75
Cutaneous Signs of Drug, Child, and Elder Abuse
Drug Abuse
• The skin often displays evidence of injection and inhalation drug abuse.
• A broad spectrum of cutaneous findings can result from local and systemic effects of the drug itself, adulterants, or associated infectious agents (Tables 75.1 and 75.2; Figs. 75.1–75.9).
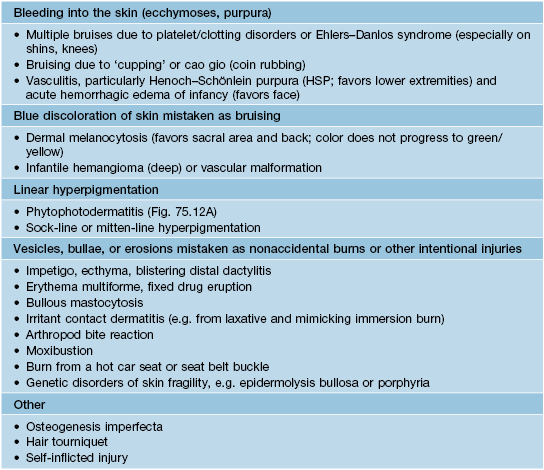
Table 75.1
Mucocutaneous signs of drug abuse.
Infections associated with drug abuse are presented in Table 75.2. A variety of cutaneous drug reactions can also develop, such as morbilliform or fixed drug eruptions, urticaria, small vessel vasculitis, and Stevens–Johnson syndrome/toxic epidermal necrolysis.
* Withdrawn from prescription drug market in 2010 in the United States and Europe.
† May also be associated with androgenetic alopecia, hirsutism, clitoral enlargement, testicular atrophy, and gynecomastia.
IV, intravenous; LSD, lysergic acid diethylamide; SC, subcutaneous.
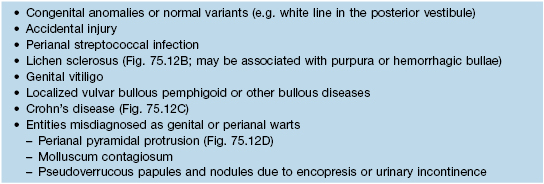
Table 75.2
Infectious complications of drug abuse.
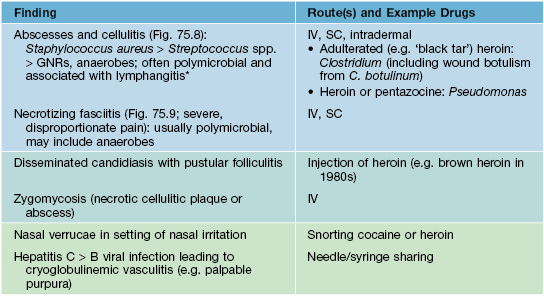
* May also be associated with osteomyelitis, septic arthritis, bacteremia, septic thrombophlebitis, and endocarditis (often tricuspid valve).
GNRs, gram-negative rods; IV, intravenous; SC, subcutaneous.

Fig. 75.1 Injection sites (‘skin tracks’) in an intravenous drug user. There is overlying hyperpigmentation and scarring of veins due to inflammation from repeated nonsterile injections as well as injections of irritating drugs and adulterants. Courtesy, Mark Pittelkow, MD.



Fig. 75.2 ‘Skin popping’ scars. A–C Multiple circular depressed scars, some with rims of post-inflammatory hyperpigmentation, admixed with circular hemorrhagic crusts overlying ulcerations. Cocaine was injected into the thighs. A, Courtesy Miguel Sanchez, MD; B, C, Courtesy, Mark Pittelkow, MD.


Fig. 75.3 Retiform purpura due to levamisole-adulterated cocaine. A, B The earlobe is a common site of involvement and purpuric lesions of the earlobe had been described previously as a side effect of levamisole. At the time of writing, up to 70% of the cocaine in the United States contained levamisole, compared to <3% of the heroin. Courtesy, Jeffrey Callen, MD.

Fig. 75.4 Atrophic depressions on the thighs and extensive calcification from multiple pentazocine injections. The calcified areas are firm upon palpation. Courtesy, Mark Pittelkow, MD.

Fig. 75.7 Coma bulla. Large bulla with subsequent erosion on the medial ankle due to a prolonged coma from barbiturate overdose. Courtesy, Mark Pittelkow, MD.

