Chapter 2 Cysts and Other Benign Lesions
LANGERHANS CELL HISTIOCYTOSIS
EPIDEMIOLOGY
• The umbrella phrase LCH is now used in lieu of the previous clinical diagnoses of eosinophilic granuloma (localized, unifocal, or multifocal bony involvement), Hand–Schüller–Christian disease (localized bone [usually skull] involvement, exophthalmos, and diabetes insipidus), and Letterer–Siwe disease (disseminated disease).
• There has been a long-standing debate whether LCH represents a true neoplasm or merely an inflammatory process.1
• LCH is often considered a disease of childhood, but in a larger series,2 approximately 40% of the study population was younger than 20 years old; overall, LCH lesions were marginally more common in females than in males.
DISTRIBUTION
HISTOLOGY/GRADING
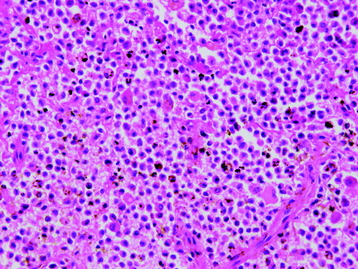
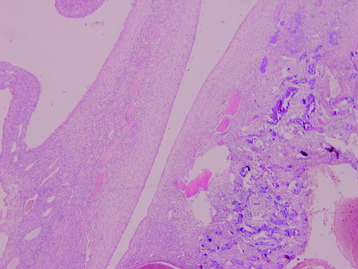
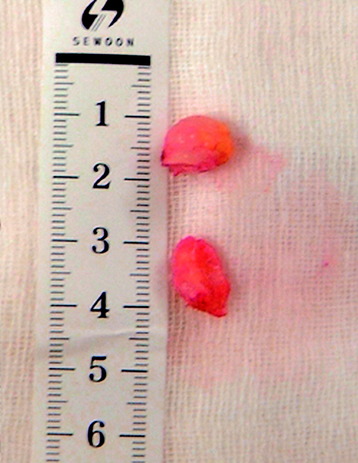
• The histologic feature of LCH consists of Langerhans cells, featured with grooved nuclei and faintly eosinophilic cytoplasm, and variable amounts of inflammatory cells including eosinophils, lymphocytes, plasma cells, and neutrophils (Fig. 2-1).
ANEURSYMAL BONE CYST
EPIDEMIOLOGY
• Aneurysmal bone cysts (ABCs) are characterized by small and large cavernous spaces filled with clotted-blood fluid.
DISTRIBUTION
• The cervical, thoracic, and lumbar spines are similarly affected and in most of the reported cases, the posterior elements of the vertebrae were the site of the lesion. Hay et al6 reported a series of 12 sacral lesions out of 92 cases of ABC in the spine.
• The etiology of ABCs is obscure, although the following theory is generally accepted. The aneurysmal bone cysts may be caused by development of a vicious hemodynamic cycle in a bone that is the site of a congenital vascular anomaly. This cycle is triggered by trauma or the development of other pathology, which interferes with venous drainage of the area. As a result, subsequent venous pressure increases, and a dilated and engorged vascular bed develops in the affected bone.4
HISTOLOGY
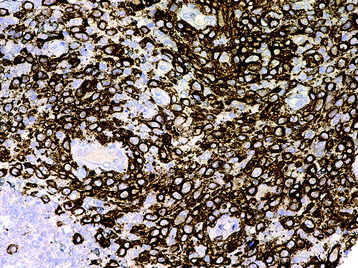
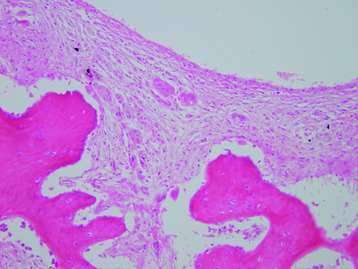
• Pathologically, ABCs contain multiple fluid-filled cavities separated by multiple fibrous septa. The new bone is commonly parallel to fibrous septa (Fig. 2-6). These large spaces filled with blood do not have an endothelial lining.7
• The fibrous septa are composed of a moderately dense cellular proliferation of bland fibroblasts, with scattered osteoclastic giant cells and reactive new bone (Fig. 2-7). In approximately one-third of cases, the bone is basophilic and has been termed “blue bone” (Fig. 2-8).
