Chapter 17 Discogenic Pain and Discography for Spinal Injections
History and Background
Discography has become a valuable diagnostic tool since its introduction in the 1940s to diagnose lumbar disc herniation.1–3 Since discography was introduced, computed tomography (CT) and magnetic resonance imaging (MRI) scanning have also added to our knowledge of the lumbar discs; however, because structural abnormalities such as degenerative disc changes, herniations, and annular tears occur in patients asymptomatic of low back pain,4,5 discography is the only direct method to asses if a disc is painful or not. Discography has also been shown to reveal abnormalities in symptomatic patients with normal MRI scans.6,7
Today, discography is used most often to identify painful internally disrupted discs.3 Discography is unique in that it is the only diagnostic technique that directly correlates a patient’s symptoms with disc morphology.4 This is analogous to palpation, which is fundamental to physical diagnosis.5 Tenderness elicited on palpation is analogous to pain provocation on discography.
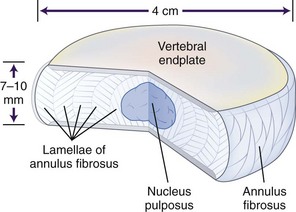
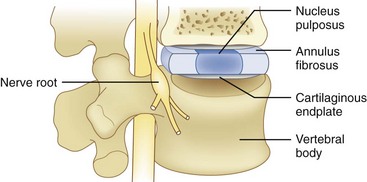
When evaluating a suspected spinal origin of pain, it is critically important to assess the significance of pathological findings on imaging studies and to determine whether those findings correlate with a patient’s symptoms. Discography is distinctive in its ability to make this determination. Discography is used in the lumbar,6–19 thoracic,20–25 and cervical26–35 regions to assess pain that is suspected to be of discogenic origin. Discogenic pain is mechanical in nature (exacerbated with activity and relieved by rest) and is felt primarily in an axial distribution. Performing discography involves the injection of radiographic contrast into the nucleus of the intervertebral disc to visualize disc morphology (Fig. 17-1).4
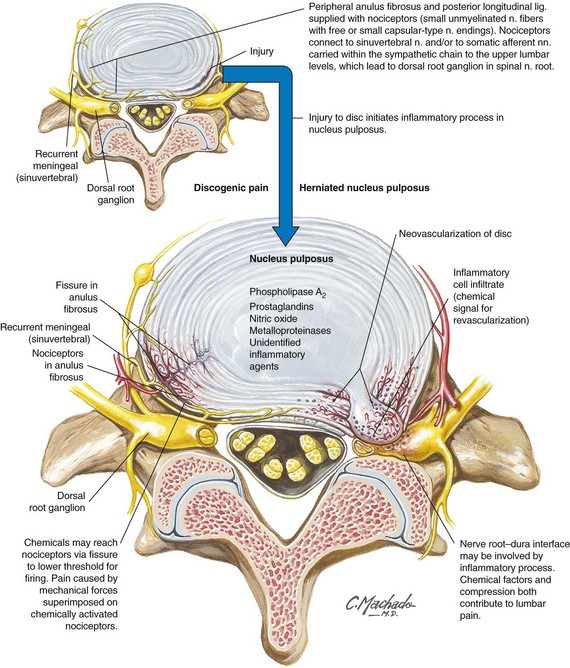
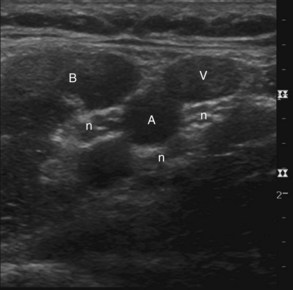
The prevalence of discogenic low back pain is 39% in those with low back pain persisting for at least 6 months and who have an unremarkable diagnostic workup and 26% of patients without radicular pain after facet joint pain was eliminated by either performing a diagnostic median branch nerve block or an intraarticular facet joint injection.36 The advent of new technology such as MRI, CT, and CT myelography has improved anatomical visualization of spine structures. However, these diagnostic modalities have not reliably identified the anatomical location of symptomatic spinal structures. This is evident in the individual who does not have radicular symptoms. Discs that appear normal or abnormal on MRI can either reproduce clinical symptoms during discography or be painless. The lumbar discs are innervated by branches from the lumbar ventral rami, the grey rami communicans, and the sinuvertebral nerve (Figs. 17-2 and 17-3). Lumbar discography has been postulated as a diagnostic test to elucidate the specific disc that requires disc excision and fusion with subsequent pain relief. The North American Spine Society (NASS) released its Position Statement on Discography in 198837 and again in 1995, summarizing the indications for discography. Both the International Spine Injection Society and NASS agree on the criteria for functional discography. Each organization indicates that a “chemically” sensitive disc is one that a patient feels pain at a low pressure stimulus (basically <15 psi). Between 15 and 50 psi, if a patient experiences pain that is concordant with the pathology of the painful disc, then it is deemed a pressure-sensitive disc. Pressures greater than 51 psi to 90 psi above the opening pressure are noted to be determined. A pressure above 90 psi is stated as being normal. The most common indication for lumbar discography is the need to determine whether one or more lumbar discs are responsible (i.e., the pain generator) for chronic ongoing low back pain. The study by Walsh et al38 refuted the findings by Holt19 demonstrating a 0% false-positive rate. Recent literature has demonstrated that compared with present imaging modalities, lumbar discography and lumbar CT discography are superior to MRI in determining abnormal annular pathology.39–43
