65
Cutaneous Manifestations of HIV Infection
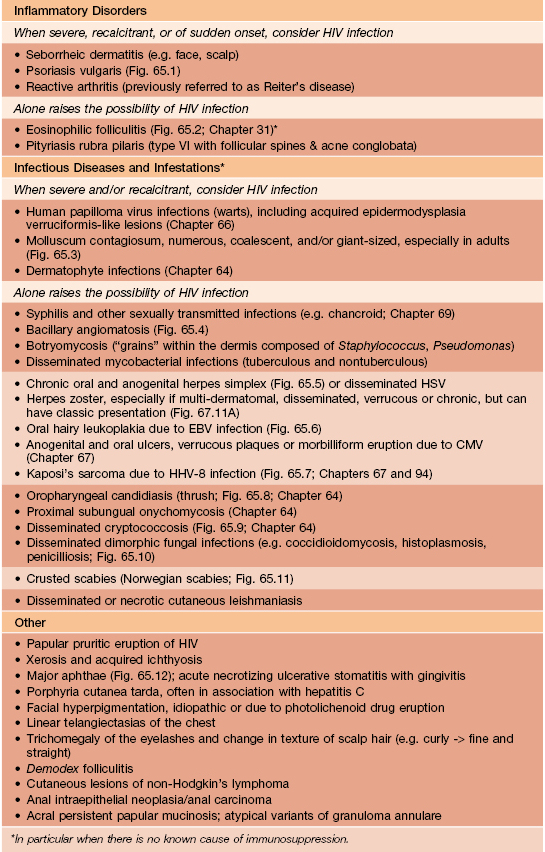
There are a number of cutaneous disorders that point to the diagnosis of HIV infection. For some, it is the mere presence of the skin disease, whereas for others, the disease is extensive or proves recalcitrant to therapy (Table 65.1; Figs. 65.1–65.12). As HIV infection is associated with immunosuppression, the clinical presentation of various infectious diseases is often reminiscent of that observed in individuals whose immunocompromised state is due to medications (e.g. CS plus chemotherapy) or underlying diseases (e.g. acute leukemia).

Fig. 65.1 Severe psoriasis in a patient with AIDS. Both sudden acute exacerbations and treatment resistance can be observed.

Fig. 65.2 Eosinophilic folliculitis. Due to associated pruritus, follicular papules are often excoriated; lesions favor the head and upper trunk. Courtesy, Clay J. Cockerell, MD.

Fig. 65.3 Molluscum contagiosum in the setting of HIV infection. Large lesions due to coalescence of individual papules. The face is a common location.

Fig. 65.4 Bacillary angiomatosis. Lesions can resemble vascular tumors or pyogenic granulomas and are a reflection of infection with Bartonella henselae or B. quintana.

Fig. 65.5 Chronic ulcerative herpes simplex viral infection in an HIV-infected patient. These slowly enlarging ulcers of the buttocks and perianal area have a characteristic scalloped border.

Fig. 65.6 Oral hairy leukoplakia. Shaggy white keratotic plaques along the lateral aspect of the tongue. A corrugated pattern is often seen. Courtesy, Charles Camisa, MD.



Fig. 65.7 Kaposi’s sarcoma in the setting of AIDS. Violaceous papules and plaques involving the face (A), palate (B), and an extremity (C). The patient also has oral candidiasis. C, Courtesy, Thomas Horn, MD.

Fig. 65.8 Both oral candidiasis and oral herpes viral infection involving the tongue. The white plaques represent the former, whereas the circular and scalloped areas of detached epithelium represent the latter. Either of these infections, and especially their combination, points to immunosuppression and the possibility of HIV infection.


Fig. 65.9 Disseminated cryptococcosis in the setting of AIDS. A Several ulcers with rolled borders. B Numerous molloscum contagiosum-like lesions. Microscopic examination and culture of either dermal scrapings or a biopsy specimen confirm the diagnosis.

Fig. 65.10 Histoplasmosis in a patient with AIDS. Disseminated papules and nodules, some with central scale-crust.

Fig. 65.11 Crusted scabies in the setting of HIV infection. Crusted scabies is often misdiagnosed as dermatitis, but these scale-crusts are teeming with mites. This form of the disease was previously referred to as Norwegian scabies.