• The majority of secondary ABCs develop in association with benign neoplasms, most commonly giant cell tumor of bone, osteoblastoma, chondroblastoma, and fibrous dysplasia.
SYNOVIAL CYST
EPIDEMIOLOGY
• Synovial cysts are commonly reported in the spine, particularly within the lumbar spine. Spinal synovial cysts tend to be located principally in the spinal canal, adjacent to the facet joints of the lumbar spine.8
• The pathogenesis of synovial cysts remains unclear, but a lot of theories have been proposed to elucidate the causes of spinal synovial cysts, such as degenerative changes in the facet joints, trauma, metaplasia, the presence of developmental rests, excess stress inflicted at the facet joints coupled with the herniation of synovial tissue, and mucinous degeneration in the connective tissues.9
DISTRIBUTION
Synovial cysts occur in a juxta-articular, posterolateral, or epidural location within the lumbar spinal canal in 0.6–8% of MRI and CT examinations.9
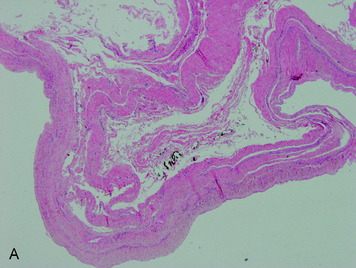
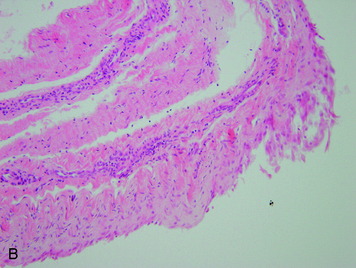
HISTOLOGY
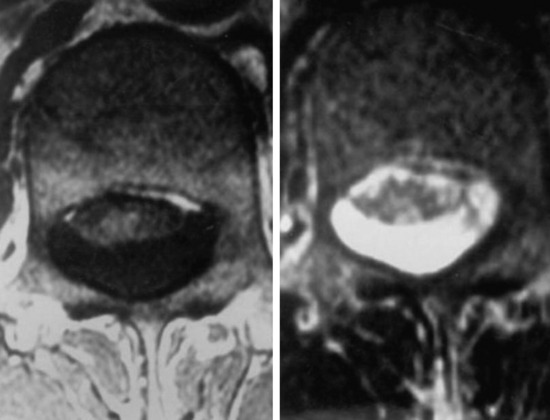
Pathologically, synovial cysts exhibit an epithelial-lining cystic lesion (Fig. 2-11, A and B), which can be differentiated from cystic degeneration of the yellow ligament. Facet degeneration accompanies 75% of the synovial cyst cases.
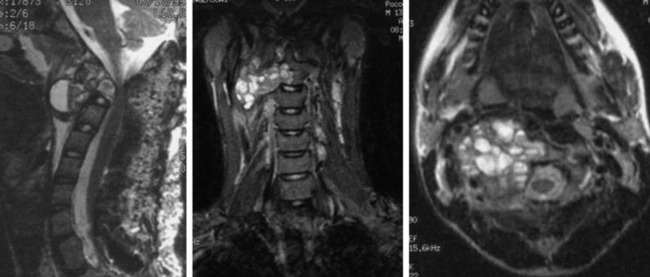
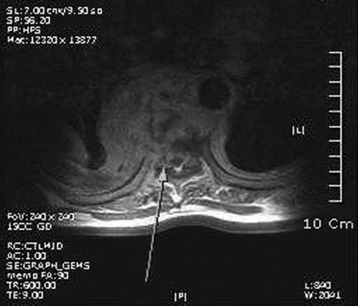
RADIOLOGY
• MRI is the examination of choice for synovial cysts. The typical finding of the synovial cyst is low to intermediate signal intensity on T1-weighted images, and high signal intensity on T2-weighted images (Fig. 2-12).