Several studies have demonstrated the limitations of MRI compared with lumbar discography in identifying symptomatic versus asymptomatic discs.39–42 In 2000, Carragee et al44 challenged the concept of zero false-positive discography results on the grounds that abnormal psychometrics lead to misleading abnormal results. Manchikanti et al,45 in 2001, to the contrary, did not find any impact on discography results in those with or without a somatization disorder. Crock46 was the first to use the term internal disc disruption in 1970 to describe the clinical syndrome of axial low back pain secondary to pathological changes within the disc in the absence of a disc herniation. Radial fissures into the outer innervated annulus can cause pain because of mechanical or chemical irritation. This is the salient pathologic feature of internal disc disruption that cannot be detected on plain radiography, CT, or myelography because these studies are unable to detect internal disc abnormalities.
CT combined with discography allows the detection of annular pathology and determines if it is symptomatic or not. MRI can reveal annular pathology but cannot determine whether or not the disc is the pain generator (Fig. 17-2).38–41 Although the presence of a high intensity zone (HIZ) on T2-weighted MRI sagittal images in the posterior annulus (representative of a radial annular fissure) has a near 90% positive predictive value with concordant discography,34–36,38,39 this is not absolute, and the absence of an HIZ does not exclude annular pathology or discogenic low back pain.38–42 HIZ lesions are also found in patients without low back pain symptoms.47–49 Lumbar discography is not only important in identifying discs that are pain generators but also serves a key role in detecting whether abnormal or normal discs (based on imaging studies) are painful.
Pathophysiology
Two of the most common problems associated with the intervertebral disc are intervertebral disc degeneration and intervertebral disc protrusion or herniation; however, the two processes are not mutually exclusive. Extruded nucleus pulposus spontaneously produces increased amounts of matrix metalloproteinases, nitric oxide, interleukin-6, prostaglandin E2, and other chemical mediators (Fig. 17-3). These products may be intimately involved in both the biochemistry of disc degeneration and the pathophysiology of radiculopathy.
Intervertebral disc degeneration is difficult to define and is also difficult to separate from the normal aging process of the intervertebral disc. However, there is a wide variation in the aging and degenerative process of the disc, and some septuagenarians have the intervertebral discs of 30-year-old adults and vice versa. The hallmarks of disc degeneration are loss of fluid and fluid pressure, disruption or breakdown of collagen (including tearing of the annulus fibrosus) and proteoglycans, and sclerosis of the cartilaginous endplate and adjacent subchondral bone. The normal aging and degeneration of the intervertebral disc is closely related to the number of vessels that reach the intervertebral disc, especially the cartilaginous endplate. As the number of vessels decreases and the nutrition provided and waste removed by these vessels decrease, the changes associated with intervertebral disc aging and degeneration increase.46 The first significant degenerative changes in the intervertebral disc appear around 11 to 12 years of age.
The number of clefts and radial tears increases from 17 to 20 years of age, and the overall number of chondrocytes decreases as cell death, mucoid degeneration, and granular changes begin to appear.45 The number of clefts and radial fissures continues to increase until late in life (>70 years of age).
