Chapter 4 Differential Diagnostic Nerve Blocks
 Despite its limitations, DDNBs can aid in distinguishing, in broader terms, pain with significant peripheral component versus pain with predominant central component.
Despite its limitations, DDNBs can aid in distinguishing, in broader terms, pain with significant peripheral component versus pain with predominant central component. When integrated with other clinical findings, DDNBs can guide the physician into understanding predominant pain mechanisms, especially of patients whose pain diagnoses have been elusive and largely untreated.
When integrated with other clinical findings, DDNBs can guide the physician into understanding predominant pain mechanisms, especially of patients whose pain diagnoses have been elusive and largely untreated. DDNBs have the potential ability to prognosticate successful response to interventions such as surgery or neurolysis before its implementation.
DDNBs have the potential ability to prognosticate successful response to interventions such as surgery or neurolysis before its implementation. The levels of the block achieved does not imply with certainty conduction block of all nerve fibers.
The levels of the block achieved does not imply with certainty conduction block of all nerve fibers. Variability exists in the rate of recovery among sympathetic, visceral, and somatic fibers after the blocks wears off.
Variability exists in the rate of recovery among sympathetic, visceral, and somatic fibers after the blocks wears off. Local anesthetic formulation (pH, lipophilicity, baricity) could significantly affect the results of the DDNB.
Local anesthetic formulation (pH, lipophilicity, baricity) could significantly affect the results of the DDNB. Pain cannot be characterized as only central even in the event of a negative DDNB result because peripheral mechanisms can still be present.
Pain cannot be characterized as only central even in the event of a negative DDNB result because peripheral mechanisms can still be present. The level of the block and its assessment is important, particularly for abdominal visceral pain, where fibers from visceral organs could synapse over several spinal cord segments.
The level of the block and its assessment is important, particularly for abdominal visceral pain, where fibers from visceral organs could synapse over several spinal cord segments. DDNBs, together with clinical, radiological, laboratory, history, physical examination, and psychosocial findings, need to be integrated together as parts of a complex puzzle in order to effectively diagnose and meaningfully treat the totality of a patient’s pain presentation.
DDNBs, together with clinical, radiological, laboratory, history, physical examination, and psychosocial findings, need to be integrated together as parts of a complex puzzle in order to effectively diagnose and meaningfully treat the totality of a patient’s pain presentation. Neurophysiological data have undermined some of the basic assumptions associated with DDNBs, and in doing so also limit the validity of its interpretation.
Neurophysiological data have undermined some of the basic assumptions associated with DDNBs, and in doing so also limit the validity of its interpretation.Introduction
Differential neural blockade has been used to obtain diagnostic information for ill-defined pain conditions that elude specific diagnoses. The technique, although deemed controversial by some,1 can have the potential to aid pain physicians with a more objective assessment of a patient’s pain and in doing so aid in developing a better approach to treatment.2,3 The International Association for the Study of Pain defines pain as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”4 One aspect of pain is nociception, which entails a complex series of electrochemical events that entail transduction of nociceptive stimuli from receptive nerve endings, transmission of impulses, modulation, and translation of subjective sensory and emotional experiences of pain.5 Other factors either unrelated or reinforced by this processes contribute to the pain experience. Thus, one of the greatest challenges that face many pain physicians today is identifying the relative contributions of psychosocial, cognitive, visceral, and somatic contributions involved in a patient’s perception of pain. The rationale for performing diagnostic differential neural blocks (DDNBs) is based on the selective blockade of specific neurological pathways and/or modalities while sparing others. In doing so, DDNBs have the potential to do the following6: (1) help to determine whether a patient has predominantly a physical or psychological component contributing to the experience of pain, (2) aid in assessing whether pain is mediated via sympathetic or somatic fibers, (3) identify potential response to placebo, and (4) predict a patient’s likelihood for success from interventions such as surgery or neurolysis.
