Chapter 8 Definition and Incidence of the Difficult Airway
I Introduction
The fundamental responsibility of an anesthesiologist is to ensure adequate gas exchange for the patient. Failure to maintain oxygenation for more than a few minutes can result in catastrophic anoxic injury. Data from closed claims of respiratory-related malpractice in 1990 reported brain damage or death in more than 85% of patients.1 In the closed claims data from 2006, improvements in airway management techniques and monitoring standards had reduced the number of intubation-related claims,2 but difficulties with airway management during emergence remained among the leading causes of serious perioperative problems. It has been estimated that the inability to successfully manage a difficult airway (DA) is responsible for as many as 30% of deaths directly attributable to anesthesia.2
II Definition and Classification of the Difficult Airway
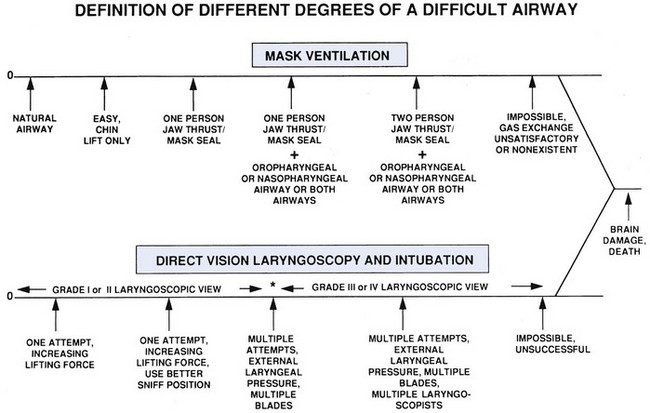
The term difficult airway spans a spectrum of clinical situations (Fig. 8-1), from difficulty or inability to provide mask ventilation to difficulty or inability to intubate the trachea. The combined “cannot intubate, cannot ventilate” (CICV) scenario carries the highest risk of brain damage or death. To better describe the layers of difficulty, we have chosen several categories of difficult or impossible mask ventilation; difficult placement of, or ventilation via an SGA; difficult laryngoscopy; and difficult intubation using direct laryngoscopy, video laryngoscopy, or flexible bronchoscopy.
A Difficult or Impossible Face Mask Ventilation
2 Definition of Difficult Mask Ventilation
The simplest mask ventilation scale in contemporary literature was described by Han and colleagues in 2004 (Table 8-1).3 In that scale, the progressive grades of difficulty are (1) ventilation by mask; (2) ventilation by mask with oral airway or other adjuvant with or without muscle relaxant; (3) difficult mask ventilation, defined as “inadequate, unstable, or requires two providers” with or without muscle relaxant; and (4) impossible mask ventilation with an inability to mask ventilate with or without muscle relaxant.
TABLE 8-1 Han Mask Ventilation Scale and Incidence of Difficult Mask Ventilation
| Grade | Description | Incidence (n, [%]) |
|---|---|---|
| 1 | Ventilated by mask | 37,857 (71.3%) |
| 2 | Ventilated by mask with oral airway or other adjuvant with or without muscle relaxant | 13,966 (26.3%) |
| 3 | Difficult ventilation (inadequate, unstable, or requiring two providers) with or without muscle relaxant | 1,141 (2.2%) |
| 4 | Unable to mask ventilate with or without muscle relaxant | 77 (0.15%) |
From Han R, Tremper KK, Kheterpal S, O’Reilly M: Grading scale for mask ventilation. Anesthesiology 101:267, 2004.
