CHAPTER 4 Basic dental and oral local anaesthesia
Dental pain is best managed by a dentist because a dentist knows about teeth and most doctors do not. They can also provide definitive care in an appropriate setting with the correct instruments. Dentists are often not available, however, so patients with toothache or dental injuries often present to the ED for pain relief. Although conventional analgesics are effective, performing a nerve block with a long-acting local anaesthetic will make the patient your friend for life. Dental blocks are also a good choice for pregnant women because local anaesthetics and adrenaline (epinephrine) are not teratogenic and can be administered safely without systemic side effects, if used correctly.
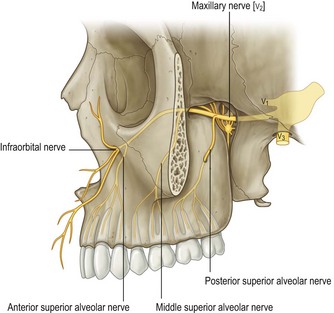
The maxillary dentition receives innervation from the maxillary branch of the trigeminal nerve (anterior, middle and posterior superior alveolar nerves, palatine nerves), and the mandibular dentition from the mandibular division of the trigeminal nerve (inferior alveolar nerve, accessory innervation).
Local anaesthesia for the maxillary dentition
Supraperiosteal or infiltration local anaesthesia
The maxillary teeth are innervated via a network of nerves originating from the maxillary nerve and the infraorbital nerve (Fig. 4.1). These nerves run in the cancellous bone of the maxilla, superior to the roots of the maxillary teeth. The lateral cortical plate of the maxillary alveolus is usually sufficiently thin and porous to allow for effective infiltration (supraperiosteal) local anaesthesia. This technique is not recommended for more than two adjacent teeth or when local infection or inflammation is present. To accomplish this, local anaesthetic is infiltrated along the buccal-gingival fold adjacent to the area to be blocked (e.g. adjacent to the first molar if that tooth is painful from infection or injury).
Technique
•
Identify the target area for needle insertion – the apex of the buccal-gingival fold adjacent to the target tooth or teeth.
•
Dry the mucosa of the target area and apply topical anaesthesia with a cotton bud. Use lidocaine 4% gel or any other topical anaesthetic (improvising with an ester such as tetracaine, which can usually be found amongst the ophthalmic medications, works extremely well).
•
Wait 30 seconds for the topical anaesthesia to take effect. To reduce the pain of injection, lift the lip, pull it taut and shake it as the needle is inserted.
•
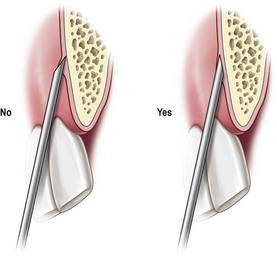
Align the syringe parallel to the long axis of the tooth. With the bevel facing the bone, insert the needle into the target area and advance the needle until the bevel is at or beyond the apex of the tooth (usually just a few millimetres) (
Fig. 4.2). There should be no resistance or patient discomfort during this procedure.
•
If two teeth need to be blocked, insert the needle of the syringe parallel to the maxillary buccal mucogingival line (where the cheek mucosa reflects onto the gum) opposite the teeth to be anaesthetised (
Fig. 4.3).
•
Aspirate, and if there is no flashback of blood, inject about 2 to 4 mL of local anaesthetic slowly over 30 to 60 seconds, and continue whilst slowly withdrawing the needle.
•
The patient should experience numbness within 2 to 5 minutes of injection. Failure to reach the apex of the tooth when injecting anaesthetic results in varying degrees of soft-tissue numbness without anaesthesia of the tooth itself. If the first attempt at infiltration fails to provide adequate pain relief, the procedure can safely be repeated several times provided that the total amount of local anaesthetic injected is within the recommended limits.
•
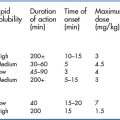
Lidocaine provides about 1 hour of dental analgesia and 3 to 5 hours of soft-tissue analgesia. For temporary relief of pain in the ED, the preferred agent is 0.5% bupivacaine or 0.5% ropivacaine with 1:200 000 adrenaline. This provides 1 to 3 hours of dental analgesia and 4 to 9 hours of soft-tissue analgesia. The duration of analgesia is less with supraperiosteal infiltration than with regional nerve blocks. The onset of analgesia is within 3 to 10 minutes, depending on which agent is used.
Tips for the non-dentist
•
The orientation of the bevel is important in order to decrease the pain of injection and to control the deflection of the needle. When infiltrating, it is better to orientate the bevel towards the bone to avoid scraping the periosteum (
Fig. 4.4). It is also important to remember, especially with nerve blocks, that the tip of the needle is deflected away from the side of the bevel as it passes through the tissues. This may amount to as much as 4 mm of deflection in a 30G needle inserted 25 mm into the tissues.
•
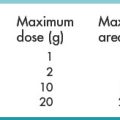
One cartridge of local anaesthetic (1.8 to 2 mL) is sufficient in dental anaesthesia to provide anaesthesia to most areas. Larger volumes injected over a larger area increase the likelihood of successful anaesthesia, however, especially for the non-expert. The disadvantage of this is the potential for toxic effects of the local anaesthetic and maximum doses should be carefully calculated and observed.