FIBROUS DYSPLASIA
EPIDEMIOLOGY
• Fibrous dysplasia is a multisystem disorder that may involve the central nervous system, endocrine organs, skin, and the skeletal system.
DISTRIBUTION
• In the monostotic form, the long tubular bones are often involved. On the other hand, the axial bone is more often involved in the polyostotic form.
• Although fibrous dysplasia accounts for approximately 7% of benign bone lesions, the prevalence of spinal involvement is thought to be very low, particularly in the monostotic form.14
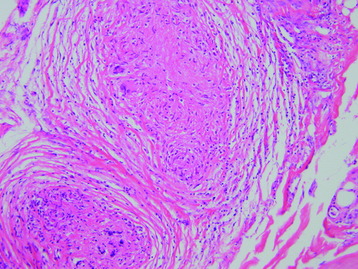
HISTOLOGY
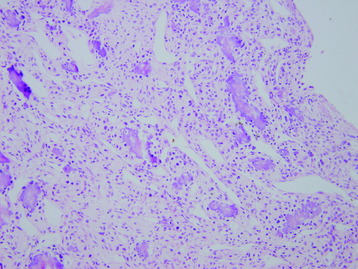
• The lesion is composed of fibrous and osseous components, which are present in varying proportions from lesion to lesion (Fig. 2-14).
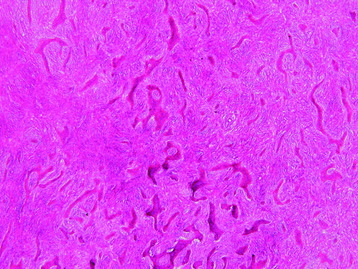
• The fibrous component is composed of cytologically bland spindle cells with a low mitotic rate, and the osseous component comprises irregular curvilinear trabeculae of woven bone, described as Chinese character–like (Fig. 2-15).
• Secondary changes, such as foam cells, multinucleated giant cells, aneurysmal bone cyst, or myxoid change may occur.
PYOGENIC OSTEOMYELITIS
• Pyogenic osteomyelitis is a bacterial suppurative infection of vertebrae and the intervertebral disc. It involves thoracic and lumbar vertebrae in most cases.
• Most of these patients are more than 50 years of age and may have other painful back conditions. Erroneous initial diagnoses are commonly made, delaying diagnosis for several weeks or months.17 It often can be misdiagnosed as metastatic or primary spine tumors.
• The incidence of vertebral osteomyelitis and discitis in one study10 was 5.3 cases per 1 million (as compared with a 7.6% and 3.9% prevalence in the general adult population of acute and chronic low back pain, respectively).
• The most common route of infection is bacteremia from an extraspinal primary source. The sources can be lung, gastrointestinal tract, genitourinary tract, and mucous infection. Vascularized subchondral bone adjacent to an endplate is the entrance to the bone marrow. Staphylococcus aureus is the most common pathogen.