Functional Discography
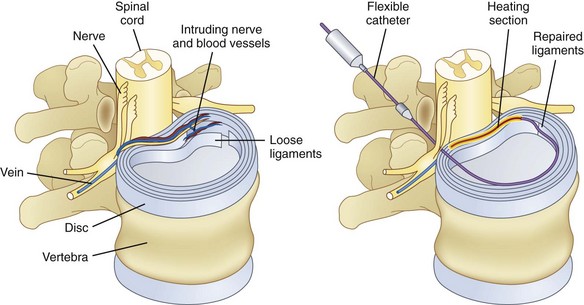
Functional anesthetic discography (FAD)50 is an additional test that can be carried out after provocation discography. It is based on analgesic discography, in which local anesthetic is injected into a painful disc and pain relief is assessed. The theory is similar to diagnostic injections of facet joints or sacroiliac joints. A 17-gauge introducer needle is used for disc access. After the provocation discogram, a balloon-tipped catheter is placed into the center of the disc through the needle (Fig. 17-4).50 The balloon is inflated with contrast, and a stopcock is closed to secure the catheter in the nucleus.
Alamin and coworkers51 reported that 50% of patients (n = 32) had confirmatory findings on FAD after a positive discogram result. The patients with confirmatory FAD underwent fusion and were followed for at least 3 months. The mean preoperative Oswestry Disability Index score was 58.5, and the mean postoperative score was 26.5. The mean preoperative VAS score for back pain was 7.2, and the mean postoperative VAS score was 3.1.
Intradiscal Procedures
Disc biacuplasty is a procedure for treating discogenic pain through neuron ablation by heating intervertebral disc tissue using cooled, bipolar radiofrequency (RF) technology. One study52 has demonstrated temperature profiles created by disc biacuplasty in human cadavers.
Many practitioners have used various injection formulas to help patients with discogenic pain (Table 17-1). From the Saal brothers using intradiscal electrothermal therapy53 to the use of catheters, medications, and now a “super glue” to help seal off annular tears, these techniques enable us to stop pain emitting from the intradiscal areas of the nucleus (Fig. 17-5).
| Discogenic Pain | Radicular Pain | Facet Joint Pain |
|---|---|---|
| IDET | Dekompressor | Radiofrequency ablation |
| DiscTRODE | Epidural steroids | Intraarticular injections |
| Nucleoplasty | Median branch nerve injection | |
| SpineWave | ||
| SpineWand | ||
| Biaculoplasty |
IDET, intradiscal electrothermal therapy.
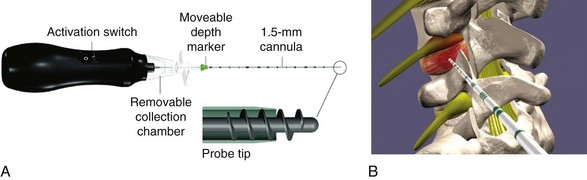
Nucleoplasty from Arthrocare Spine allowed the knowledge and technique to be capitalized on by the use of RF energy to heat up channels within the disc, allowing a coblation and coagulation to occur simultaneously inside the nucleus. By the use of the technique, one could vaporize material and create a negative vacuum in the nucleus, thereby allowing the outer rim to retract back into the disc. Stryker developed the very well-known and proven Dekompressor. This device actually removes intradiscal material and creates a negative vacuum in the disc, allowing the out-bulge defect to retract and lessen the contact on the nerve root (Fig. 17-6). The use of a sealant to stop annular stimulation in addition to helping the disc to actually rehydrate is another novel concept. Spinal Restoration in Austin, Texas, is in a third-phase clinical trial analyzing the concept at the present time.
1 Lindblom K. Technique and results in myelography and disc puncture. Acta Radiol. 1950;34:321-330.
2 Aprill C, Bogduk N. High-intensity zone: A diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992;65:361-369.
3 Guyer RD, Ohnmeiss DD. Lumbar discography. Position statement from the North American Spine Society Diagnostic and Therapeutic Committee. Spine. 1995;20:2048-2059.