Langeron and colleagues defined difficult face mask ventilation as “the inability of an unassisted anesthesiologist to maintain oxygen saturation >92%, as measured by pulse oximetry, or to prevent or reverse signs of inadequate ventilation during positive-pressure mask ventilation under general anesthesia.”4 In their study, mask ventilation was considered difficult if one or more of six criteria were present:
1. Inability for the unassisted anesthesiologist to maintain oxygen saturation >92% using 100% oxygen and positive-pressure mask ventilation
2. Important gas flow leak by the face mask
3. Need to increase gas flow to >15 L/min and to use the oxygen flush valve more than twice
4. No perceptible chest movement
El-Ganzouri and coworkers defined difficult mask ventilation as the “inability to obtain chest excursion sufficient to maintain a clinically acceptable capnogram waveform despite optimal head and neck positioning and use of muscle paralysis, use of an oral airway, and optimal application of a face mask by anesthesia personnel.”5
3 Incidence of Difficult Mask Ventilation
Two studies by Kheterpal and associates on difficult and impossible mask ventilation represent the largest investigations to date on the topic. The incidence of difficult mask ventilation was 1.4% in 22,660 patients and 2.2% in a subsequent study of 50,000 patients.6,7 The incidence of impossible ventilation ranged from 0.15% to 0.16% in these two large studies. Langeron and colleagues reported a 5% incidence of difficult mask ventilation, with 1 of every 1502 patients impossible to ventilate with a face mask (0.07%).4 In other large, prospective studies the incidence has ranged from 0.07% to 1.4%,5,8,9 although this was not the primary outcome being assessed. In summary, difficult mask ventilation can be expected 1 or 2 times in every 100 anesthesias, and impossible mask ventilation 1 or 2 times in 1000 anesthesias.
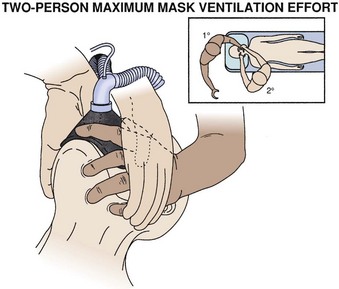
Methods used to improve airway patency include the head-tilt, jaw-thrust, and chin-lift maneuvers as well as insertion of oral or nasal airways. If mask seal is poor, the practitioner may choose a different face mask, use a two-hand or two-person technique, insert bolsters between the alveolar ridge and the cheeks, or employ other methods to improve the interface between the face and the mask. When two persons are needed, ideally the primary anesthesiologist stands at the patient’s head and initiates jaw thrust with the left hand at the angle of the left mandible and left-sided mask seal while the right hand compresses the reservoir bag. The standard position for the primary anesthesiologist appears in Figure 8-2. The secondary (helping) person stands at the patient’s side, at the level of the patient’s shoulder, facing the primary anesthesiologist. The right hand of the secondary anesthesiologist should cover the left hand of the primary anesthesiologist and contribute to left-sided jaw thrust and mask seal, and the left hand of the secondary person initiates right-sided jaw thrust and mask seal. In this way, all four hands are doing something important without interfering with one another, and there is almost no redundant effort. With this positioning, the secondary person can watch the monitors continuously, manipulate the larynx externally, and hand equipment to the primary anesthesiologist.
B Difficulties with Supraglottic Airway Devices
The last two decades have seen a phenomenal increase in the use of SGAs for elective and rescue purposes. Most studies of SGA devices describe first-attempt and overall success rates. Difficulties with the devices include failure of insertion, failure to form a clear passage to the trachea, and failure to form an effective seal in the airway.10
Most of the studies reporting difficulties with SGAs have focused on LMAs. Among these, the failure rate is 1% for the intubating and ProSeal models and 2% for the LMA classic and flexible models.10
2 Incidence of Success
For the ProSeal laryngeal mask airway (PLMA), first-attempt success rates range from 76% to 100% (mean, 87.3%), and overall insertion success rates range from 90% to 100% (mean, 98.4%).11 One of the important rescue functions of the LMA is as a conduit for flexible bronchoscopic intubation. The inability to visualize vocal cords using a trans-LMA flexible bronchoscopic technique is a significant impediment to successful tracheal intubation. The incidence of difficult laryngeal visualization ranges from 0% to 26% with the PLMA.11 Although it is possible that success rates with other SGA devices may differ, the inherent variability in success is an important learning point. Early recognition of unsuccessful placement and institution of alternative airway plans are essential to prevent morbidity from failure of an SGA device.
