateral collateral ligament
3. May be iatrogenic—caused by steroid injection within the MTP joint—results in plantar plate attenuation
VI METATARSOPHALANGEAL INSTABILITY
A Mild subluxation of the MTP joint that presents with pain and swelling without any deformity. Drawer test results in pain within the joint (Figure 6-49).
A Osteochondrosis of one of the lesser metatarsals, most commonly involving the second metatarsal
B Patients have pain localized over the affected metatarsal head.
1. The second metatarsal is affected in over two thirds of cases. The third metatarsal accounts for most of the remaining cases. The fourth is affected in less than 5% of cases. The first and fifth metatarsals are rarely affected.
2. The pain is worse with ambulation and activities. It is relieved with sitting.
C Common radiographic findings in Freiberg disease include
1. Resorption of the central metatarsal bone adjacent to the articular surface with flattening of the metatarsal head (Figure 6-50)
3. Joint space narrowing in late-stage disease with associated osteophyte formation along with collapse of the articular surface (Figure 6-51)
1. Common strategies consist of activity modification, shoe-wear modification (hard sole), orthotics (metatarsal bar), and a period of protected weight bearing.
1. For early-stage disease, joint débridement should be considered.
 All synovitis, osteophytes, and loose bodies are débrided through a dorsal incision.
All synovitis, osteophytes, and loose bodies are débrided through a dorsal incision.
 This should be considered for patients with relatively good articular surface congruity and minimal metatarsal deformity.
This should be considered for patients with relatively good articular surface congruity and minimal metatarsal deformity.
2. Many studies have reported good results with dorsal closed-wedge metaphyseal osteotomy of the affected metatarsal (Figure 6-52).
 This is done in conjunction with a thorough débridement of synovitis, abnormal cartilage, osteophytes, and necrotic bone.
This is done in conjunction with a thorough débridement of synovitis, abnormal cartilage, osteophytes, and necrotic bone.
 This osteotomy serves to rotate the plantar aspect of the articular surface, which is typically well preserved, to a more superior position, where it then articulates with the phalanx.
This osteotomy serves to rotate the plantar aspect of the articular surface, which is typically well preserved, to a more superior position, where it then articulates with the phalanx.
A Several types of deformity exist, including underlapping, overlapping, rotatory, and cock-up fifth toe.
B Subluxation at the fifth MTP results in weakened push-off during ambulation, a loss of coverage of the fifth metatarsal head, and subsequent callus formation under the dorsolateral aspect of the fifth toe.
1. Stretching or taping may be helpful with an overlapping fifth toe, along with wide–toe box shoes.
 EDL transfer into the abductor digiti minimi with rerouting inferior to the phalanx
EDL transfer into the abductor digiti minimi with rerouting inferior to the phalanx
 Release of the dorsomedial capsule and Z-plasty of the skin may be required.
Release of the dorsomedial capsule and Z-plasty of the skin may be required.
2. Congenital curly toe (underlapping)
 Tenotomy of FDL and flexor digitorum brevis has been recommended in children with flexible deformities.
Tenotomy of FDL and flexor digitorum brevis has been recommended in children with flexible deformities.
3. Syndactylization is reserved for salvage after failed operative intervention.
section 8 Hyperkeratotic Pathologies
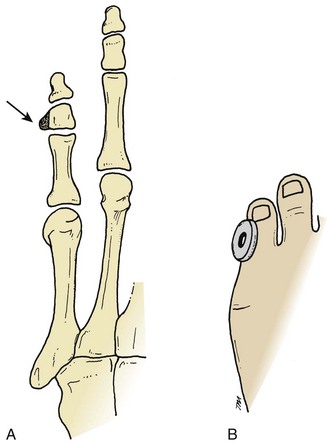
1. Commonly occur over the metaphyseal aspect of the phalanges at the metatarsophalangeal or interphalangeal joints, especially of the fifth toe
