17 Delirium and Acute Encephalopathies
Clinical Vignette
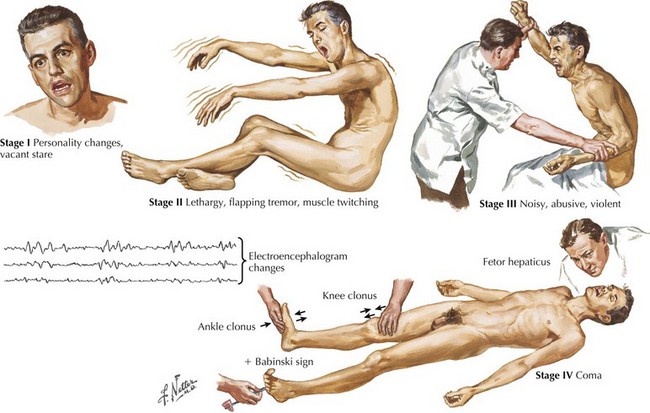
Delirium is a common, acquired neuropsychiatric disorder frequently encountered in clinical practice. Marked by cognitive and behavioral symptoms and a fluctuating course, delirium presents doctors and families with a host of challenges, from initial diagnosis and management, to ethical dilemmas surrounding informed consent, personal autonomy, and patient safety (Fig. 17.1). There is a lack of consensus regarding the definition and terminology pertaining to delirium. Terms such as “acute confusional state,” “encephalopathy,” and “change in mental status” are often used arbitrarily. As delirium often presents within the context of myriad medical and/or surgical conditions, it is often not appreciated to be a clinically independent entity. Nevertheless, delirium is associated with considerable morbidity and mortality, delaying or interfering with proper care as well as promoting great distress for nursing staff, physicians, and families.
Definition
Diagnosis
Evaluation
Various disorders need to be considered in the differential diagnosis of the delirious patient. In order to differentiate delirium from dementia, there are some very simple means (Table 17-1). These include the following:
Table 17-1 Clinical Differences Between Delirium and Dementia
| Delirium | Dementia | |
|---|---|---|
| Onset | Acute to subacute | Subacute to chronic |
| Level of consciousness | Impaired, fluctuates | Unaffected until late stages |
| Cognition | Poor attention, disorientation | Poor memory; attention and orientation affected later |
| Motor behavior | Variably increased or reduced | Usually normal |
| Psychotic features | Common and prominent | Less common and usually less prominent |
Treatment
Benzodiazepines may be used for their sedating and anxiolytic effects.
Andrew MK, Freter SH, Rockwood K. Prevalence and outcomes of delirium in community and non-acute care settings in people without dementia: a report from the Canadian Study of Health and Aging. BMC Medicine. 2006;4:15.
Brown TM, Boyle MF. ABC of psychological medicine: delirium. BMJ. 21 Sept 2002;325:644-647.
Francis J, Young GB. Diagnosis of delirium and confusional states. www.uptodate.com, 2009.
Johnson MH. Assessing confused patients. J Neurol Neurosurg Psychiatry. 2001;71(Suppl. 1):i7-i12.
Meagher DJ. Delirium: optimising management. BMJ. 20 January 2001;322:144-149.