Chapter 1 Design and organisation of intensive care units
An intensive care unit (ICU) is a specially staffed and equipped area of a hospital dedicated to the management of patients with life-threatening illnesses, injuries or complications. ICUs developed from the postoperative recovery rooms and respiratory units of the 1920s, 1930s and 1940s when it became clear that concentrating the sickest patients in one area was beneficial. Intermittent positive-pressure ventilation (IPPV) was pioneered in the treatment of respiratory failure in the 1948–1949 poliomyelitis epidemic and particularly in the 1952 Copenhagen poliomyelitis epidemic when IPPV was delivered using an endotracheal tube and a manual bag.1 Subsequently mechanical ventilators were developed and became increasingly used for the treatment of thoracic surgery, general surgery, tetanus and ‘crushed chests’.
As outlined below, the ICU is not just a ward but a department with dedicated medical, nursing and allied health staff: it operates with defined policies and procedures and has its own quality improvement, continuing education and research programmes. Through its care of critically ill patients in the ICU and its outreach activities (see Chapter 2), the intensive care department provides an integrated service to the hospital, without which many programmes (e.g. cardiac surgery, trauma, transplantation) could not function.
CLASSIFICATION AND ROLE DELINEATION OF AN ICU
The delineation of roles of hospitals in a region or area is necessary to rationalise services and optimise the use of resources. Each ICU should similarly have its role in the region defined and should support the defined duties of its hospital. In general, small hospitals require ICUs that provide basic intensive care. Critically ill patients who need complex management and sophisticated investigative back-up should be managed in an ICU located in a large tertiary referral hospital. Three levels of adult ICUs are classified as follows by the Joint Faculty of Intensive Care Medicine (Australia and New Zealand).2 The European Society of Intensive Care Medicine has a similar classification.3 The American College of Critical Care Medicine also has a similar classification but uses a reversed-numbering system.4 It should be noted that full-time directors and directors with qualifications in intensive care medicine are less common in the USA,5 as are the requirement for a dedicated doctor for the ICU around the clock and referral to the attending ICU specialist for management.6
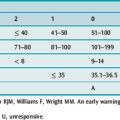
The classification of types of ICU must not be confused with the description of critical care beds throughout a hospital, as with the UK classification of critical care beds (Table 1.1).
| Level 0 |
| Patients whose needs can be met through normal ward care in an acute hospital |
| Level I |
| Patients at risk of their condition deteriorating, or those recently relocated from higher levels of care whose needs can be met on an acute ward with additional advice and support from the critical care team |
| Level II |
| Patients requiring more detailed observation or intervention, including support for a single failing organ system or postoperative care, and those stepping down from higher levels of care |
| Level III |
| Patients requiring advanced respiratory support alone or basic respiratory support together with support of at least two organ systems. This level includes all complex patients requiring support for multiorgan failure (http://www.ics.ac.uk/icmprof/downloads/icsstandards-levelsofca.pdf) |
TYPE AND SIZE OF AN ICU2
The number of ICU beds in a hospital usually ranges from 1 to 4 per 100 total hospital beds. This depends on the role and type of ICU. Multidisciplinary ICUs require more beds than single-specialty ICUs, especially if high-dependency beds are integrated into the unit. ICUs with fewer than four beds are considered not to be cost-effective and are too small to provide adequate clinical experience for skills maintenance for medical and nursing staff. On the other hand, the emerging trend of ICUs having 267 or more beds creates major management problems. Although the evidence is scant, there is a suggestion that efficiency deteriorates once the number of critically ill patients per medical team exceeds 12.8 Consequently two or more medical teams may need to work together in these ‘mega-units’.