The approach to DDNB is varied and may have evolved over the years. The “classic approach,” as described in 1964 by McCollum and Stephen,7 proposes varying concentrations of local anesthetic to be injected intrathecally. This approach mainly relies on the relative susceptibilities of the different types of nerve fibers to create a concentration-dependent response differential that enables the selective blockade of specific neuronal pathways while sparing others. The “modified approach” was introduced as a more time-efficient and practical alternative to its classic counterpart.3,8,9 Subsequently, clinicians used the “epidural approach” in the hopes of minimizing post–lumbar puncture cephalgia associated with spinal injections.2 Other approaches that have also been introduced include the “anatomical approach” and the “opioid approach.” The “anatomical approach” relies on the sequential blockade of specific nerve fibers based on its anatomical locations as opposed to differential susceptibility to varying concentrations of local anesthetic.3 The “opioid approach,” introduced in 1985, suggests the use of epidural opioid in lieu of local anesthetics to eliminate a potential source of bias (i.e., cues of numbness and warmth that the local anesthetic may give to patients undergoing the test).6 The latter two approaches do not necessarily provide better diagnostic value than the classic or modified approaches. On the contrary, critics have pointed out that they may be less effective in differentiating specific pain pathways as will be discussed further below.1,10–12
Historical Perspective
The concept of differential nerve blockade is largely based on the early studies of Gasser and Erlanger in 1929.13,14 These two American scientists who studied the effects of cocaine on canine peripheral nerves suggested that small-diameter nerve fibers were more susceptible to the blocking actions of local anesthetics compared with larger nerve fibers because the former possess greater surface to volume ratio, thus rendering the axoplasm more readily infiltrated by local anesthetics.14 This early model of differential neural blockade has come to be known as the “size principle” and has also served as an explanation for the differential loss of function observed clinically during spinal and epidural anesthesia.15,16 These findings subsequently led to the use of differential spinal blocks as a diagnostic tool for pain.7,13 However, neurophysiological evidence has since disproven Gasser and Erlanger’s concept of nerve conduction, and over time, their “size principle” has also been challenged.17–19 In 1989, Fink20 proposed the “length principle” as an alternative explanation. This principle suggests that for nerve fiber conduction to be blocked, three consecutive nodes of Ranvier must be exposed to the local anesthetic.21 The “length principle” has been considered an extension rather than a renunciation of the original “size principle” because axonal diameter does correlate with internodal distance.22 The thicker the diameter of an axon, the further the internodal distance and the less amount of nodes likely exposed to a given amount of local anesthetic. However, the “size principle,” which has influenced most of the work on differential blocks, could be misleading because given a sufficient length of nerve, there is no apparent difference in the concentration of local anesthetics required for a conduction nerve block in all fibers.23 To proponents of DDNBs, Fink’s “length principle” provides a valid explanation that links stepwise loss of function observed clinically with neuraxial anesthesia to the concept of differential nerve fiber susceptibility and thus justifies, to a certain extent, its use as a diagnostic tool for pain.3
Classification of Five Types of Pain
DDNBs, as classically described, involve injecting saline and then local anesthetic in gradually increasing strengths into the spinal space.7 The goal is to delineate the underlying pain mechanism that could fall under one of five types:
Placebo-Responsive Pain
Pain is considered to be placebo responsive if relief occurs after the injection of saline. It has been shown that up to 35% of patients with true organic pain actually respond to placebo; however, this is short lived and self-limiting.24 If pain relief after placebo persists for an extended period of time, an underlying psychogenic pain mechanism may be considered.
Sympathetic Pain
Pain mediated by sympathetic fibers is inferred if the patient experiences relief after sympathetic fibers are blocked with sympatholytic concentrations of anesthetic, which are thought to be lower anesthetic concentrations sufficient enough to block sympathetic preganglionic B fibers while sparing other fiber types.25,26 Pain relief should occur concomitantly with signs of sympathetic blockade such as temperature changes and sympathogalvanic response (SGR; the activation of sweat glands by postganglionic sympathetic fibers) but without signs of sensory block.
Visceral Pain
Visceral pain is pain originating from internal organs. Stimuli required to elicit pain in visceral organs vary between structures (e.g., the myocardium is sensitive to ischemia but not to mechanical stimulation). The quality of visceral pain is often different from somatic pain. Although somatic pain is initially sharp followed by localized burning or throbbing, visceral pain tends to be poorly localized, presenting as dull, aching sensations. Although this type of pain is conducted by Aδ and C fibers, the ratio of Aδ to C fibers is 1 : 10 in viscera as opposed to 1 : 2 in cutaneous afferents.27 Furthermore, visceral nociceptive fibers have extensive overlap among their receptive fields.28,29
Central Pain
If the patient does not gain any relief from any of the injections despite achieving surgical levels of anesthesia of nerves that cover the target organ, then a central mechanism or pain generator should be suspected. Central pain can be attributed to one of four possible causes, including central lesions, true psychogenic pain, malingering, or encephalization.2 Central lesions involve damage to or dysfunction of the central nervous system (CNS) above the level of the differential nerve block. Examples include poststroke thalamic pain and multiple sclerosis. Pain with psychogenic features refers to physical pain perpetuated by an underlying psychological disorder such as depression or anxiety. Encephalization is a poorly understood phenomenon that has been proposed to explain central pain3 whereby chronic, severe pain of peripheral origin becomes self-sustaining at a central level and remains persistent despite removal of the original peripheral triggering mechanism. Malingering is the deliberate feigning or exaggeration of pain or illness in anticipation of some benefit such as financial compensation or avoidance of responsibility. There are no valid clinical methods for its assessment and thus can be difficult to prove or disprove.30
Classification of Nerve Fibers
Gasser and Erlanger14 earlier developed the classification system for peripheral nerve fibers mainly based on axonal diameter, conduction velocity (in meters per second), and myelination. This system is still in use today and basically categorizes nerve fibers into three types: A, B, and C.