C Difficult Direct Laryngoscopy
1 Laryngeal Visualization
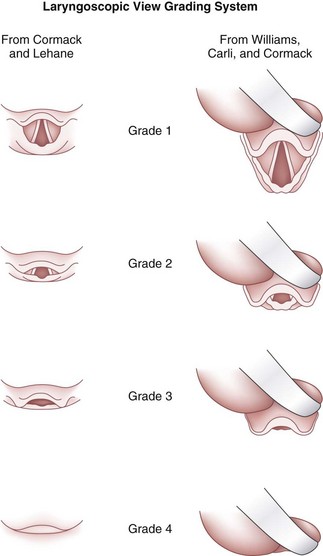
The appearance of the laryngeal inlet on direct laryngoscopy is best described by the Cormack and Lehane grade of laryngeal view.12 Difficult laryngoscopy is most commonly defined as presence of a grade 3 or 4 view on laryngoscopy.6,7 Several maneuvers have been shown to improve the laryngeal view on laryngoscopy, but in general, poorer laryngeal views contribute progressively to greater difficulty in achieving successful tracheal intubation (Fig. 8- 3).12–14 As the view worsens, increasing the anterior lifting force with the laryngoscope blade, reinstituting the optimal sniff position, making multiple attempts, manipulating the larynx externally (see Chapter 17 and Fig. 17-10), or opting for alternative devices or laryngoscopists may be required to achieve intubation.
There is a learning curve for management of a DA, and a poor laryngeal view observed by an inexperienced laryngoscopist may easily be improved by a more experienced or skillful individual with perhaps a different blade. Although a severe grade 3 (epiglottis tip) or grade 4 (just soft palate) laryngoscopic view (see Fig. 8-3) may be overcome by the occasional successful “blind” intubation, these views more often render intubation impossible. Therefore, early recognition of a DA and immediate availability of skilled help and advanced equipment for airway management are essential components of DA management.
2 Incidence of Difficult Laryngeal Visualization
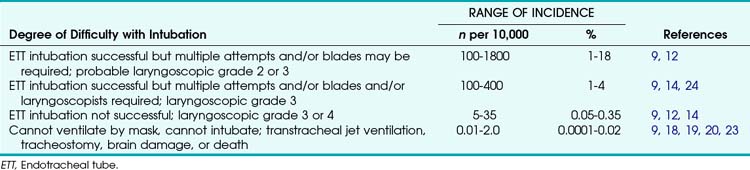
The incidence of difficult laryngoscopy or intubation in the general surgical population varies greatly depending on the laryngeal view, the individual study population, and the definition of a DA. A grade 2 or 3 laryngoscopic view requiring multiple attempts or blades (and presumably external laryngeal pressure) is relatively common and is found in 1% to 18% of cases (Table 8-2). Grade 3 laryngeal views result in a successful intubation at a rate of 1% to 4%. Intubation is unsuccessful in between 5 and 35 of every 10,000 patients, and the CICV scenario occurs in 0.01 to 2 patients per 10,000.
For studies of difficult laryngoscopy to be reliable and for the laryngoscopic grading system to be helpful, the reported grades must describe the best view that was obtained, which, in turn, depends on the best possible performance of laryngoscopy. The components of best performance of laryngoscopy consist of the optimal sniff position, good complete muscle relaxation, firm forward traction on the laryngoscope, and, if necessary, firm external laryngeal manipulation. For example, the application of external laryngeal pressure may reduce the incidence of a grade 3 view from 9% to between 5.4% and 1.3%.9 In doubtful cases, the anesthesiologist, while performing laryngoscopy with the left hand, should quickly apply external pressure over the hyoid, thyroid, and cricoid cartilages with the right hand. The pressure point that affords the best laryngeal view can be determined in a matter of seconds.