Fig. 65.12 Major aphthae in a patient with AIDS. Resolution of these oral ulcers may require thalidomide.
In HIV-infected patients, several cutaneous diseases (e.g. disseminated coccidioidomycosis, Kaposi’s sarcoma) are AIDS-defining conditions (see http://www.cdc.gov/mmwr), whereas others such as oral hairy leukoplakia and seborrheic dermatitis can serve as early clues to the infection, i.e. when there are >500 CD4+ cells/mm3.
Epidemiology
Exanthem of Primary HIV Infection (Acute Retroviral Syndrome)
Immune Reconstitution Inflammatory Syndrome (IRIS)
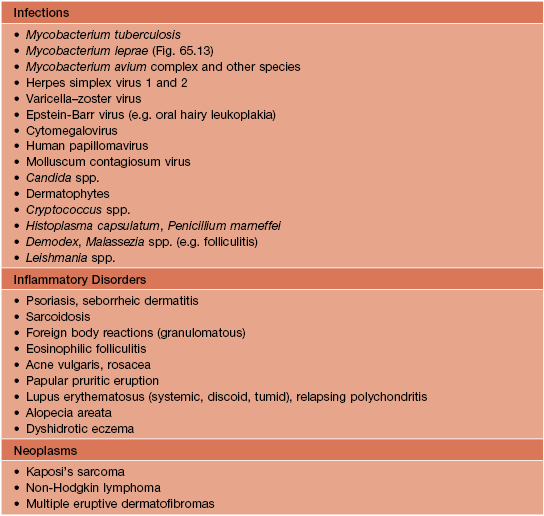
• Those disorders that can ‘flare’ or ‘worsen’ due to an increase in the ability to mount an inflammatory response following the institution of ART are outlined in Table 65.2 (Fig. 65.13).
Table 65.2
Cutaneous diseases that can ‘flare’ due to the immune reconstitution inflammatory syndrome (IRIS).
IRIS can also occur in other settings of immunosuppression (e.g. solid organ transplants, TNF administration).
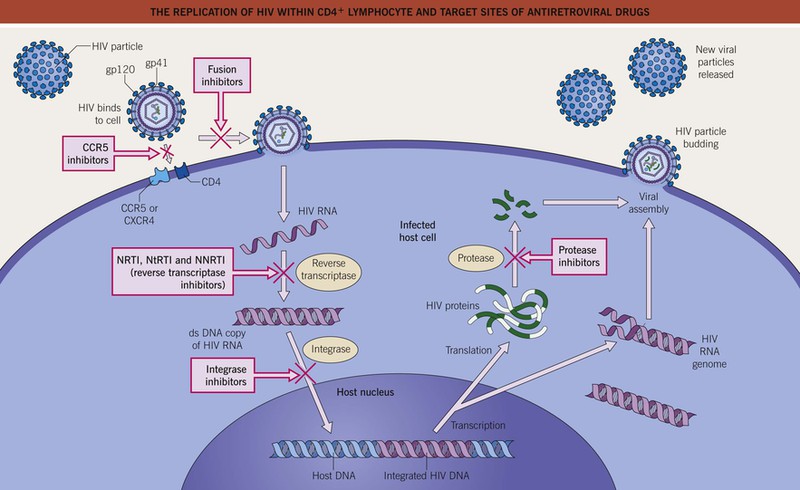
Antiretroviral Therapy (ART)
• For naive patients, initial combination ART currently consists of one of the following: (1) efavirenz/tenofovir/emtricitabine; (2) ritonavir-boosted atazanavir + tenofovir/emtricitabine; (3) ritonavir-boosted darunavir + tenofovir/emtricitabine; or (4) raltegravir + tenofovir/emtricitabine (see http://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf).
• Table 65.3 (Figs. 65.14 and 65.15) outlines the mucocutaneous side effects of these anti-retroviral drugs (Fig. 65.16); such reactions can lead to the discontinuation of the incriminated medication.
Table 65.3
Cutaneous side effects of antiretroviral therapy (ART).
In general, patients with HIV infection have an increased risk of developing drug-induced morbilliform eruptions and toxic epidermal necrolysis, e.g. to sulfonamides. Dark-colored cells = common; light-colored cells = less common. A whole cell that lacks specific drug names refers to that class of drugs, whereas in subdivided cells, it refers to the remainder of that class of drugs.
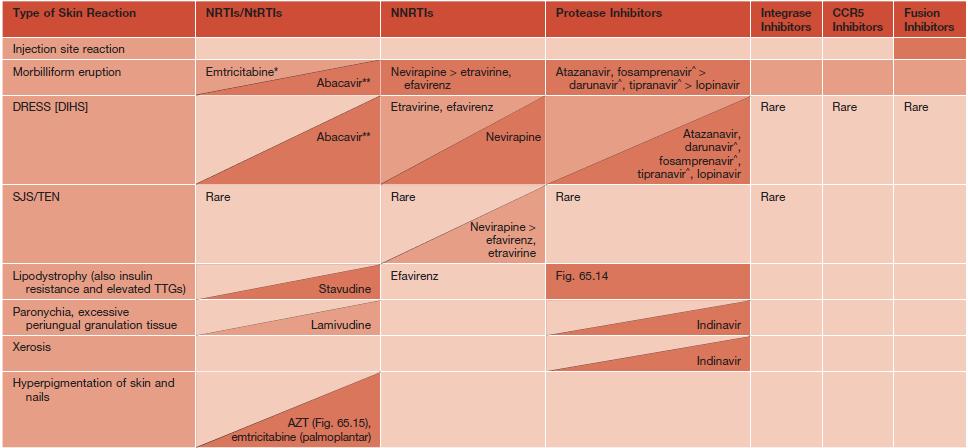

Fig. 65.14 HIV/ART-associated lipodystrophy. Marked indentation of the medial cheeks due to lipoatrophy is a characteristic finding, as is a decrease in subcutaneous fat of the extremities and an increase in abdominal fat (central obesity). Courtesy, Priya Sen, MD.

Fig. 65.15 Zidovudine-associated melanonychia. Patients receiving zidovudine (AZT) may develop longitudinal streaks, horizontal bands, or diffuse hyperpigmentation as well as oral and cutaneous hyperpigmentation.
For further information see Ch. 78. From Dermatology, Third Edition.