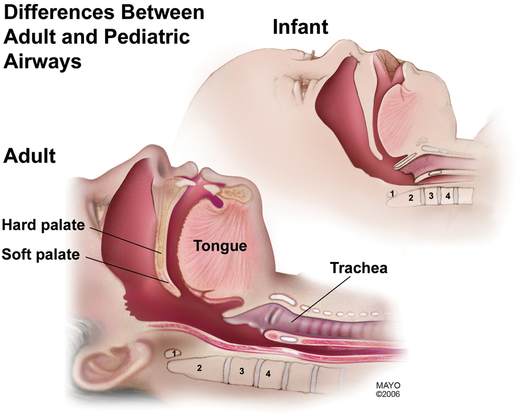
Differences between the infant and adult airway
The infant airway differs from the adult airway in structure and in functionality (Figure 192-1). Understanding these differences is important for airway management and, when necessary, for successful tracheal intubation of neonatal, infant, and pediatric airways.
Tracheal tube
Size and type
Choosing the correct size of tracheal tube in infants and children is dependent upon the size of the child. Table 192-1 gives some approximate tracheal tube sizes used in infants and children. The presence of an air leak around the tracheal tube is critically important in preventing postintubation edema of the trachea. An air leak should be present at less than 30 cm H2O peak inflation pressure (the approximate capillary pressure of the tracheal mucosa). If it is not, then the tube should be replaced with the next half-size smaller. Airway resistance is inversely proportional to the radius of the lumen to the fourth power for laminar flow. Therefore, in an infant airway, 1 mm of edema will obstruct the airway by more than 40%, according to the law of Poiseuille.
Table 192-1
| Age | Size |
| Premature (<2.5 kg) | 2.5 |
| Term neonate | 3.0 |
| 2-8 months | 3.5 |
| 8-12 months | 4.0 |
| 18-24 months | 4.5 |
| Older than 24 months | (Age in years/4) + 4 |