D Difficult Intubation During Direct Laryngoscopy
Unlike difficult mask ventilation and difficult laryngoscopy, there is no uniformly accepted method of classifying difficult intubation. The Intubation Difficulty Score (IDS) validated by Adnet and colleagues15 describes a spectrum of intubation difficulty. The assessment variables for the IDS are number of additional attempts, number of additional operators, number of alternative intubation techniques used, Cormack-Lehane laryngeal view minus 1, need for excessive lifting force, need for laryngeal pressure, and vocal cord adduction. Each variable carries one point, and difficult intubation is defined as an IDS score greater than 5, indicating moderate to major difficulty, with infinity (∞) being assigned to an impossible intubation. Kheterpal and associates defined difficult intubation as intubation requiring more than three attempts by anesthesia attending staff to secure the airway with an endotracheal tube.6,7
1 Incidence of Difficult Intubation
The incidence of difficult intubation was 10.3% in a recent study of emergent tracheal intubations in a university hospital.16 The incidence of failed tracheal intubation ranges from 0.05% to 0.35%; the low and high ends of this range are associated with elective surgical and obstetric patients, respectively. The incidence of failed intubation is approximately 8 times higher in the obstetric population than in others, with a 13-fold increase in the risk of death.17
2 Combined Difficult Mask Ventilation and Difficult Intubation
In one study, the incidence of combined difficult mask ventilation and difficult intubation was 0.37%.6 Patients whose lungs were impossible to ventilate via mask had a risk for difficult intubation of 25%, significantly higher than that for the overall population. One in three patients with combined impossible mask ventilation and difficult intubation required an alternative intubation technique to secure the airway, with 10% of such patients requiring a surgical airway. Similarly, one of the significant findings in another study was that difficult mask ventilation conferred a fourfold greater risk for difficult intubation and a 12-fold greater risk of an impossible intubation.5
3 Impossible Mask Ventilation and Intubation
The incidence of CICV has been estimated to range from 0.01 to 2.0 cases per 10,000 patients.17–20 In a recent study of 50,000 patients, Kheterpal and colleagues described the incidence as 3.75 per 10,000 patients.7 Despite recent advances in airway devices and techniques, most busy hospitals encounter several such events every year, making it imperative to ensure that DA recognition and management remains a central tenet of anesthesiology education and training.
4 Variability in Incidence of Difficult Laryngoscopy and Difficult Intubation
Difficult direct laryngoscopy (a grade 3 or 4 laryngeal view) is synonymous with difficult intubation in most patients.12 However, tracheal intubation and laryngoscopy have slightly differing skill requirements, which may contribute to variability in the occurrence of difficult laryngoscopy and difficult intubation. In one prospective study examining respiratory complications in 1005 patients whose tracheas were intubated, 3 patients had grade 4 laryngeal views. One of these patients was easy to intubate, one was “moderately difficult” to intubate, and one was “difficult” to intubate.8 In the same study, among 68 patients with a grade 3 laryngoscopic view, 5 (7%) were difficult to intubate, 50 (74%) were moderately difficult, and 13 (19%) were easy to intubate.
Four relatively uncommon scenarios explain some of the discordance between difficult laryngoscopy and difficult intubation. First, some patients with a grade 3 view have a trachea that can be intubated on the first or second attempt if the distal end of the endotracheal tube is appropriately curved by a malleable stylet (hockey-stick shape) or if a small curved introducer is used (e.g., a gum elastic bougie). Second, grade 3 laryngoscopic views have been variously described as seeing only the palate and all of the epiglottis or as seeing only the palate and just the tip of the epiglottis.21 The different attributes of grade 3 may respond differently to adjustments such as optimal external laryngeal pressure, and therefore they may differ initially and subsequently with respect to difficulty of tracheal intubation. Third, a grade 3 view with a curved blade placed in the vallecula (because of a long, floppy epiglottis) may become a grade 1 or 2 view if either a curved or straight blade is placed posterior to the epiglottis and lifted anteriorly.22 Fourth, pathologic conditions such as laryngeal web, laryngeal tumors, or tracheal stenosis may disassociate ease of laryngoscopy from difficulty of tracheal intubation.