Fig. 75.8 Cellulitis of the lower extremity in an intravenous drug user. Courtesy, Mark Pittelkow, MD.

Fig. 75.9 Necrotizing fasciitis of the upper extremity with extensive tissue necrosis in an intravenous drug user. Surgical debridement has been performed. Courtesy, Mark Pittelkow, MD.


Fig. 75.6 Multiple excoriations in a cocaine addict. The patient felt ‘crawling’ in his skin. Courtesy, Mark Pittelkow, MD.
Child Abuse
• Cutaneous signs of physical abuse.
– Unexplained bruises (Fig. 75.10), curvilinear or binding marks (e.g. produced by belts, ropes, or cords), buckle imprints, and burns (e.g. from cigarettes or scalding; Fig. 75.11).



Fig. 75.10 Bruising and petechiae. A, B Bruising and petechiae of the pinna and post-auricular area in a 6-year-old boy, consistent with a hand slap by an adult. C Bruising from a belt and belt buckle on the back of an 8-year-old boy. A, B, From Hobbs CJ, Wynne JM. Physical Signs of Child Abuse. © 2001 WB Saunders; C, Courtesy, Sharon Ann Raimer, MD.


Fig. 75.11 Injuries produced by burns. A Cigarette burn. B Bullae and erosions due to dunking in hot water, with a sharp line of demarcation on the arm (arrow; ‘glove/stocking’ distribution). ‘Donut-type sparing’ on the child’s buttocks may be seen when the buttocks are held against the cooler tub while water scalds the surrounding immersed skin. Courtesy, Sharon Ann Raimer, MD.
– Delay between the injury and seeking medical care.
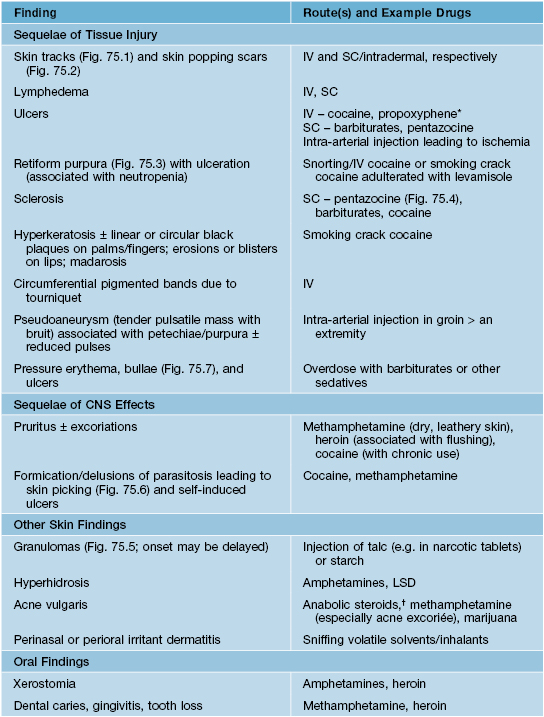
• DDx: conditions that can mimic physical and sexual abuse in children are listed in Tables 75.3 and 75.4 (Fig. 75.12).




Fig. 75.12 Cutaneous disorders that may be misdiagnosed as physical or sexual abuse. A Linear hyperpigmented streaks due to phytophotodermatitis on the back of a 2-year-old girl; the mother had lime juice on her hand when she touched the child. B Genital lichen sclerosus may have associated purpura or hemorrhagic bullae. C Cutaneous Crohn’s disease can present with vulvar erythema and swelling as well as perianal ulcers. D A perianal pyramidal protrusion in the typical location, just anterior to the anus in the midline. This finding is most common in infant girls. A, Courtesy, Anthony J. Mancini, MD; B, Courtesy, Sharon Ann Raimer, MD; C, D, Courtesy, Julie V. Schaffer, MD.
• Rx: guidelines for evaluation of suspected child abuse are available at http://pediatrics.aappublications.org/content/119/6/1232.full.pdf (physical abuse) and http://pediatrics.aappublications.org/content/116/2/506.full.pdf (sexual abuse).
Elder Abuse
• Risk factors include dementia and social isolation.
• The National Center on Elder Abuse (http://www.ncea.aoa.gov) provides resources to assist in the recognition and management of elder abuse.
For further information see Chs. 89 and 90. From Dermatology, Third Edition.