HIGH-DEPENDENCY UNIT (HDU)9,10
The HDU provides invasive monitoring and support for patients with or at risk of developing acute (or acute on chronic) single-organ failure, particularly where the predicted risk of clinical deterioration is high or unknown. It may act as a ‘step-up’ or ‘step-down’ unit between the level of care delivered on a general ward and intensive care, but does not normally accept patients requiring mechanical ventilation. Several older studies have shown benefits to outcome associated with the introduction of HDUs,9 whereas a more recent study has questioned these findings.11
PAEDIATRIC ICU (PICU)2
A PICU is a separate area in the hospital capable of providing complex, multisystem life support for indefinite periods to infants and children less than 16 years of age. It is a tertiary referral centre for children needing intensive care and has extensive back-up laboratory and clinical services to support this tertiary role. Consultants in a PICU are paediatric intensive care specialists with expertise different from their adult intensive care colleagues. All patients admitted to the PICU are referred to the attending PICU specialists for management.
DESIGN OF AN ICU1,3,12
STORAGE AND SUPPORTING SERVICES AREAS
Floor areas for supporting services should make up about 20–25% of the patient and central station areas. Utility rooms must be clean and separate, each with its own access. Disposal of soiled linen and waste must be catered for, including contaminated items from infectious patients, using one-way traffic schemes. Facilities for estimating blood gases, glucose, electrolytes, haemoglobin, lactate and sometimes clotting status are usually sufficient for the unit’s laboratory. There should be a pneumatic tube or other system to transfer specimens to pathology. A good communication network of phones/intercoms is vital to locate and inform staff quickly. Adequate arrangements for offices, doctor-on-call rooms, staff lounge (with food/drinks facilities), wash rooms, education (seminar room) and a waiting room (see below) complete the unit.
STAFFING2–5
The level of staffing depends on the type of hospital and a tertiary hospital ICU requires a large team. Whatever the size of the team, it is crucial that there is free communication and collaboration among team members and a true multidisciplinary approach. Knaus et al. in a classic study13 first showed a relationship between the degree of coordination in an ICU and the effectiveness of its care. Other studies have shown relationships between collaboration and teamwork and better outcomes for patients and staff.14,15 Inadequate communication is the most frequent root cause of sentinel events.16
MEDICAL STAFF17
The director should be supported by a group of other specialists trained in intensive care medicine who provide patient care and contribute to non-clinical activities. In an ICU of level II or III there must be at least one specialist exclusively rostered to the unit at all times. Specialists should have a significant or full-time commitment to the ICU ahead of clinical commitments elsewhere. There should be sufficient numbers to allow reasonable working hours, protected non-clinical time and leave of all types. The recent increase in ICU outreach activities (medical emergency team calls, outpatient review: see Chapter 2) has increased the workload of intensive care specialists as well as junior staff in many hospitals, resulting in the need to increase the size of the medical team.
This physician staffing model has been used in Australia and New Zealand for many years, but has not been common in the USA. A systematic review18 has shown that when there has been mandatory intensivist consultation (or closed ICU – see below) compared with no or elective intensivist consultation or open ICU, both ICU and hospital survival were improved and there was a reduced length of stay in ICU and in hospital.
NURSING STAFF
Critical care nursing is covered in Chapter 6. The bedside nurse conducts the majority of patient assessment, evaluation and care in an ICU. In ICUs supporting tertiary hospitals 1:1 nursing is required for all ventilated patients, whereas one nurse per two patients is appropriate for HDU patients. Some complex patients with multiple supports may require more than one nurse. When leave of all kinds is factored in, long-term 24-hour cover of a single bed requires a staff complement of six nurses. Nurse shortages have been shown to be associated with increased patient mortality and nurse burnout and adversely affect outcome and job satisfaction in the ICU.19,20
ALLIED HEALTH
Major ICUs must have 24-hour access to pathology and radiological services. Access to physiotherapists, dieticians, social workers and other therapists should also be available. A dedicated ward clinical pharmacist is invaluable and participation of a pharmacist on ward rounds has been associated with a reduction in adverse drug events.21 Respiratory therapists are allied health personnel trained in and responsible for the equipment and clinical aspects of respiratory therapy, a concept well established in North America, but not the UK, continental Europe and Australasia. Technical support staff,22 either as members of the ICU staff, or seconded from biomedical departments, are necessary to service, repair and develop equipment.