5 Complications of Difficult Laryngoscopy and Difficult Intubation
Anesthesia in a patient with a DA can lead to direct airway trauma and morbidity from hypoxia and hypercarbia. Incidence of brain damage, cardiac arrest, and death related to airway disasters appears to be decreasing.2,19,23 Directly mediated laryngovagal reflexes (airway spasm, apnea, bradycardia, arrhythmia, or hypotension) and laryngospinal reflexes (coughing, vomiting, or bucking) are the source of some morbidity. In general, DA management is more likely to be associated with use of physical force during laryngoscopy and more attempts to secure the airway; together, these increase the incidence of complications. Airway complications can range from minor (trivial or nuisance value) to major (life-threatening or fatal).
In a recent study on emergent tracheal intubations with a 10.8% incidence of difficult intubation, the complications seen in 4.2% of cases were aspiration, esophageal intubation, dental injury, and pneumothorax.16 The independent predictors of complications in this study were multiple intubation attempts (odds ratio [OR], 6.7; 95% confidence interval [CI], 3.2 to 14.2), grade 3 or 4 laryngeal view (OR, 1.9; 95% CI, 1.1 to 3.5), general care floor location (OR, 1.9; 95% CI, 1.2 to 3.0), and emergency department location (OR, 4.7; 95% CI, 1.1 to 20.4).
In an earlier study, a 5% incidence of relatively minor upper airway complications (posterior pharyngeal and lip lacerations and bruises) was demonstrated with laryngoscopy and intubation in patients with normal airways. In patients with anticipated difficult intubation, the incidence of minor trauma increased to 17%.24 In patients in whom tracheal intubation was actually found to be difficult (i.e., multiple attempts at laryngoscopy but ultimately successful), the incidence of upper airway complications was 63%.24
In previous studies of anesthetic cardiac arrests, the incidence of inability to ventilate after induction was 0.12 per 10,000 anesthesias, accounting for 12% of the preventable causes. However, in a large contemporary study of 50,000 patients undergoing anesthesia for surgery, no incidence of brain damage or death was noted.7 This result validates the view that modern advances in preoperative airway assessment, patient monitoring, airway equipment, and techniques have significantly reduced severe morbidity due to a DA.
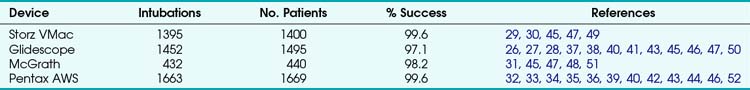
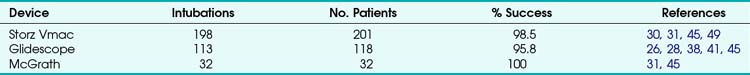
E Difficult Video Laryngoscopy
Video laryngoscopes and optical laryngoscopes have been increasingly used in routine and DA management. In general, these devices provide a better laryngoscopic view than does direct laryngoscopy. It is important to note that an improved Cormack-Lehane laryngoscopic grade does not always guarantee successful intubation of the trachea.25 Many of these devices use a highly angulated blade with a camera positioned to allow the user to “see around the corner” of the tongue. Whereas direct laryngoscopy creates a straight line between the operator’s eye and the vocal cords, allowing straightforward intubation, highly curved video laryngoscopes maintain the natural curvature of the airway and require special techniques to pass a tube into the trachea.
An excellent review of video laryngoscope use in adult airway management has been published.25 It pooled data from 27 studies in adult patients (Tables 8-3 and 8-4). The operators using the devices were different, and the criteria for successful intubation as well as the definition of a DA were inconsistently applied from study to study, so the reader should not make direct comparisons between the devices listed in these two tables. The tracheas of patients with normal airways were intubated between 97.1% and 99.6% of the time with these devices. There are fewer data for patients with DAs, but the rate of successful intubation varied from 95.8% to 100% with video-enabled devices.