•
If local infiltration is ineffective for the maxillary tooth or teeth, a nerve block might be required. An infraorbital nerve block will anaesthetise the anterior superior alveolar nerve which innervates the anterior maxillary teeth and a posterior superior alveolar nerve block will anaesthetise the maxillary molars.
•
Avoid using a standard dental syringe: it is impossible to aspirate using these syringes. Use a conventional syringe with the smallest readily available needle of appropriate length (often a 23G 40-mm needle).
Intraoral infraorbital nerve block
This block provides excellent anaesthesia for pain involving the upper teeth from the midline to the canine or for lacerations involving the upper lip. It also anaesthetises the maxillary premolars and part of the root of the first maxillary molar in about 70% of patients.
The infraorbital foramen can easily be identified using ultrasound to establish its exact position.
Technique
•
Locate the infraorbital foramen, which is about 10 mm inferior to the infraorbital notch (the zygomaticomaxillary suture) and about 25 mm lateral to the midline of the face. The patient might experience some discomfort when palpating over the foramen.
•
Identify the target area for needle insertion – the apex of the buccal-gingival fold directly adjacent to the first maxillary premolar.
•
Dry the mucosa and apply topical anaesthetic.
•
Keep your index finger over the infraorbital foramen and lift the lip, pull the tissue taut and shake the lip while inserting the needle, to minimise the pain of injection.
•
Keep the syringe parallel to the long axis of the first premolar and direct the needle toward the finger over the infraorbital notch and the infraorbital foramen (
Fig. 4.5); keep close to the periosteum to avoid the facial artery.
•
Slowly advance the needle until it meets bone (about 10 to 15 mm in an adult), about 10 mm below the inferior orbital margin; do not attempt to enter the infraorbital foramen – this might lead to intraneural injection and further complications.
•
Aspirate. If there is no flashback of blood, slowly inject 2 to 5 mL of local anaesthetic.
•
If blood is aspirated, withdraw the needle by 5 mm and slightly redirect it while advancing.
•
The patient should experience anaesthesia within about 5 minutes of injection.
Posterior superior alveolar nerve block
This nerve block is the preferred alternative to supraperiosteal injection for the maxillary molars when more than two teeth are involved or when infiltration anaesthesia fails or is contraindicated. The block anaesthetises the second and third maxillary molars and, in about 70% of patients, the entire first molar. In the remaining 30% of patients, the posterior superior alveolar nerve innervates all but one root of the first maxillary molar; these patients can be given a supplemental supraperiosteal injection following the block or an infraorbital nerve block if necessary. This block is highly effective but carries a greater risk of intravascular injection and haematoma formation than most other dental blocks. Frequent aspiration is essential during the procedure, so a needle no smaller than 25G is recommended.
Technique
•
Identify the target area for needle insertion – the apex of the buccal-gingival fold adjacent to the second maxillary molar.
•
Dry the mucosa and apply topical anaesthetic.
•
Ask the patient to open their mouth and to move their jaw toward the affected side to create more room.
•
Retract the patient’s cheek on the side being injected, pull the tissue taut and shake it while inserting the needle.
•
Puncture the mucosa at the target area with the syringe aligned with the long axis of the second maxillary molar (
Fig. 4.6).
•
Advance the needle medially (at a 45° angle) and posteriorly (at a 45° angle to the long axis of the second maxillary molar) to a depth of about 15 mm.
•
If bone is contacted, the needle has been directed too medially and should be redirected more laterally.
•
Aspirate once, then rotate the syringe by 90° and aspirate again. If there is no flashback of blood, inject 2 to 5 mL of local anaesthetic over 30 to 60 seconds while aspirating periodically during the injection.
•
If blood is aspirated, withdraw the needle and redirect it more medially and superiorly.
•
Complications (most importantly bleeding) most often result from a needle inserted too deep. If the local anaesthetic was injected with a too shallow needle insertion, adequate anaesthesia may still be attained: too shallow is preferable to too deep with this block.
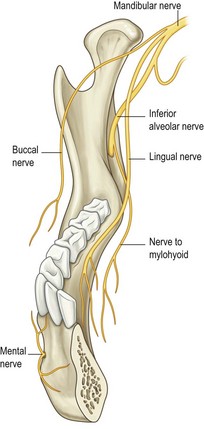
Local anaesthesia for the mandibular dentition (Fig. 4.7)
Supraperiosteal or infiltration local anaesthesia
This is generally not effective for the mandibular teeth because the thick bony cortex of the mandible is impermeable to local anaesthetic. Nerve block anaesthesia is therefore usually necessary for adequate anaesthesia and analgesia of the lower teeth.