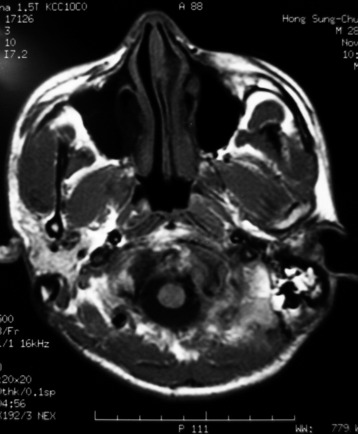
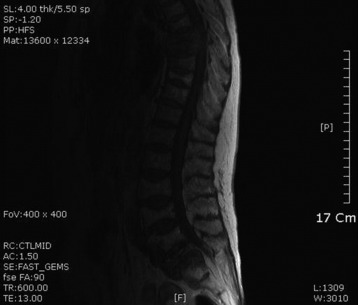
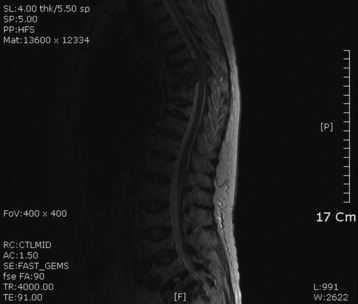
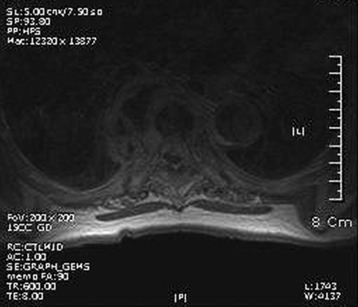
• On T1WI of MRI, low signal lesion is shown at the disc and adjacent vertebral bodies (Fig. 2-20). The disc space is seen to be narrow. On T2WI, the disc space is of high signal (Fig. 2-21).
• On enhancement with gadolinium, diffuse enhancement is achieved (Fig. 2-22). An epidural mass or paraspinal mass is commonly formed (Fig. 2-23).
TUBERCULOUS OSTEOMYELITIS
• Tuberculous spondylitis (TS) starts from the initial inoculum in the anterior vertebral body. The mode of transmission is hematogenous spread or through lymphatics from pulmonary origin.
• The spread to the adjacent vertebral body is made beneath the longitudinal ligament, with the intervertebral disc spared. Spondylitis develops in less than 1% of patients with tuberculosis.
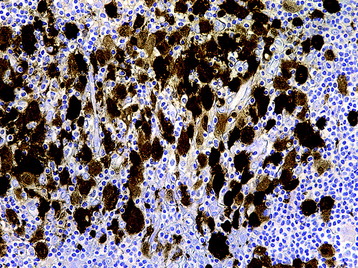
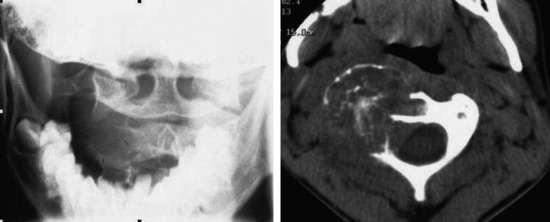
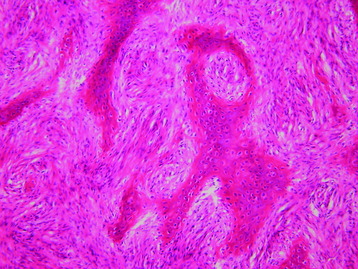
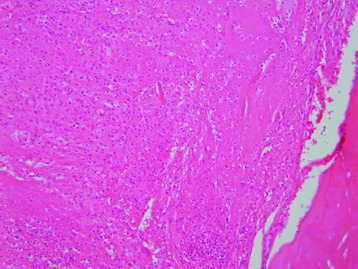
• The typical microscopic findings of tuberculosis are the formation of granuloma and caseation necrosis. The granuloma is composed of epithelioid histiocytes and one or two Langerhans giant cells. Lymphocyte infiltration is common (Fig. 2-24).