F Difficult Flexible Bronchoscopic Intubation
1 Definition of Difficult Flexible Bronchoscopic Intubation
Flexible bronchoscopic intubation skills are now considered essential for all practicing anesthesia providers. Although flexible bronchoscopic devices have enhanced patient safety, especially when DA management is anticipated, they are by no means fail-safe. A difficult or impossible flexible bronchoscopic intubation can broadly be described as inadequate laryngeal visualization with or without difficulty in advancing an endotracheal tube. The ease of laryngeal exposure was defined by Ovassapian as not difficult, moderately difficult (needing some manipulation of the fiberscope in all directions), or difficult (needing extensive manipulation of the bronchoscope in all directions with or without change in position).53
2 Incidence of Difficult or Failed Flexible Bronchoscopic Intubation
Inadequate laryngeal visualization is a result of several factors acting individually or in tandem: inexperienced operators, presence of blood or secretions, inadequate topical anesthesia, distorted airway anatomy, and equipment failure. Factors typically unaffected by direct laryngoscopy, such as the presence of a large, floppy epiglottis or small amounts of pharyngeal blood, could pose significant hurdles to successful flexible bronchoscopic intubation. The incidence of difficult laryngeal visualization has been reported to be 6.7% with orotracheal and 4.4% with nasotracheal awake flexible bronchoscopic intubation.53 The incidence of difficult laryngeal visualization using orotracheal approach under general anesthesia was only 4.4%, reflecting differences in patient types, with distorted upper airway anatomy or a severely compromised airway typically being managed in an awake patient. The incidence of difficult flexible bronchoscopic intubation using an orotracheal approach was 29.1% in awake and 24.1% in anesthetized patients. In contrast, the incidence during nasotracheal intubation was markedly lower, at 6.0% in awake and 11.0% in anesthetized patients, reflecting important technical differences between the two approaches. Flexible bronchoscopic intubation failed in 1.4% of awake and 2.1% of anesthetized patients, with equal distribution of difficult visualization and inability to advance the endotracheal tube.53
IV Clinical Pearls
• The inability to manage a difficult airway (DA) is responsible for a large proportion of deaths and morbidity directly attributable to anesthesia.
• Although it is important to have common definitions for common problems, the literature continues to report variable nomenclature related to DA management. It is important to have an understanding of the incidence of significant airway problems for the specialty to make advances in this area.
• Difficult mask ventilation has been reported at a rate of 1 to 2 per 100 anesthesias, and impossible mask ventilation can be expected at a rate of 1 to 2 per 1000 anesthesias.
• The failure rate for supraglottic airway (SGA) devices is approximately 2% for the classic and flexible laryngeal mask airways (LMAs) and 1% for the intubating and ProSeal LMAs.
• Fewer data exist regarding failure of video and optical laryngoscopes than for direct laryngoscopy, but the incidence of failed intubation with these devices ranges from 0.4% to 2.9% in patients with a normal airway and from 0% to 4.2% for patients with a DA.
• When difficult laryngoscopy is defined as a Cormack-Lehane grade 2 or 3 view requiring multiple attempts or blades, the reported incidence varies from 1% to 18% of surgical cases; however, most of these patients are successfully intubated.
• Unsuccessful intubation with direct laryngoscopy occurs at a rate of 5 to 35 per 10,000 anesthesias, and the “cannot intubate, cannot ventilate” (CICV) scenario occurs at a rate of 0.01 to 2 per 10,000 anesthesias.
• Large multicenter studies will be required to refine understanding of the incidence of serious airway problems.
All references can be found online at expertconsult.com.
1 Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–833.
2 Cheney FW, Posner KL, Lee LA, et al. Trends in anesthesia-related death and brain damage: A closed claims analysis. Anesthesiology. 2006;105:1081–1086.
3 Han R, Tremper KK, Kheterpal S, O’Reilly M. Grading scale for mask ventilation. Anesthesiology. 2004;101:267.
4 Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
5 el-Ganzouri AR, McCarthy RJ, Tuman KJ, et al. Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–1204.
7 Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: A review of 50,000 anesthetics. Anesthesiology. 2009;110:891–897.
12 Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111.
25 Niforopoulou P, Pantazopoulos I, Demestiha T, et al. Video-laryngoscopes in the adult airway management: A topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–1061.
1 Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–833.
2 Cheney FW, Posner KL, Lee LA, et al. Trends in anesthesia-related death and brain damage: A closed claims analysis. Anesthesiology. 2006;105:1081–1086.
