48
Darier Disease and Hailey–Hailey Disease
Darier Disease (Keratosis Follicularis)
– Onset usually between ages 6 and 20 years, with peak during adolescence.
– Chronic course, often worse in summer.
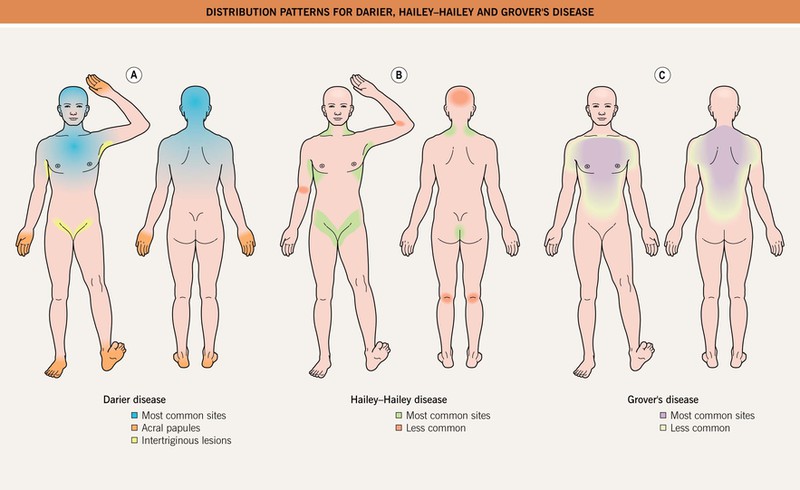
– Crusted, pink-red to brown papules that may coalesce into plaques (Fig. 48.1) in a ‘seborrheic’ and sometimes intertriginous distribution (Fig. 48.2).





Fig. 48.1 Darier disease. Truncal involvement with a predilection for seborrheic areas (A–D). Keratotic papules can vary from red (A, B) to brown (C, D) in color and may become confluent. E Severe intertriginous involvement. A, C, Courtesy, Julie V. Schaffer, MD; E, Courtesy, Daniel Hohl, MD.
– Hypopigmented macules may be the predominant feature, especially in darker skin types (Fig. 48.3).

Fig. 48.3 Darier disease. Observed most commonly in individuals with darkly pigmented skin, a guttate leukoderma may be seen in patients with Darier disease, including the segmental form. Courtesy, Julie V. Schaffer, MD.
– Itching and malodor can be prominent.
– Flat-topped skin-colored to brown papules (resemble flat warts) on the dorsal hands and feet (Fig. 48.4).

Fig. 48.4 Darier disease. Multiple flat-topped papules on the dorsal aspect of the hand. Courtesy, Daniel Hohl, MD.
– Palmoplantar keratotic papules (Fig. 48.5).


Fig. 48.5 Palmar involvement in Darier disease. A Both keratotic papules and keratin-filled depressions are seen. B Less commonly, a thick, spiked focal keratoderma is observed. A, Courtesy, Kalman Watsky, MD; B, Courtesy, Julie V. Schaffer, MD.
– Nail changes, e.g. distal notching with longitudinal erythronychia (see Chapter 58).
– Whitish papules of the oral mucosa (Fig. 48.6).
• Rare subtypes – acral hemorrhagic, segmental (see Chapter 51).
• Exacerbating factors include sunlight, heat, occlusion, sweat, bacterial colonization.
• There may be an association with neuropsychiatric disease (e.g. major depression).
• Complications include bacterial (e.g. Staphylococcus aureus), fungal (e.g. tinea corporis), viral (e.g. herpes simplex virus [HSV]) infections; consider Kaposi’s varicelliform eruption due to HSV in a patient with sudden onset of uniform hemorrhagic crusts, fever, and malaise (Fig. 48.7).

Fig. 48.7 Darier disease with superimposed HSV infection (Kaposi’s varicelliform eruption). Multiple hemorrhagic crusts of a similar size are seen.
• Histologic features – acantholytic dyskeratosis above suprabasilar clefting.
• DDx: mild forms – severe seborrheic dermatitis, Grover’s disease; predominantly intertriginous – Hailey–Hailey disease, pemphigus vegetans, blastomycosis-like pyoderma, papular acantholytic dyskeratosis (vulvar); acral lesions – acrokeratosis verruciformis of Hopf (may be an allelic disorder or forme fruste; Fig. 48.8), flat warts, stucco keratosis, Flegel’s disease.

Fig. 48.8 Acrokeratosis verruciformis of Hopf. Involvement of the dorsal aspect of the foot with flat-topped papules.
• Rx:
– General measures: lightweight clothing, sunscreen, antimicrobial cleansers, keratolytic emollients.
Hailey–Hailey Disease (Familial Benign Chronic Pemphigus)
– Onset in the second or third decade but sometimes delayed into the fourth or fifth decade.
– Variable course with remissions and flares.
– Mainly affects the major body folds (Fig. 48.2), including inframammary in women (Fig. 48.9); sometimes other sites affected (Fig. 48.10).


Fig. 48.9 Hailey–Hailey disease. A Erythematous, eroded plaque in the axilla. Note the intact flaccid vesicles at 2 and 7 o’clock. B Chronic submammary lesion with erosions in a worm-eaten pattern.

Fig. 48.10 Hailey–Hailey disease. Circinate plaques on the back with erosions and crusting in the active borders. Courtesy, Louis A. Fragola, Jr., MD.
– Moist, malodorous plaques, with erosions, fissures, and flaccid blisters (Fig. 48.9); circinate plaques with eroded/crusted borders (Fig. 48.10).
• Rare subtype – segmental (see Chapter 51).
• Exacerbating factors include friction, heat, sweat, bacterial colonization, application of adhesive tape; complications the same as for Darier disease (see above).
• Histologic features – acantholysis of the majority of the epidermis.
• Rx:
– General measures: lightweight clothing, antimicrobial cleansers.
– For symptomatic disease: intermittent topical/intralesional CS.
For further information see Ch. 59. From Dermatology, Third Edition.