C Fibers
Fiber diameter is a function of how heavily myelinated the axons are. Larger A fibers are heavily myelinated and have greater conduction velocities measured as the distance an action potential travels through an axon over time in meters per second. On the other hand, C fibers are unmyelinated and small in size and have the slowest conduction velocity.31,32 Properties of nociceptive compared with non-nociceptive somatic afferent neurons include a longer action potential duration and a slower maximum rate of fiber firing. These properties appear to be graded according to the conduction velocity group with the slowest fibers having the longest action potential and least rate of fiber firing (C > Aδ > A-α/β).33
The Role of Local Anesthetics
Local anesthetics block the propagation of nerve impulses such as those for pain by inhibiting the formation and propagation of action potentials. Several mechanisms have been proposed, but most evidence suggest that the sodium channel is the key target.34 By diffusing through the axonal membrane, local anesthetics bind to the cytoplasmic side of a sodium channel, thereby inhibiting conformational changes that would have otherwise resulted in the channel’s opening for sodium influx and activation. Local anesthetics do not only block inward sodium channels but also the outward potassium channels, which might be an important effect because potassium channels are responsible for repolarization and maintenance of resting membrane potential, which affects excitability.35,36 Clinical onset depends on the rate of diffusion through the neuronal membrane. Thus, amide-based local anesthetics such as bupivacaine that happen to be more lipophilic are thought to produce nerve blockade more readily than the less lipid soluble ester-based local anesthetics such as procaine. Lipophilicity allows the anesthetic to penetrate a nerve fiber more readily and exert its effect before being removed into the circulation. In theory, a less lipophilic local anesthetic would be the more ideal agent for DDNBs because they produce blockade of smaller fibers (e.g., C fibers) more readily but are then removed by the circulation before they can penetrate the diffusion barriers of larger fibers. As such, greater concentrations of ester-based anesthetics would be needed to create blockade of larger fibers and the differential is more easily established. In vivo studies, however, have found that regardless of type of local anesthetic, a differential in susceptibility exists based on fiber type with A-α fibers consistently less sensitive to local anesthetic, regardless of type, versus the smaller C or A-δ fibers.37 The order of susceptibility to blockade by local anesthetic is as follows: (most susceptible to least susceptible) B < C < A-δ < A-γ < A-β < A-α.2,3,20,38
Proposed Mechanisms of Differential Neural Blockade
DDNBs are based on the premise that a given concentration of local anesthetic can selectively block a specific nerve fiber type while sparing others.1 The mechanism of this differential effect is not clearly understood.20,39 Several explanations have been offered.
Bathed Length Principle
For local anesthetics to effectively block a nerve fiber, at least three nodes of Ranvier need to be bathed in the anesthetic because conduction can leap two consecutive blocked nodes but not three.40 Fink’s “bathed length principle” suggests that a functional relationship between local anesthetic susceptibility and fiber length (and therefore size) exists.20 That is, smaller diameter fibers are more easily blocked than larger diameter fibers, which tend to have greater internodal distance and thus tend to require more anesthetic for three consecutive nodes to be bathed. After the three-node requirement is met, there is a minimum concentration of local anesthetic required for each fiber type to have all of its sodium channels occupied before conduction can be blocked. This is known as the minimum blocking concentration (Cm). Smaller fibers are thought to have smaller Cms than larger fibers, enabling different types of fibers to respond to different concentrations of anesthetic.19,41
Sodium Channel Packing
Sodium channel density at the nodes of Ranvier are thought to be increased as fiber size increases.42 This increased distribution of sodium channels on larger fibers is referred to as “sodium channel packing” and has been proposed as one possible mechanism that explains why larger fibers require a higher Cm than do smaller fibers.3
Decremental Conduction
Given an impulse conducting along an axon, there is thought to be a cumulative decrease in the currents excited with successive nodes of Ranvier.20 For local anesthetic concentrations below the Cm, not enough sodium channels within a node are blocked such that at each node, the action potential undergoes a progressive reduction in amplitude and conduction until succeeding nodes are rendered vulnerable to even suboptimal doses of anesthetic. This phenomenon, referred to as “decremental conduction,” has mainly been demonstrated in myelinated axons.20,43 Thus, for anesthetic concentrations below the Cm, impulse blockade is more likely to occur in fibers in which a greater number of nodes are exposed. Larger fibers are therefore less vulnerable because even if conduction is decrementally slowed, not enough nodes are exposed to the lower anesthetic dose, enabling the impulse to again resume full conduction speed after the conducting membrane is again reached.