2. Secondary to frictional irritation or from pressure over bony prominences (Figure 6-53)
3. Examination reveals epidermal hyperplasia with a conical central area.
II SOFT CORNS (HELOMATA MOLLE)
1. Hyperkeratoses that develop as the result of moisture in web space and pressure from neighboring phalangeal condyles (Figure 6-54)
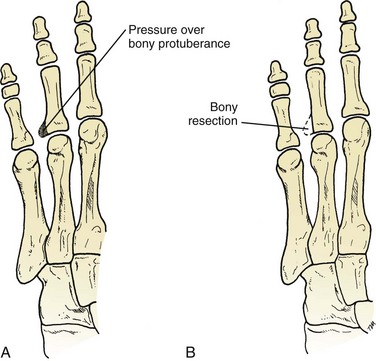
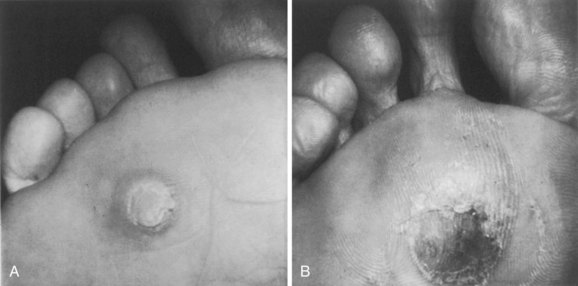
III INTRACTABLE PLANTAR KERATOSIS
A Plantar callus secondary to excess pressure from metatarsal head
B Predisposing factors—fat pad atrophy, plantar-flexed first ray, equinus contracture, intrinsic minus toe contracture, and hypertrophy of the sesamoid
C Two main types (Figure 6-55)
 Localized callus with a hyperkeratotic core, usually caused by prominence of fibular condyle
Localized callus with a hyperkeratotic core, usually caused by prominence of fibular condyle
IV BUNIONETTE DEFORMITY (TAILOR’S BUNION)
1. Prominence over the distal aspect of the fifth metatarsal head
2. Causes pain over the lateral or plantar aspect of the MTP joint, particularly with compressive shoe wear
3. Bunionette deformity in conjunction with ipsilateral hallux valgus and metatarsus primus varus is termed “splayfoot.”
4. Three distinct types have been described based on the anatomic location of the deformity along the fifth metatarsal.
 Type I deformity—distinguished by the presence of an enlarged fifth metatarsal head (Figure 6-56)
Type I deformity—distinguished by the presence of an enlarged fifth metatarsal head (Figure 6-56)
 Type II deformity—demonstrates lateral bowing of the fifth metatarsal diaphysis (Figure 6-57)
Type II deformity—demonstrates lateral bowing of the fifth metatarsal diaphysis (Figure 6-57)
 Type III deformity—demonstrates an abnormally widened fourth-fifth metatarsal angle (intermetatarsal angle >8 degrees) (Figure 6-58)
Type III deformity—demonstrates an abnormally widened fourth-fifth metatarsal angle (intermetatarsal angle >8 degrees) (Figure 6-58)
1. Shoe-wear modification, strategic padding, and shaving the symptomatic callus is usually effective.
2. With plantar callus or associated pes planus, consider a metatarsal pad or custom orthotic device.
1. Lateral metatarsal head condylectomy (type I)
2. Distal fifth metatarsal osteotomy (i.e., chevron) (type II)
3. Oblique diaphyseal osteotomy (type III)
4. Consider metatarsal head resection for salvage.
5. Proximal osteotomy should be avoided owing to the tenuous blood supply at the proximal metadiaphyseal junction of the fifth metatarsal.