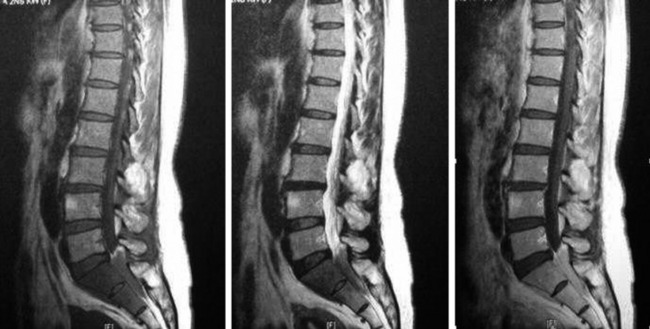
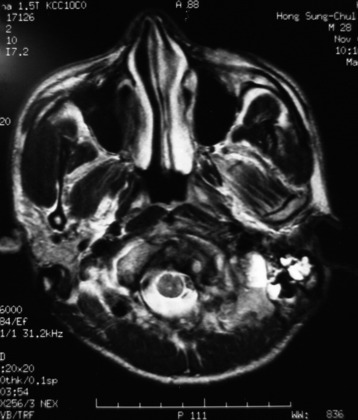
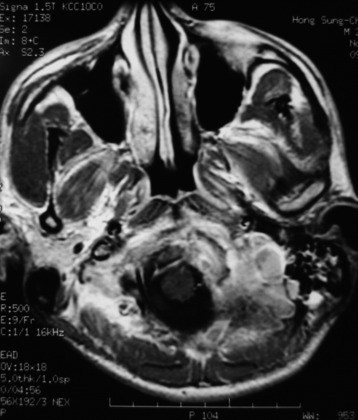
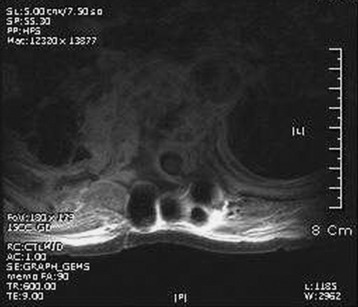
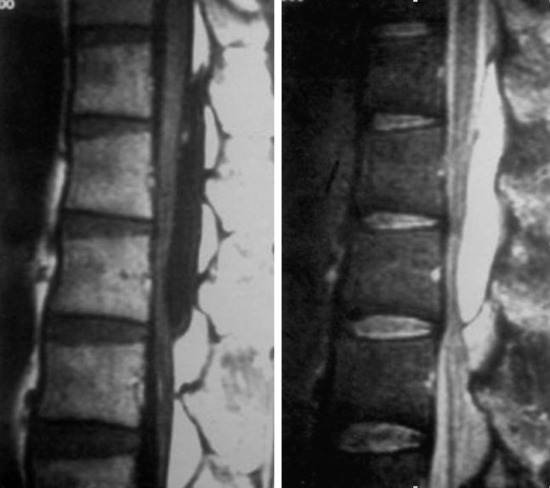
• The signal change of involved vertebral bodies is low on T1WI and high on T2WI (Figs. 2-25 and 2-26). When gadolinium is administered, diffuse enhancement pattern is observed in the bone marrow, longitudinal ligament, disc, and spinal dura (Fig. 2-27). The disc space is spared until the vertebral body is completely collapsed (Fig. 2-26).
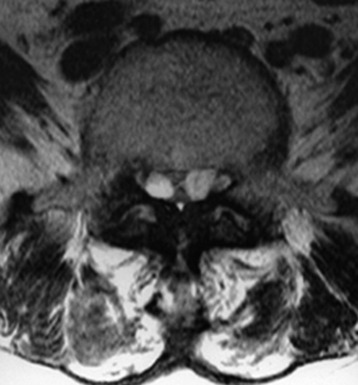
EXTRADURAL ARACHNOID CYST
EPIDEMIOLOGY
• Spinal extradural arachnoid cysts are thought to be extradural outpouchings of arachnoid that communicate with the intraspinal subarachnoid space through a small defect in the dura.18
• The pathogenesis of spinal extradural arachnoid cysts is unclear. It is known to be associated with trauma, surgery, arachnoiditis, and neural tube defects.19,20 In many cases, there is no identifiable cause, and most non-traumatic spinal extradural arachnoid cysts are thought to be congenital.19 Therefore, they are thought to arise from a congenital dural defect that allows the arachnoid membrane to herniate through the adjacent dura mater.18,21,22 The bone changes (thinning of the laminae) observed on MRI and at the time of surgery suggest a long-standing lesion with a congenital origin.
• The mechanism by which the spinal cord is compressed by such cysts is unclear, but several theories have been proposed on the pathogenetic mechanism23:
1 A one-way valve causes intermittent increased pressure within the extradural cyst, thereby compressing the spinal cord.