Frequency-Dependent Block
This phenomenon occurs when repetitive firing of a nerve effects a cumulative depression of sodium currents such that suboptimal doses of local anesthetic then become sufficient to establish blockade. This explains why preganglionic sympathetic B fibers, which convey repetitive, tonic vasoconstrictive impulses, are most susceptible to local anesthetic.39,44 It has been proposed that both phenomena, frequency-dependent block and decremental conduction, may superimpose on each other and even further enhance the blocking effect of considerably low concentrations of local anesthetic.3
Diagnostic Differential Nerve Block: Classic Approach
The classic DDNB as described below is largely based on the works of Arrowood and Sarnoff in 194813 and McCollum and Stephen in 1964.7 The technique involves injecting local anesthetic into the subarachnoid space to obtain diagnostic information from patients with lower extremity or lower trunk pain. This serves as the prototype diagnostic differential block from which subsequent versions are based.3
Interpretation
If the patient reports relief of pain after the injection of Solution A (normal saline), his or her pain is thought to be placebo responsive. Psychologic facilitatory mechanisms may even be suggested if relief is long lasting because true placebo responses are usually short lived and self-limiting.3 As such, a repeat procedure or psychological referral may be of value. If pain relief occurs after the injection of Solution B (procaine 0.25%), the inference is that sympathetic preganglionic B fiber activity is mainly involved. This is confirmed by clinical signs of a sympathectomy, which can include an increase in temperature and a SGR without concurrent signs of cutaneous or sensory involvement. These types of patients may respond beneficially to sympathetic blocks. If pain relief occurs after Solution C (procaine 0.5%) is injected and there is clinical evidence of sensory involvement such as diminished cutaneous sensation to pinprick covering the distribution of pain, then the implication is that A-δ fibers, C fibers, or both are involved. If relief is achieved only after Solution D (procaine 5%) is injected, the mechanism remains to be considered somatic in origin, taking into account the potential for interindividual variability with the presumption that some patients may have higher Cms.3 If the patient does not obtain any relief despite evidence of complete sympathetic, somatic, and even motor blockade, the underlying pain mechanism is thought to be central in origin, which could point to any one of the four possible causes described earlier: CNS lesion, psychogenic pain, malingering, or encephalization.
Diagnostic Differential Nerve Block: Modified Approach
The modified approach was developed as a more practical and expeditious alternative to its classic counterpart.3,8,9 This approach uses only two of the four solutions. The goal is to block all types of fibers immediately. The patient is then observed in reverse order as fibers recover sequentially starting with the larger diameter fibers. Thus, instead of correlating pain relief with onset of fiber blockade, the modified approach correlates the return of pain with the return of fiber function.
Diagnostic Differential Nerve Block: Epidural Approach
To avoid a spinal puncture and thus diminish the chances of a spinal headache, the epidural approach has been proposed as an alternative to the spinal injections.6 This epidural approach is procedurally similar to its spinal counterpart with the following exception: instead of the subarachnoid space, the epidural space is accessed for the injection of solutions. Thus, the epidural approach can also be done in two ways, mirroring the classic and modified versions described above.
Description
The epidural approach mirroring the classic procedure was introduced by Raj in 1977.45 The epidural space is accessed using the loss-of-resistance technique via an epidural needle, and the solutions injected sequentially into the epidural space are as follows: “Solution A” containing normal saline; “Solution B” containing lidocaine 0.5%, considered the mean sympatholytic epidural concentration; “Solution C” containing lidocaine 1%, considered the mean sensory-blocking epidural concentration; and “Solution D” containing lidocaine 2%, considered the mean epidural concentration to block all modalities.
Diagnostic Differential Nerve Block: Opioid Approach
One criticism of neuraxial DDNBs as previously described is that local anesthetics can provide patients with cues of numbness or warmth in the area of blockade,1,3,46 especially if they have had previous experience with local anesthetics (e.g., from a laboring epidural or at a dentist office).6 This cue could potentially or subconsciously alert the patient to the presumed onset of pain relief, which could potentially cast doubt on the interpretation of the patient’s subjective response.1,6,46 Thus, using epidural opioids have been suggested as an alternative to local anesthetics.6,47 Opioid effects are thought to be more specific and do not provide the cues of numbness or warmth to trigger placebo responses.1
Interpretation
Analgesia reported by the patient after the injection of fentanyl indicates a predominantly nociceptive mechanism for the pain versus a predominantly psychologic one. Reversal of analgesia after injection of naloxone by the unaware patient further confirms the primarily nociceptive mechanism. No response to any of the above injections, including lidocaine, implicates predominantly psychologic or social factors.6
Limitations
Epidural opioids may not be effective in relieving nonpsychogenic, neuropathic, or visceral pain.1,11,12 Additionally, IV naloxone does not necessarily reverse the analgesic effects of epidural opioids completely.48 There have been no formal studies comparing the opioid approach versus the other nonopioid approaches described.1,6 Therefore, further studies are needed.