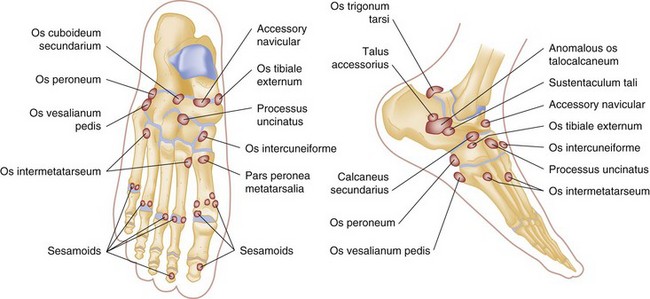
section 9 Sesamoids
A The medial (tibial) and lateral (fibular) hallucal sesamoids are part of a strong sesamoid capsuloligamentous complex.
1. Enveloped within the two heads of the flexor hallucis brevis tendon, separated by an intersesamoid ridge called the crista
2. Attached to proximal phalanx via the plantar plate
3. Suspended by the collateral ligaments of MTP joint, metatarsosesamoid ligaments, intersesamoid ligament, abductor hallucis tendon, and adductor hallucis tendon
B Analogous to the patella, as a mechanism to increase the mechanical advantage of the pulley function of the intrinsics (flexor hallucis brevis)
C Protects the FHL and disperses the forces beneath the first metatarsal head
A Sesamoid disorders can include acute injury (fracture, dislocation, sprain/“turf toe”), sesamoiditis, stress fracture, arthrosis, avascular necrosis, and intractable plantar keratosis.
1. Chief complaint is pain under the first metatarsal head, especially with toe-off.
2. Physical examination—tenderness with direct palpation of the involved sesamoid, pain with first MTP ROM
3. Radiographs—in addition to anteroposterior and lateral views, lateral oblique (fibular sesamoid) and medial oblique (tibial sesamoid) views isolate each bone, and the axial view shows the articulation with the metatarsal head (Figure 6-59).
4. Mechanism of injury—forced dorsiflexion of the first MTP joint, repetitive loading
 Signs—normal ROM, weight bearing without difficulty, normal radiographs
Signs—normal ROM, weight bearing without difficulty, normal radiographs
 Treatment—stiff insole, taping, with immediate return to play
Treatment—stiff insole, taping, with immediate return to play
 Initial treatment with a fracture boot to limit the stress across the sesamoid
Initial treatment with a fracture boot to limit the stress across the sesamoid
 Transition to sesamoid relief pad (dancer’s pad) with gradual resumption of activity
Transition to sesamoid relief pad (dancer’s pad) with gradual resumption of activity
3. Sesamoiditis can be treated with anti-inflammatory medications, rest, ice, and activity and shoe-wear modification.
1. Symptomatic nonunions or cases that prove refractory to conservative care can be treated surgically with bone grafting or with partial or complete sesamoidectomy.
2. The results of sesamoidectomy are the most predictable.
 Excision of the proximal or distal pole achieves the best results and should be performed if the fracture pattern allows.
Excision of the proximal or distal pole achieves the best results and should be performed if the fracture pattern allows.
3. Complications of medial and lateral sesamoidectomy are hallux valgus and varus, respectively.
 Repairing the defect with capsule (or a slip of abductor hallucis for the tibial sesamoid) should help prevent this complication.
Repairing the defect with capsule (or a slip of abductor hallucis for the tibial sesamoid) should help prevent this complication.
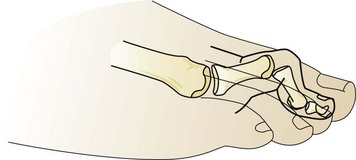
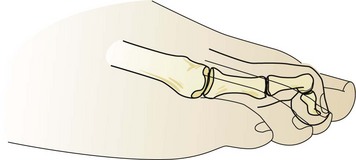
 Cock-up deformity (or claw toe) will occur if both sesamoids are excised (Figure 6-60).
Cock-up deformity (or claw toe) will occur if both sesamoids are excised (Figure 6-60).
 Care should be taken to avoid injury to the FHL and loss of flexor function, especially in the high-performance athlete.
Care should be taken to avoid injury to the FHL and loss of flexor function, especially in the high-performance athlete.