OTHER STAFF
Provision should be made for adequate secretarial support.23 Transport and ‘lifting’ orderly teams will reduce physical stress and possible injuries to nurses and doctors. If no mechanical system is available to transport specimens to the laboratories (e.g. air-pressurised chutes), sufficient and reliable couriers must be provided to do this day and night. The cleaning personnel should be familiar with the ICU environment and infection control protocols. There should also be a point of contact for local interpreters, chaplains, priests or officials of all religions, when there is need for their services.
CLINICAL ACTIVITIES
OPERATIONAL POLICIES2
Clear-cut administrative policies are vital to the functioning of an ICU. An open ICU has unlimited access to multiple doctors who are free to admit and manage their patients. A closed ICU has admission, discharge and referral policies under the control of intensivists. Improved cost benefits are likely with a closed ICU and patient outcomes are better, especially if the intensivists have full clinical responsibilities.18,24 Consequently ICUs today, especially levels II and III, should be closed under the charge of a medical specialist director. All patients admitted to the ICU are referred to the director and his/her specialist staff for management, although it is important for the ICU team to communicate regularly with the parent unit and to make referrals to specialised services when appropriate.
Policies for the care of patients should be formulated and standardised. They should be unambiguous, periodically reviewed and familiarised by all staff. Examples include infection control and isolation policies, policies for intra- and interfacility transport, end-of-life policies (e.g. do not resuscitate (DNR) procedure) and sedation and restraint protocols. It should be noted, however, that when protocols involve complex issues (such as weaning from mechanical ventilation) they may be less efficient than the judgement of experienced clinicians.25 Clinical management protocols, e.g. for feeding and bowel care, can be laminated and placed in a folder at each bed or loaded on to the intranet.
PATIENT CARE
ICU patient management should be multidisciplinary, with medical, nursing and other staff working together to provide the best care for each patient. The critical care nurse is the primary carer at the bedside and monitors, manages and supports the critically ill patient (see Chapter 6). The medical team consists of one or more registrars, residents or fellows who direct medical care with an intensive care specialist. The patient should be assessed by a formal ward round of the multidisciplinary team twice daily, usually at a time when the junior medical staff are handing over from one shift to the next. The nurse coordinating the floor and in larger units allied health staff such as pharmacists and dieticians also take part. Each patient should be assessed clinically (examination, observations and pathology, radiological and other investigation results), the medication chart reviewed, progress determined and a management plan developed for the immediate and longer term. The ward round is also an opportunity to assess compliance with checklists such as Fast Hug.26 Clearly, unstable patients will require much more frequent assessment and intervention.
Wherever possible clinical management should be evidence-based and derived through consensus of the members of the ICU team, accepting, however, that evidence-based medicine has limitations when applied to intensive care medicine.27
CARE OF FAMILIES28
ICU care includes sensitive handling of relatives. It is important that there are early and repeated discussions with patients’ families to reduce family stress and improve consistency in communication. Ideally one senior doctor should be identified as the ICU representative to liaise with a particular family. Discussions should be interactive and honest and an attempt made to predict the likely course, especially with respect to outcome, potential complications and the duration of intensive care management required. The time, date and discussion of each interview should be recorded. Cultural factors should be acknowledged and spiritual support available, especially before, during and after a death. Open visiting hours allow families maximum contact with their loved one and promote an atmosphere of openness and transparency.
NON-CLINICAL ACTIVITIES2
Non-clinical activities are very important in the ICU, as they enhance the safety, quality and currency of patient care. The Joint Faculty of Intensive Care Medicine recommends that full-time intensive care specialists should have as protected non-clinical time three half-day sessions per week.29 Nursing and allied health staff should also seek protected time for these activities.
QUALITY IMPROVEMENT30,31
Quality indicators can be considered under three headings:
The QI process involves identification of the indicator to be improved (e.g. high ventilator-associated pneumonia (VAP) rate), development of a method to improve it (e.g. checklist such as Fast Hug26), implementation of the method to improve it (e.g. requrement to tick off the checklist on the morning ward round), re-evaluation of the indicator (e.g. VAP rate) to ensure the intervention has improved the outcome and finally to ensure sustainability (e.g. print checklist on ICU chart).