3 Han R, Tremper KK, Kheterpal S, O’Reilly M. Grading scale for mask ventilation. Anesthesiology. 2004;101:267.
4 Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
5 el-Ganzouri AR, McCarthy RJ, Tuman KJ, et al. Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–1204.
6 Kheterpal S, Han R, Tremper KK, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885–891.
7 Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: A review of 50,000 anesthetics. Anesthesiology. 2009;110:891–897.
8 Asai T, Koga K, Vaughan RS. Respiratory complications associated with tracheal intubation and extubation. Br J Anaesth. 1998;80:767–775.
9 Rose DK, Cohen MM. The airway: Problems and predictions in 18,500 patients. Can J Anaesth. 1994;41:372–383.
10 Brimacombe JR. Laryngeal mask anesthesia: Principle and practice, ed 2. Philadelphia: Saunders; 2005.
11 Cook TM, Lee G, Nolan JP. The ProSeal laryngeal mask airway: A review of the literature. Can J Anaesth. 2005;52:739–760.
12 Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111.
13 Williams KN, Carli F, Cormack RS. Unexpected difficult laryngoscopy: A prospective survey in routine general surgery. Br J Anaesth. 1991;66:38–44.
14 Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987;42:487–490.
15 Adnet F, Borron SW, Racine SX, et al. The intubation difficulty scale (IDS): Proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87:1290–1297.
16 Martin LD, Mhyre JM, Shanks AM, et al. 3,423 Emergency tracheal intubations at a university hospital: Airway outcomes and complications. Anesthesiology. 2011;114:42–48.
17 Munnur U, de Boisblanc B, Suresh MS. Airway problems in pregnancy. Crit Care Med. 2005;33:S259–S268.
18 Bellhouse CP, Dore C. Criteria for estimating likelihood of difficulty of endotracheal intubation with the Macintosh laryngoscope. Anaesth Intensive Care. 1988;16:329–337.
19 Keenan RL, Boyan CP. Decreasing frequency of anesthetic cardiac arrests. J Clin Anesth. 1991;3:354–357.
20 Tunstall ME. Failed intubation in the parturient. Can J Anaesth. 1989;36:611–613.
21 Williamson R. Grade III laryngoscopy: Which is it? Anaesthesia. 1988;43:424.
22 Arino JJ, Velasco JM, Gasco C, Lopez-Timoneda F. Straight blades improve visualization of the larynx while curved blades increase ease of intubation: A comparison of the Macintosh, Miller, McCoy, Belscope and Lee-Fiberview blades. Can J Anaesth. 2003;50:501–506.
23 Eichhorn JH. Documenting improved anesthesia outcome. J Clin Anesth. 1991;3:351–353.
24 Hirsch IA, Reagan JO, Sullivan N. Complications of direct laryngoscopy: A prospective analysis. Anesthesiol Rev. 1990;17:34.
25 Niforopoulou P, Pantazopoulos I, Demestiha T, et al. Video-laryngoscopes in the adult airway management: A topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–1061.
26 Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (Glidescope) in 728 patients. Can J Anaesth. 2005;52:191–198.
27 Rai MR, Dering A, Verghese C. The Glidescope system: A clinical assessment of performance. Anaesthesia. 2005;60:60–64.
28 Stroumpoulis K, Pagoulatou A, Violari M, et al. Videolaryngoscopy in the management of the difficult airway: A comparison with the Macintosh blade. Eur J Anaesthesiol. 2009;26:218–222.
29 Kaplan MB, Hagberg CA, Ward DS, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357–362.
30 Kaplan MB, Ward DS, Berci G. A new video laryngoscope: An aid to intubation and teaching. J Clin Anesth. 2002;14:620–626.
31 Shippey B, Ray D, McKeown D. Case series: The McGrath videolaryngoscope—An initial clinical evaluation. Can J Anaesth. 2007;54:307–313.
32 Suzuki A, Toyama Y, Katsumi N, et al. The Pentax-AWS rigid indirect video laryngoscope: Clinical assessment of performance in 320 cases. Anaesthesia. 2008;63:641–647.