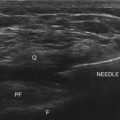
Diagnostic Differential Nerve Block: Anatomical Approach
The anatomical approach allows for the assessment of neck, upper extremity, thoracic, abdominal, pelvic, and lower extremity pain.3 It relies on the anatomical separation of the types of fibers and as such involves the sequential performance of three blocks for each assessment: the placebo block, the sympathetic block, and the somatic block. The anatomical approach allows for the injection of local anesthetic to block only one type of fiber at a time. Additionally, it is thought to obviate the problems associated with a high spinal or epidural block and may be more appropriate to use for assessment of pain in the upper part of the body.3
Description
For thoracic pain, the anatomical approach can be used, especially in cases in which an epidural DDNB is contraindicated. After the injection of placebo, a thoracic paravertebral sympathetic block is performed. This is followed by either a paravertebral somatic block or intercostal nerve block. Interpretation of results based on pain relief is similar to that previously described for head, neck, and upper extremity pain. The main caveat to using the anatomical approach in this region of the body is the associated increased risk for developing a pneumothorax.3 For this reason, the epidural approach is considered to be the safer block for the assessment of thoracic pain.
For abdominal pain, as above, placebo is injected first. However, in this location, it is suggested that the somatic block is performed before sympathetic block.31 The reason for this is that visceral pain, which largely courses via sympathetic fibers, can be more difficult to localize and characterize. Therefore, somatic or chest wall pain in the abdomen needs to be ruled out first.3 Thus, if a paravertebral or intercostal block produces complete anesthesia of the body wall pain distribution yet the patient’s and pain still persists, a celiac plexus or splanchnic nerve block is then performed to confirm if the pain is truly visceral in origin.
There is limited evidence for the use of DDNB as a diagnostic procedure for abdominal visceral pain, especially using an anatomical approach. In a study by Conwell et al,49 differential neuraxial blockade was used to determine the source of chronic abdominal pain in patients diagnosed with chronic pancreatitis. The modified epidural approach was used, and saline or 2% lidocaine was injected in a stepwise fashion to achieve surgical anesthesia. Patients were evaluated for recovery of motor and sensory function every 10 minutes. On the basis of the response to local anesthetic, pain was characterized as visceral, somatic (nonvisceral), or central in origin. Based on their results, the authors found that the majority of patients had nonvisceral chronic pain (only four of 22 had a positive visceral responses to DDNB) despite a pre-DDNB diagnosis of chronic pancreatitis. While recognizing the limitations of the technique, the authors concluded that DDNB is a useful procedure in attempting to diagnose visceral origin of pain, which could dictate further treatment plans.
Limitations
The anatomical approach, when compared with other approaches, can be more painful and less precise.3 It can involve three separate injections per patient. Additionally, because pain involving visceral structures can be subserved by a combination of sympathetic and somatic fibers,10 delineating a sympathetic versus a somatic mechanism for thoracic, abdominal, or pelvic pain may not always be as clear cut. Furthermore, there is potential for placebo response after each injection, whether sympathetic or somatic. Finally, because of the increased risk for a pneumothorax when performing paravertebral sympathetic blocks, the anatomical approach is considered less than ideal for the evaluation of thoracic pain.3
Discussion
The concept of differential neural blockade has been described since the 1920s. Yet many decades later, its validity and utility as a diagnostic measure remains under a cloud of controversy and scrutiny.1,46 The interaction between local anesthetic and nerve fiber is dynamic and influenced by multiple factors such as location of nerve fibers in the nerve bundle, the length exposed to the local anesthetic, the degree of activity of the nerve, and the local tissue factors (e.g., pH).
The basic premise that certain concentrations of local anesthetic block specific fibers in sequential fashion while sparing others is not a widely accepted concept. Hogan and Abram,1 for example, point to the “impossibility of complete block of one fiber type without at least a partial block of others.” In addition, although the sympathetic fibers are thought to be blocked first and recover last, some have argued that there may not be a size-related differential in fiber susceptibility, citing that the larger A-β fibers can be blocked by a concentration that spares the smaller C fibers.41 It has been demonstrated and confirmed that conduction block in myelinated nerve fibers are not linearly correlated with fiber conduction velocity/fiber size.50 Evidence that large-diameter fibers are more readily susceptible to local anesthetic is contrary to the notion of DDNB.19 These findings tend to suggest the absence of a true differential (i.e., sympathetic versus somatic pain may not be as easy to delineate as once thought).