Inferior alveolar nerve block
The inferior alveolar nerve block provides anaesthesia for all the ipsilateral mandibular teeth, the anterior two-thirds of the tongue, and the skin and soft tissue innervated by the mental nerve, and is useful to provide anaesthesia for dental pain and for laceration repair of the anterior tongue and floor of the mouth. The complication rate and failure rate are slightly higher with this block than with some of the other dental blocks. Patients should be warned to avoid self-injury because of the anaesthesia of the lips and tongue.
Technique
•
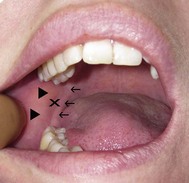
Identify the target area for needle insertion – the area between the pterygomandibular fold and the anterior border of the ramus about 10 mm superior to the occlusal plane of the mandibular teeth (
Fig. 4.8).
•
Apply a topical anaesthetic to this area.
•
Insert your thumb into the patient’s mouth and place it on the coronoid notch with your index finger just anterior to the ear.
•
Retract the cheek laterally to maximise visibility and to decrease the pain of the injection.
•
Introduce the needle medial to the centre of your thumb 10 mm above and parallel to the mandibular occlusal plane (
Fig. 4.9A).
•
Swing the syringe so that the barrel is in the opposite corner of the mouth, resting on the premolars (
Fig. 4.9B).
•
Aim toward your index finger and slowly advance the needle until the bone is contacted, usually a distance of about 25 mm.
•
If the needle does not contact bone, redirect the needle more laterally.
•
Withdraw the needle 1 mm and aspirate, then rotate the syringe 90° and re-aspirate.
•
If there is no flashback of blood, slowly inject 5 mL of local anaesthetic.
•
If blood is aspirated, withdraw the needle about 5 mm and reposition it.
•
Inject another 2 mL of local anaesthetic while withdrawing the needle.
•
If the injection fails to result in adequate analgesia, it can safely be repeated unless the maximum dose of local anaesthetic has been reached.
Intraoral mental nerve block
This is a straightforward, highly successful technique that numbs the mandibular buccal soft tissues from the midline to the second premolar and the skin of the chin and lower lip. It is ideal for patients with trauma to this area who require debridement or laceration repair. The use of a nerve block rather than local infiltration of anaesthetic is particularly advantageous when the laceration involves a cosmetically important structure, such as the vermilion border of the lip, as there is no tissue distortion. The position of the mental foramen is variable but is usually 8 mm superior to the inferior border of the mandible on a line between the premolars or in line with the second premolar; occasionally it is opposite the first molar.
The mental foramen can be identified using ultrasound to establish its exact position.
Technique
•
Dry the mucosa and apply topical anaesthetic to the buccal-gingival fold opposite the second premolar.
•
Retract, stretch and shake the lower lip to facilitate a painless injection.
•
Introduce the needle parallel to the long axis of the second premolar into the target area (
Fig. 4.10).
•
Advance the needle about 5 mm.
•
Aspirate. If there is no flashback of blood, slowly inject 5 mL of local anaesthetic.
•
If blood is aspirated, withdraw and redirect the needle.
•
The patient should experience complete anaesthesia within about 5 minutes of injection.
•
If anaesthesia is not successful, reattempt injection slightly posterior to the initial target point.
Lingual nerve block
The lingual nerve supplies sensation to the anterior two-thirds of the tongue and the floor of the mouth. The lingual nerve is often blocked during the inferior alveolar nerve block but may be blocked separately if required. The lingual nerve is a branch of the mandibular nerve and runs in the submucosa medial to the mandibular molars.
Technique
•
Identify the target point for needle insertion – the floor of the mouth medial to the third molar.
•
Dry the mucosa and apply topical anaesthetic.
•
Insert the needle as vertically as possible and advance it about 5 mm (
Fig. 4.11).
•
Aspirate. If there is no flashback of blood, slowly inject 5 mL of local anaesthetic.
•
If blood is aspirated, withdraw and reposition the needle before re-aspirating.
Long buccal nerve block
The long buccal nerve supplies some sensation to the anterior mandibular teeth and an area of the cheek lateral to that supplied by the infraorbital nerve (superior to the labial angle, extending laterally towards the zygoma). It crosses the ramus of the mandible at the level of the maxillary occlusal plane from medial to lateral and runs in the submucosa lateral to the molars.
Technique
•
Identify the target point for needle insertion – the buccal-gingival fold lateral to the first molar (
Fig. 4.12A).
•
Dry the mucosa and apply topical anaesthetic.
•
Insert the needle parallel to the long axis of the molar and advance it about 5 mm.
•
Aspirate. If there is no flashback of blood, slowly inject 5 mL of local anaesthetic.
•
If blood is aspirated, remove the needle and reposition it.
An alternative method is to block the nerve where it crosses the ramus of the mandible (Fig. 4.12B):
•
Identify the target point for needle insertion – the pterygomandibular fold at the level of the maxillary occlusal plane.
•
Insert the needle and advance it directly posteriorly until the bone is contacted, then withdraw the needle by 1 mm.
•
Aspirate. If there is no flashback of blood, slowly inject 5 mL of local anaesthetic.
•
If blood is aspirated, withdraw the needle by 5 mm and reposition it.
Local and Regional Anaesthesia in the Emergency Department Made