33 Hirabayashi Y, Seo N. Airway scope: Early clinical experience in 405 patients. J Anesth. 2008;22:81–85.
34 Hirabayashi Y. Airway scope: Initial clinical experience with novice personnel. Can J Anaesth. 2007;54:160–161.
35 Asai T, Enomoto Y, Shimizu K, et al. The Pentax-AWS video-laryngoscope: The first experience in one hundred patients. Anesth Analg. 2008;106:257–259.
36 Asai T, Liu EH, Matsumoto S, et al. Use of the Pentax-AWS in 293 patients with difficult airways. Anesthesiology. 2009;110:898–904.
37 Nouruzi-Sedeh P, Schumann M, Groeben H. Laryngoscopy via Macintosh blade versus Glidescope: Success rate and time for endotracheal intubation in untrained medical personnel. Anesthesiology. 2009;110:32–37.
38 Xue FS, Zhang GH, Liu J, et al. The clinical assessment of Glidescope in orotracheal intubation under general anesthesia. Minerva Anestesiol. 2007;73:451–457.
39 Hirabayashi Y, Seo N. Tracheal intubation by non-anesthesia residents using the Pentax-AWS airway scope and Macintosh laryngoscope. J Clin Anesth. 2009;21:268–271.
40 Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–730.
41 Sun DA, Warriner CB, Parsons DG, et al. The Glidescope video laryngoscope: Randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–384.
42 Enomoto Y, Asai T, Arai T, et al. Pentax-AWS, a new videolaryngoscope, is more effective than the Macintosh laryngoscope for tracheal intubation in patients with restricted neck movements: A randomized comparative study. Br J Anaesth. 2008;100:544–548.
43 Malik MA, Subramaniam R, Maharaj CH, et al. Randomized controlled trial of the Pentax AWS, Glide-scope, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth. 2009;103:761–768.
44 Komatsu R, Kamata K, Hoshi I, et al. Airway Scope and gum elastic bougie with Macintosh laryngoscope for tracheal intubation in patients with simulated restricted neck mobility. Br J Anaesth. 2008;101:863–869.
45 Maassen R, Lee R, Hermans B, et al. A comparison of three videolaryngoscopes: The Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth Analg. 2009;109:1560–1565.
46 Liu EH, Goy RW, Tan BH, Asai T. Tracheal intubation with videolaryngoscopes in patients with cervical spine immobilization: A randomized trial of the Airway Scope and the Glidescope. Br J Anaesth. 2009;103:446–451.
47 van Zundert A, Maassen R, Lee R, et al. A Macintosh laryngoscope blade for videolaryngoscopy reduces stylet use in patients with normal airways. Anesth Analg. 2009;109:825–831.
48 O’Leary AM, Sandison MR, Myneni N, et al. Preliminary evaluation of a novel videolaryngoscope, the McGrath series 5, in the management of difficult and challenging endotracheal intubation. J Clin Anesth. 2008;20:320–321.
49 Jungbauer A, Schumann M, Brunkhorst V, et al. Expected difficult tracheal intubation: A prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br J Anaesth. 2009;102:546–550.
50 Xue FS, Zhang GH, Li XY, et al. Comparison of hemodynamic responses to orotracheal intubation with the Glidescope videolaryngoscope and the Macintosh direct laryngoscope. J Clin Anesth. 2007;19:245–250.
51 Walker L, Brampton W, Halai M, et al. Randomized controlled trial of intubation with the McGrath Series 5 videolaryngoscope by inexperienced anaesthetists. Br J Anaesth. 2009;103:440–445.
52 Malik MA, Subramaniam R, Churasia S, et al. Tracheal intubation in patients with cervical spine immobilization: A comparison of the Airwayscope, LMA CTrach, and the Macintosh laryngoscopes. Br J Anaesth. 2009;102:654–661.
53 Ovassapian A. Flexible bronchoscopic endoscopy and the difficult airway. Philadelphia: Lippincott-Raven; 1996.