Neurophysiological data have undermined some of the basic assumptions associated with DDNBs and in doing so, also limit the validity of its interpretation.1,46 For example, one premise of DDNBs is that pain is generated from a single peripheral source, and its impulses then travel via “unique and consistent” neural pathways.1 However, this may not always be the case. In chronic neuropathic pain states, the dorsal root ganglia (DRG) of injured nerves can spontaneously generate pain impulses with or without peripheral nerve or nociceptor activation. Thus, blocking nociceptor or peripheral nerves close to the site of initial injury but distal to the DRG may not stop the spontaneous firing of the DRG. Therefore, the patient’s perception of pain remains. This would then lead to the mistaken assumption that the injured nerve is not responsible for the patient’s pain. Pain does not necessarily involve one specific peripheral source, pathway, or mechanism as a simplistic interpretation of a DDNB would suggest. There can be complex and possibly multiple neurophysiological processes that play a role in the generation, propagation, and maintenance of pain, each contributing its own unique dimension and adding to the complexity of the experience of pain. These are factors that need to be taken into consideration by the clinician when interpreting the results of a DDNB.
DDNB is not a one size fits all phenomenon. Interindividual variations in neural anatomy and local anesthetic response need to be taken into account.1 For example, the Cm can differ among different patients and different patient conditions. Lidocaine 0.25% that is thought to selectively block predominantly sympathetic fibers for some individuals may be enough of a concentration to block all types of sensory fibers for others.1,6 Actively firing afferent fibers such as those from injured peripheral nerves may be more sensitive to local anesthetic and thus tend to have lower than normal Cms such that very low concentrations of anesthetics can reduce maximum firing rates of the axons and produce pain relief without necessarily diminishing skin sensation to temperature or pinprick.1 Thus, pain relief may be erroneously attributed to sympathetic blockade when nociceptive fibers were actually blocked. Nerve fiber sensitivity to local anesthetics varies. This is demonstrated by the differential ability of bupivacaine at a given concentration to block sensory fibers, but not motor fibers, to the same extent as lidocaine.51 The different structure of sodium channels, their distribution throughout the nervous system, and the affinity of different local anesthetics for the various channels could account for variability in the results of the DDNB.
The level of the block and its assessment is important, particularly for the abdominal visceral pain, where fibers from visceral organs could synapse over several spinal cord segments. The sensory modalities used are cold pinprick and touch representing signals carried by different classes of nerve fibers. Differential block has been assessed using cutaneous current perception thresholds (CPTs).52 This methodology uses an electrical stimulus to enable a direct quantitative assessment of A-β, A-δ, and C fibers. The authors demonstrated that after a spinal block, the return of the CPTs to baseline occurred sequentially: first, the A-β fiber CPTs returned to baseline, and this correlated with the return of touch sensation; then the return of A-δ fiber CPTs to baseline occurred, and this correlated with the return of sharp pinprick sensation; and, finally, the return of C fiber CPTs to baseline occurred, correlated with the return of cold sensation. They also demonstrated that loss of tolerance to a painful stimulus correlated with the recovery of A-β fiber CPTs to baseline at a time when A-δ and C fiber CPTs were still significantly elevated. Because A-β fibers are not considered to carry nociceptive information, the authors concluded that pain can occur when there is partial recovery of A-δ and C fibers and that “assessing the dermatomal level to touch rather than pinprick may be a more useful predictor of the dermatomal level of the block.”52 These variances, if not recognized, can degrade the accuracy of information that DDNBs provide.
Potentially confounding factors exist such as the improper use of pain scales, problems associated with placebo effects, bias from patient expectations, and observer error. These are thought by some to limit the usefulness of the interpretation of DDNBs.1,6,46 Finally, our concept of pain (especially chronic pain) is constantly evolving as scientific research continues to provide us with new insight. Pain is currently regarded as a predominantly subjective phenomenon with complex physiologic, anatomical, and psychosocial facets that contribute to its totality.3,46 A patient undergoing a DDNB may be motivated by external factors that enter into his or her reporting. Examples cited are reassurance or confirmation of suspicions to persuade doubting family members or the patients themselves or certification of disability for legal or financial gain.46 As such, pain can be difficult to measure from a purely quantitative standpoint. Thus, physicians need to use caution and recognize the potential for misinterpretation of DDNBs to avoid inappropriate therapy.46
Conclusion
Despite their shortcomings, DDNBs continue to be used in clinical practice today.3 A retrospective review of 100 patients with chronic pain who underwent a DDNB after all other diagnostic measures had failed to establish a cause has shown that DDNBs are effective in diagnosing the underlying pain mechanism.53 This same study reports that 74% of the patients studied were unexpectedly found to have an underlying sympathetic mechanism. Had these differential blocks not been performed, it is likely that their pain would have been attributed to a psychogenic mechanism3 and erroneously treated as such. This is true especially because for many of these patients, their chronic pain syndrome have come to manifest as “bizarre” signs and symptoms seemingly “unrelated” to the true underlying cause.3 It is also plausible that had a diagnosis been established and sympathetic blocks performed early on, a more positive outcome would have resulted for these patients.3 Furthermore, recent studies might enhance the role for DDNB in chronic visceral pain.49 However, there remains to be a scarcity of controlled studies supporting or negating the use of DDNBs.46 Additionally, there have been no outcome studies to support any claims that differential blocks lead to the selection of appropriate treatment.1 Thus, it is difficult to make a definitive conclusion given that further studies are needed.