4 Lindblom K. Technique and results of diagnostic disc puncture and injection (discography) in the lumbar region. Acta Orthop Scand. 1951;20:315-326.
5 Bogduk NC, Aprill C, Derby R. Discography. In: White A, Schofferman A, editors. Spine Care. Diagnosis and conservative treatment. St. Louis: Mosby; 1995:219-236.
6 Lam KS, Carlin D, Mulholland RC. Lumbar disc high-intensity zone: the value and significance of provocative discography in the determination of the discogenic pain source. Eur Spine J. 2000;9:36-41.
7 Schellhas KP, Pollei SR, Gundry CR, Heithoff KB. Lumbar disc high-intensity zone. Correlation of magnetic resonance imaging and discography. Spine. 1996;21:79-86.
8 Buirski G, Silberstein M. The symptomatic lumbar disc in patients with low-back pain: magnetic resonance imaging appearance in both symptomatic and control population. Spine. 1993;18:1808.
9 Milette PC, Fontaine S, Lepanto L, et al. Differentiating lumbar disc protrusions, disc bulges and discs with normal contour but abnormal signal intensity. Magnetic resonance imaging with discographic correlations. Spine. 1999;24:44.
10 Ohnmeiss DD, Vanharanta H, Ekholm J. Relation between pain locations and disc pathology: a study of pain drawings and CT/discography. Clin J Pain. 1999;15:210.
11 Walsh TR, Weinstein JN, Spratt KF, et al. Lumbar discography in normal subjects: a controlled, prospective study. J Bone Joint Surg. 1990;72:1081.
12 Manchikanti L, Singh V, Pampati V, et al. Provocative discography in low back pain patients with or without somatization disorder: a randomized prospective evaluation. Pain Physician. 2001;4:227-239.
13 Horton WC, Daftari TK. Which disc visualized by magnetic resonance imaging is actually a source of pain? A correlation between magnetic resonance imaging and discography. Spine. 1992;17:S164-S171.
14 Kornberg M. Discography and magnetic resonance imaging in the diagnosis of lumbar disc disruption. Spine. 1989;14:1368-1372.
15 Manchikanti L, Singh V, Pampati V, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308-316.
16 Buenaventura RM, Shah RV, Patel V, et al. Systematic review of discography as a diagnostic test for spinal pain: an update. Pain Physician. 2007;10:147-164.
17 Bogduk N. Lumbar disc stimulation (provocation discography). In: Practice Guidelines for Spinal Diagnostic and Treatment Procedures. ISIS. 2004:20-46.
18 Derby R, Eek B, Lee SH, et al. Comparison of intradiscal restorative injections and intradiscal electrothermal treatment (IDET) in the treatment of low back pain. Pain Physician. 2004;7:63-66.
19 Holt EPJr. Fallacy of cervical discography. Report of 50 cases in normal subjects. JAMA. 1964;188:799-801.
20 Schellhas KP, Pollei SR, Dorwart RH. Thoracic discography: a safe and reliable technique. Spine. 1994;19:2103.
21 Wood KB, Schellhas KP, Garvey TA, Aeppli D. Thoracic discography in healthy individuals: a controlled prospective study of magnetic resonance imaging and discography in asymptomatic symptomatic individuals. Spine. 1999;24:1548.
22 Winter RB, Schellhas KP. Painful adult thoracic Scheuermann’s disease: diagnosis by discography and treatment by combined arthrodesis. Am J Orthop. 1996;25:783.
23 Winter RB, Schellhas KP. Painful adult thoracic Scheuermann’s disease: diagnosis by discography and treatment by combined arthrodesis. Am J Orthop. 1996;25:783-786.
24 Bogduk N. Thoracic provocation discography. In: Practice Guidelines for Spinal Diagnostic and Treatment Procedures. ISIS. 2004:287-294.
25 Singh V. Thoracic discography. Pain Physician. 2004;7:451-458.
26 Parfenchuck TA, Janssen ME. A correlation of cervical magnetic resonance imaging and discography/computed tomographic discograms. Spine. 1994;19:2819.
27 Schellhas KP, Smith MD, Gundry CR, Pollei SR. Cervical discogenic pain: prospective correlation of magnetic resonance imaging and discography in asymptomatic subjects and pain sufferers. Spine. 1996;21:300.