Activities that assess outcomes are calculating risk-adjusted mortality using a scoring system such as the Acute Physiology and Chronic Health Evaluation II (APACHE II) and calculation of standardised mortality ratios (see Chapter 3), measurement of rates of adverse events such as central venous catheter-associated blood stream infection rate or serious adverse drug event rate and surveys (e.g. patient or relative satisfaction, bad backs from lifting in ICU nurses).
Risk management is a closely related field. In the ICU, risks can be identified from critical incident reports, morbidity and mortality reviews and complaints from staff, patients or family members. Using similar methodology to the QI process risks must be identified, assessed and analysed, managed and re-evaluated. A major patient safety incident should result in a root cause analysis.32
EDUCATION
All ICUs should have a documented orientation programme for new staff. There should be educational programmes for medical staff and a formal nursing education programme. Educational activities for intensive care trainees include lectures, tutorials, bedside teaching and trial examinations (written, clinical and viva). Apart from clinical reviews, meetings to review journals and new developments should be held regularly. Nurses are usually required to undergo annual assessment for advanced life support and sometimes other assessments (e.g. medication safety). Increasingly, simulation centres are used to teach and assess skills and teamwork in crisis scenarios.33 A number of ICUs are also involved in undergraduate medical teaching. All staff should also participate in continuing education activities outside the hospital (e.g. local, national or international meetings).
THE FUTURE
In the USA critical care medicine is thought to account for 1–2% of the gross domestic product34 and has become increasingly used and prominent in the delivery of health care. Although the total number of hospitals, hospital beds and inpatient days has decreased, there has been shown to be a large increase in the number of intensive care beds and bed days.35 There is every reason to expect that other developed countries will follow this trend. As ICUs become larger and ICU staff become larger still (because of outreach activities: see Chapter 2) it is crucial that the basic principles outlined in this chapter are followed and that standards of ICU design, staffing and clinical and non-clinical activities are maintained.
1 Trubuhovich R. On the very first, long-term, large-scale use of IPPV. Albert Bower and V Ray Bennett: Los Angeles, 1948–1949. Crit Care Resusc. 2007;9:91-100.
2 Minimum Standards for Intensive Care Units. Melbourne: Joint Faculty of Intensive Care Medicine, 2003. Policy document IC-1
3 Ferdinande P. Members of the Task Force of the European Society of Intensive Care Medicine. Intens Care Med. 1997;23:226-232.
4 Haupt MT, Bekes CE, Brilli RJ, et al. Guidelines on critical care services and personnel: recommendations based on a system of categorization of three levels of care. Crit Care Med. 2003;31:2677-2683.
5 Brilli RJ, Spevetz A, Branson R, et al. Critical care delivery in the intensive care unit: defining clinical roles and the best practice model. Crit Care Med. 2001;29:2007-2019.
6 Angus DC, Shorr AF, White A, et al. Critical care delivery in the United States: distribution of services and compliance with the Leapfrog recommendations. Crit Care Med. 2006;34:1016-1024.
7 Martin J, Anderson T, Turton C, et al. Intensive Care Resources and Activity: Australia and New Zealand 2003–2005. Melbourne: ANZICS, 2006.
8 Dara SI, Afessa B. Intensivist-to-bed ratio: association with outcomes in the medical ICU. Chest. 2005;128:567-572.
9 Boots R, Lipman J. High dependency units: issues to consider in their planning. Anaesth Intens Care. 2002;30:348-354.
10 Minimum Standards for High Dependency Units Seeking Accreditation for Training in Intensive Care. Melbourne: Joint Faculty of Intensive Care Medicine, 2000. Policy document IC-13
11 Bellomo R, Goldsmith D, Uchino J, et al. A before and after trial of the effect of a high-dependency unit on post-operative morbidity and mortality. Crit Care Resusc. 2005;7:16-21.