1 Hogan QH, Abram SE. Neural blockade for diagnosis and prognosis. A review. Anesthesiology. 1997;86:216-241.
2 Molloy RE, Candido KD. Diagnostic nerve blocks. In: Benzon H, Raja SN, Molloy R, Liu S, Fishman SM, editors. Essentials of pain medicine and regional anesthesia. ed 2. Philadelphia: Elsevier; 2005:181-189.
3 Winnie AP, Candido KD. Differential neural blockade for the diagnosis of pain. In: Waldman SD, editor. Pain management. Philadelphia: Saunders; 2007:155-166.
4 Pain terms: a list with definitions and notes on usage. Recommended by the IASP Subcommittee on Taxonomy. Pain. 1979;6:249.
5 Heinricher MM, Cheng ZF, Fields HL. Evidence for two classes of nociceptive modulating neurons in the periaqueductal gray. J Neurosci. 1987;7:271-278.
6 Cherry DA, Gourlay GK, McLachlan M, Cousins MJ. Diagnostic epidural opioid blockade and chronic pain: preliminary report. Pain. 1985;21:143-152.
7 McCollum DE, Stephen CR. The use of graduated spinal anesthesia in the differential diagnosis of pain of the back and lower extremities. South Med J. 1964;57:410-416.
8 Ahlgren EW, Stephen CR, Lloyd EA, McCollum DE. Diagnosis of pain with a graduated spinal block technique. JAMA. 1966;195:813-816.
9 Ramamurthy S, Winnie AP. Diagnostic maneuvers in painful syndromes. Int Anesthesiol Clin. 1983;21:47-59.
10 Al-Chaer ED, Traub RJ. Biological basis of visceral pain: recent developments. Pain. 2002;96:221-225.
11 Arner S, Arner B. Differential effects of epidural morphine in the treatment of cancer-related pain. Acta Anaesthesiol Scand. 1985;29:32-36.
12 Hogan Q, Haddox JD, Abram S, et al. Epidural opiates and local anesthetics for the management of cancer pain. Pain. 1991;46:271-279.
13 Arrowood JG, Sarnoff SJ. Differential spinal block; use in the investigation of pain following amputation. Anesthesiology. 1948;9:614-622.
14 Gasser HS, Erlanger J. The role of fiber size in the establishment of a nerve block by pressure or cocaine. Am J Physiol. 1929;88:581-591.
15 Bromage PR. An evaluation of bupivacaine in epidural analgesia for obstetrics. Can Anaesth Soc J. 1969;16:46-56.
16 Greene NM. Area of differential block in spinal anesthesia with hyperbaric tetracaine. Anesthesiology. 1958;19:45-50.
17 Fink BR, Cairns AM. Differential slowing and block of conduction by lidocaine in individual afferent myelinated and unmyelinated axons. Anesthesiology. 1984;60:111-120.
18 Franz DN, Perry RS. Mechanisms for differential block among single myelinated and non-myelinated axons by procaine. J Physiol. 1974;236:193-210.
19 Gissen AJ, Covino BG, Gregus J. Differential sensitivities of mammalian nerve fibers to local anesthetic agents. Anesthesiology. 1980;53:467-474.
20 Fink BR. Mechanisms of differential axial blockade in epidural and subarachnoid anesthesia. Anesthesiology. 1989;70:851-858.
21 Fink BR, Cairns AM. Lack of size-related differential sensitivity to equilibrium conduction block among mammalian myelinated axons exposed to lidocaine. Anesth Analg. 1987;66:948-953.
22 Raymond SA, Strichartz GR. The long and short of differential block. Anesthesiology. 1989;70:725-728.
23 Fink BR, Cairns AM. Lack of size-related differential sensitivity to equilibrium conduction block among mammalian myelinated axons exposed to lidocaine. Anesth Analg. 1987;66:948-953.
24 Beecher HK. The powerful placebo. JAMA. 1955;159:1602-1606.
25 Fink BR, Cairns AM. Differential use-dependent (frequency-dependent) effects in single mammalian axons: data and clinical considerations. Anesthesiology. 1987;67:477-484.
26 Heavner JE, de Jong RH. Lidocaine blocking concentrations for B- and C-nerve fibers. Anesthesiology. 1974;40:228-233.
27 Janig W, Morrison JF. Functional properties of spinal visceral afferents supplying abdominal and pelvic organs, with special emphasis on visceral nociception. Prog Brain Res. 1986;67:87-114.
