32
Disorders of Eccrine and Apocrine Glands
Eccrine and apocrine glands represent the two major types of sweat glands (see Fig. 91.1).
Eccrine Glands
Apocrine Glands
Hyperhidrosis
• Excessive production of eccrine sweat is usually due to primary cortical (emotional) hyperhidrosis and the favored sites are the axillae or palms and soles (Fig. 32.1) > the face (Fig. 32.2); involvement is bilateral and symmetric.

Fig. 32.1 Volar hyperhidrosis (primary cortical). The palmoplantar skin displays excessive eccrine sweat production, including the portions that extend onto the sides of the hands, feet, and digits. Its onset is during childhood as opposed to axillary hyperhidrosis, which has its onset around puberty.

Fig. 32.2 Primary cortical (emotional) hyperhidrosis involving the face. Sweat droplets are evident on the upper cutaneous lip, jawline, and chin. Reproduced from Hurley HJ. Hyperhidrosis. Curr. Opin. Dermatol. 1997;4:105–114. Philadelphia: Rapid Science Publishers.
• Secondary hypothalamic (thermoregulatory) hyperhidrosis can be due to a number of systemic diseases, from infections to neoplasms (Table 32.1).
Table 32.1
Causes of secondary hypothalamic hyperhidrosis.
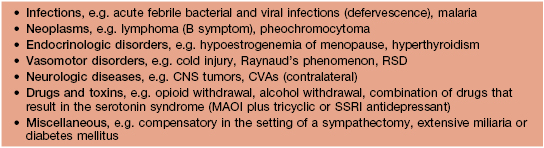
CNS, central nervous system; CVA, cerebrovascular accident; MAOI, monoamine oxidase inhibitor; RSD, reflex sympathetic dystrophy, also referred to as complex regional pain syndrome; SSRI, selective serotonin reuptake inhibitor. Linezolid is an MAOI.
• Secondary medullary (gustatory) hyperhidrosis can be physiologic as exemplified by the facial sweating that occurs with spicy foods or pathologic as occurs in Frey’s syndrome (Fig. 32.3); in the former, taste receptors send afferent impulses, whereas in the latter, disrupted nerves for sweat aberrantly connect with nerves for salivation.

Fig. 32.3 Gustatory sweating in the auriculotemporal (Frey’s) syndrome, as a consequence of parotid surgery. The blue-black area represents sweating (starch–iodine technique). Salivary stimulation induced this sweating response. Reproduced from Hurley HJ. Hyperhidrosis. Curr. Opin. Dermatol. 1997;4:105–114. Philadelphia: Rapid Science Publishers.
• Injuries or diseases affecting the spinal cord can result in segmental hyperhidrosis.
• Injection of botulinum toxin type A every ~6 months is very effective for primary cortical (emotional) hyperhidrosis (Fig. 32.4); tap water iontophoresis is less effective.

Fig. 32.4 Delineation of area for injections of botulinum toxin A for axillary hyperhidrosis (starch–iodine technique). Blue-black areas represent foci of sweating. In the case of onabotulinumtoxin A, a total of 50–100 U is injected, utilizing 10–15 injection sites. Courtesy, Alastair Carruthers, MD, and Jean Carruthers, MD.
Hypohidrosis (and Anhidrosis)
• There are multiple etiologies of hypohidrosis and anhidrosis including the following:
– Manifestation of inherited disorders, in particular ectodermal dysplasias (see Chapter 52), as well as acquired disorders such as Sjögren’s syndrome.
• Increased risk of developing hyperthermia.
• Evaluation includes colorimetric testing (see Fig. 32.4) and biopsy of affected skin.
Bromhidrosis (Foul-Smelling Sweat)
Chromhidrosis
Sweat Retention Disorders
Miliaria
• Classically divided into three major types: (1) crystallina – tiny, superficial, short-lived, clear vesicles (Fig. 32.5A; see Fig. 28.3); (2) rubra (prickly heat) – pruritic erythematous papulovesicles and occasionally pustules that favor the upper trunk (Fig. 32.5B); and (3) profunda – white papules due to excessive sweating in a hot climate (rare); these three forms reflect ductal occlusion within the stratum corneum, mid-epidermis, and dermal–epidermal junction, respectively.


Fig. 32.5 A Miliaria crystallina. Multiple small superficial vesicles with clear fluid. B Miliaria rubra. Multiple erythematous nonfollicular papules and papulovesicles on the back.
• If extensive, decrease in eccrine function can give rise to hyperpyrexia.
• DDx: miliaria rubra needs to be distinguished from folliculitis, Grover’s disease, neutrophilic eccrine hidradenitis, and cutaneous candidiasis.
Fox–Fordyce Disease (Apocrine Miliaria)
Hidradenitis
Neutrophilic Eccrine Hidradenitis
Idiopathic Palmoplantar Hidradenitis
• Occurs following vigorous physical activity, primarily in healthy children.
• Thought to be precipitated by rupture of eccrine glands.
• Erythematous, tender nodules appear suddenly, most often on the soles (Fig. 32.8), and then spontaneously resolve over days to weeks.
Other
Keratolysis Exfoliativa
• Common disorder in healthy individuals; affects the palms >> soles.
• Multiple annular and semi-annular collarettes of white scale that usually measure <5 mm, but may be larger (Fig. 32.9); no preceding vesicles or inflammation clinically.

Fig. 32.9 Keratolyis exfoliativa. Small annular collarettes of scale on the palm. Courtesy, Jean L. Bolognia, MD.
• Recurrent and sometimes associated with hyperhidrosis.
• Rx: nonspecific; effectiveness of topical agents, e.g. 12% ammonium lactate, 20% urea, is limited.
For further information see Chs. 35 and 39. From Dermatology, Third Edition.