12 Society of Critical Care Medicine. Guidelines for intensive care unit design. Crit Care Med. 1995;23:582-588.
13 Knaus WA, Draper EA, Wagner DP, et al. An evaluation of outcome from intensive care in major medical centers. Ann Intern Med. 1986;104:410-418.
14 Baggs JG, Schmitt MH, Mushlin AI, et al. Association between nurse–physician collaboration and patient outcomes in three intensive care units. Crit Care Med. 1998;27:1991-1998.
15 Reader TW, Flin R, Mearns K, et al. Interdisciplinary communication in the intensive care unit. Br J Anaesth. 2007;98:347-352.
16 Joint Commission on Accreditation of Health Care Organizations (JCAHO). Statistics: Root Cause Statistics – Root Causes of Sentinel Events (All Categories). Oakbrook Terrace, Ill: JCAHO, 2005.
17 The Duties of an Intensive Care Specialist in Hospitals Accredited for Intensive Care Training. Melbourne: Joint Faculty of Intensive Care Medicine, 2000. Policy document IC-2
18 Pronovost PJ, Angus DC, Dorman T, et al. Physician staffing patterns and clinical outcomes in critically ill patients. JAMA. 2002;288:2151-2162.
19 Tarnow-Mordi W, Hau C, Warden A, et al. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive care unit. Lancet. 2000;356:185-189.
20 Ulrich BT, Lavandero R, Hart KA, et al. Critical care nurses’ work environments: a baseline status report. Crit Care Nurse. 2006;26:46-57.
21 Leape LL, Cullen DJ, Demspey Clapp M, et al. Pharmacist participation in physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282:267-270.
22 Carter BG, Kiraly N, Hochmann N, et al. ICU staffing: identification and survey of staff involved in providing technical services to Australian and New Zealand intensive care units. Anaesth Intens Care. 2007;35:259-265.
23 Administrative Services to Intensive Care Units. Melbourne: Joint Faculty of Intensive Care Medicine, 2006. Policy document IC-7
24 Hanson CW, Deutschman CS, Anderson HL, et al. Effects of an organised critical care service on outcomes and resource utilization: a cohort study. Crit Care Med. 1999;27:270-274.
25 Krishnan JA, Moore D, Robeson C, et al. A prospective, controlled trial of a protocol-based strategy to discontinue mechanical ventilation. Am J Respir Crit Care Med. 2004;169:673-678.
26 Vincent JL. Give your patient a fast hug (at least) once a day. Crit Care Med. 2005;33:1225-1229.
27 Vincent JL. Evidence-based medicine in the ICU: important advances and limitations. Chest. 2004;126:592-600.
28 Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for the support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Crit Care Med. 2007;35:605-622.
29 Joint Faculty of Intensive Care Medicine. Intensive Care Specialist Practice in Hospitals Recognised for Training in Intensive Care Medicine IC-2. Available online at JFICM australia http://www.anzca.edu.au/jficm/resources/policy/IC-2-2005.pdf
30 Curtis JR, Cook DJ, Wall RJ, et al. Intensive care quality improvement: a ‘how-to’ guide for the interdisciplinary team. Crit Care Med. 2006;34:211-218.
31 Quality Assurance. Melbourne: Joint Faculty of Intensive Care Medicine, 2000. Policy document IC-8
32 Batty L, Holland-Elliot K, Rosenfeld D. Investigation of eye splash and needlestick incidents from an HIV-positive donor on an intensive care unit using root cause analysis. Occup Med. 2003;53:147-150.
33 Hammond J. Simulation in critical care and trauma education and training. Curr Opin Crit Care. 2004;10:325-329.
34 Gipe BT. Financing critical care medicine in 2010. N Horiz. 1999;7:184-197.
35 Halpern NA, Pastores S, Greenstein RJ. Critical care medicine in the United States 1985–2000: an analysis of bed numbers, use and costs. Crit Care Med. 2004;32:1249-1259.