28 Cervero F. Visceral versus somatic pain: similarities and differences. Dig Dis. 2009;27(suppl 1):3-10.
29 Cervero F. Sensory innervation of the viscera: peripheral basis of visceral pain. Physiol Rev. 1994;74:95-138.
30 Mendelson G, Mendelson D. Malingering pain in the medicolegal context. Clin J Pain. 2004;20(6):423-432.
31 Djouhri L, Lawson SN. Abeta-fiber nociceptive primary afferent neurons: a review of incidence and properties in relation to other afferent A-fiber neurons in mammals. Brain Res Rev. 2004;46:131-145.
32 Djouhri L, Lawson SN. Differences in the size of the somatic action potential overshoot between nociceptive and non-nociceptive dorsal root ganglion neurones in the guinea-pig. Neuroscience. 2001;108:479-491.
33 Lawson SN. Phenotype and function of somatic primary afferent nociceptive neurones with C-, Adelta- or Aalpha/beta-fibres. Exp Physiol. 2002;87:239-244.
34 Liu SS. Local anesthetics: clinical aspects. In: Benzon H, Raja SN, Molloy R, Liu S, Fishman SM, editors. Essentials of pain medicine and regional anesthesia. ed 2. Philadelphia: Elsevier; 2005:558-565.
35 Brau ME, Vogel W, Hempelmann G. Fundamental properties of local anesthetics: half-maximal blocking concentrations for tonic block of Na+ and K+ channels in peripheral nerve. Anesth Analg. 1998;87:885-889.
36 Olschewski A, Hempelmann G, Vogel W, Safronov BV. Blockade of Na+ and K+ currents by local anesthetics in the dorsal horn neurons of the spinal cord. Anesthesiology. 1998;88:172-179.
37 Ford DJ, Raj PP, Singh P, et al. Differential peripheral nerve block by local anesthetics in the cat. Anesthesiology. 1984;60:28-33.
38 Rosenberg PH, Heinonen E, Jansson SE, Gripenberg J. Differential nerve block by bupivacaine and 2-chloroprocaine. An experimental study. Br J Anaesth. 1980;52:1183-1189.
39 Fink BR. Mechanism of differential epidural block. Anesth Analg. 1986;65:325-329.
40 Tasaki I. Nervous transmission. Springfield, IL: CC Thomas; 1953. p 164
41 Fink BR, Cairns AM. Lack of size-related differential sensitivity to equilibrium conduction block among mammalian myelinated axons exposed to lidocaine. Anesth Analg. 1987;66:948-953.
42 de Jong RH. Differential nerve block. In: Local Anesthetics. St. Louis: Mosby; 1994. p 84
43 Lorente de No R, Condouris GA. Decremental conduction in peripheral nerve. Integration of stimuli in the neuron. Proc Natl Acad Sci U S A. 1959;45:592-617.
44 Folkow B. Impulse frequency in sympathetic vasomotor fibres correlated to the release and elimination of the transmitter. Acta Physiol Scand. 1952;25:49-76.
45 Raj PP: Sympathetic pain mechanisms and management. Second Annual Meeting of the American Society of Regional Anesthesia, Hollywood, FA 10-11 March 1977.
46 Raja SN. Nerve blocks in the evaluation of chronic pain. Anesthesiology. 1997;86:4-6.
47 Cousins MJ, Glynn CJ. New horizons. In: Cousins MJ, Bridenbaugh PO, editors. Neural blockade in clinical anesthesia and management of pain. Philadelphia: Lippincott; 1980:699-719.
48 Rawal N, Schott U, Dahlstrom B, et al. Influence of naloxone infusion on analgesia and respiratory depression following epidural morphine. Anesthesiology. 1986;64:194-201.
49 Conwell DL, Vargo JJ, Zuccaro G, et al. Role of differential neuroaxial blockade in the evaluation and management of pain in chronic pancreatitis. Am J Gastroenterol. 2001;96:431-436.
50 Fink BR, Cairns AM. Lack of size-related differential sensitivity to equilibrium conduction block among mammalian myelinated axons exposed to lidocaine. Anesth Analg. 1987;66:948-953.
51 Scholz A, Kuboyama N, Hempelmann G, Vogel W. Complex blockade of TTX-resistant Na+ currents by lidocaine and bupivacaine reduce firing frequency in DRG neurons. J Neurophysiol. 1998;79:1746-1754.
52 Liu S, Kopacz DJ, Carpenter RL. Quantitative assessment of differential sensory nerve block after lidocaine spinal anesthesia. Anesthesiology. 1995;82:60-63.
53 Winnie AP, Collins VJ. The pain clinic. I. Differential neural blockade in pain syndromes of questionable etiology. Med Clin North Am. 1968;52:123-129.