28 Schellhas KP, Garvey TA, Johnson BA, et al. Cervical discography: analysis of provoked responses at C2-C3, C3-C4, and C4-C5. Am J Neuroradiol. 2000;21:269.
29 Grubb SA, Kelly C. Cervical discography: clinical implications from 12 years of experience. Spine. 2000;25:1382.
30 Fortin JD. Cervical discography with CT and MRI correlations. In: Lennard TA, editor. Pain Procedures in Clinical Practice. Philadelphia: Hanley and Belfus; 2000:230-240.
31 Bogduk N. Cervical disc stimulation (provocation discography). In: Practice Guidelines for Spinal Diagnostic and Treatment Procedures. ISIS. 2004:95-111.
32 Roth DA. Cervical analgesic discography. A new test for the definitive diagnosis of painful-disk syndrome. JAMA. 1976;235:1713-1714.
33 Whitecloud TSIII, Seago RA. Cervical discogenic syndrome. Results of operative intervention in patients with positive discography. Spine. 1987;12:313-317.
34 Motimaya A, Arici M, George D, Ramsby G. Diagnostic value of cervical discography in the management of cervical discogenic pain. Conn Med. 2000;64:395-398.
35 Zeidman SM, Thompson K, Ducker TB. Complications of cervical discography: analysis of 4400 diagnostic disc injections. Neurosurgery. 1995;37:414-417. 1994
36 Manchikanti L, Singh V, Pampati V, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308-316.
37 Executive Committee of North American Spine Society. Position Statement on Discography. Spine. 1988;13:1349.
38 Walsh TR, Weinstein JN, Spratt K, et al. Lumbar discography in normal subjects. J Bone Joint Surg Am. 1990;72:1081-1088.
39 Horton WC, Daftari TK. Which disc visualized by magnetic resonance imaging is actually a source of pain? A correlation between magnetic resonance imaging and discography. Spine. 1992;17:S164-S171.
40 Kornberg M. Discography and magnetic resonance imaging in the diagnosis of lumbar disc disruption. Spine. 1989;14:1368-1372.
41 April C, Bogduk N. High intensity zone. A diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992;65:361-369.
42 Schellhas KP, Pollei SR, Gundry C, Heithoff KB. Lumbar disc high-intensity zone. Correlation of magnetic resonance imaging and discography. Spine. 1996;21:79-86.
43 Schwarzer AC, Aprill CN, Derby R, et al. The relative contributions of the disc and zygapophyseal joint in chronic low back pain. Spine. 1994;19:801-806.
44 Carragee E, Tanner C, Khurana S, et al. The rates of false-positive lumbar discography in select patients without low back symptoms. Spine. 2000;25:1373-1380.
45 Manchikanti L, Singh V, Pampati V, et al. Provocative discography in low back pain patients with or without somatization disorder: a randomized prospective evaluation. Pain Physician. 2001;4:227-239.
46 Crock HV. A reappraisal of intervertebral disc lesions. Med J Augst. 1970;1:983-989.
47 Smith BM, Hurwitz EL, Solsberg D, et al. Interobserver reliability of detecting lumbar intervertebral disc high-intensity zone on magnetic resonance imaging and association of high-intensity zone with pain and annular disruption. Spine. 1998;23:2074-2080.
48 Lam KS, Carlin D, Mulholland RC. Lumbar disc high-intensity zone: the value and significance of provocative discography in the determination of the discogenic pain source. Euro. Spine J. 2000;9:36-41.
49 Stadnik TW, Lee RR, Coen HL, et al. Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Neuroradiology. 1998;206:49-55.
50 Functional Anesthetic Discography [Package Insert]. Sunnyvale, California: Kyphon Inc, 2006.
51 Alamin T: International Society for the Study of the Lumbar Spine. Abstracts. Bergen, Norway; June 13-17, 2006, pp 52-53.
52 Karaman H, Tüfek A, Kavak GÖ, et al. 6-month results of transdiscal biacuplasty on patients with discogenic low back pain: preliminary findings. Int J Med Sci. 2011;8:1-8.
53 Saal JA, Saal JS. Intradiscal electrothermal therapy for the treatment of chronic discogenic low back pain. Clin Sports Med. 2002;21(1):167-187.