Chapter 33 Current Indications for Temporary and Permanent Cardiac Pacing
In the past few decades, improvements in device technology and surgical techniques have made permanent pacemaker implantation a readily performed minor surgery with a low likelihood of major complications. Similarly, temporary pacemaker insertion can often be performed at the bedside quickly and safely with a relatively limited set of tools. Nevertheless, employing cardiac pacing in a given situation remains a major clinical decision, as it has the potential for life-altering consequences for the patient. In 2008, the American College of Cardiology, the American Heart Association, and the Heart Rhythm Society (ACC/AHA/HRS) jointly issued an updated set of guidelines for cardiac pacing on the basis of a comprehensive review of available clinical data and expert opinion.1 This chapter refers to this document frequently and makes use of the ACC/AHA/HRS conventional division of indications into class I, class IIa, class IIb, and class III. The European Society of Cardiology separately released a set of guidelines for pacemaker implantation in 2007, making use of the same system for classifying indications.2
The ACC/AHA/HRS and ESC guidelines also classify the supportive data for each recommendation by assigning a level of evidence (LOE, see Appendix Table 33-1).* It is notable that of the 71 specific ACC/AHA/HRS recommendations relating to permanent cardiac pacing in adults, only 3 have LOE A, 29 have LOE B, and 39 have LOE C. In some instances, the lack of randomized trials reflects a broad consensus on the standard of care and the absence of alternatives to cardiac pacing for symptomatic bradycardia. In many other instances, however, particularly for class II indications, data from large clinical trials are scarce. The guidelines should, therefore, not be adhered to blindly but should be seen as a framework to assist with clinical decision making. Accordingly, the aim of this chapter is to review the indications for cardiac pacing in adults, including temporary pacing, permanent pacing, and multiple-site pacing, with special attention to clinical dilemmas and specific clinical situations. Device therapy in pediatric and adolescent patients and in patients with congenital heart disease will be reviewed separately.
Indications for Permanent Pacing
Disorders of Sinoatrial Conduction
The functions of the sinus node are impulse generation, impulse transmission, and modulation of heart rate in response to autonomic inputs. Patients suffering from sinus node dysfunction manifest one or more of several distinct electrocardiographic abnormalities, including sinus bradycardia, sinus pauses, bradycardia alternating with tachyarrhythmias, and failure to augment heart rate appropriately with exercise (see Appendix Table 33-2). Typically, such patients will complain of lightheadedness, fatigue, syncope, or activity intolerance. The main diagnostic tool for establishing the diagnosis of sinus node dysfunction is continuous ambulatory electrocardiographic monitoring for a period determined by the frequency of the patient’s symptoms.
No randomized trials demonstrating that pacing improves survival in patients with sinus node dysfunction have been conducted, and at least one small series suggests that short-term prognosis is good in this patient population.3 Thus, the primary role for pacing is to treat symptoms, prevent adverse events such as syncope, and permit therapy with drugs that slow heart rate, as required to treat other medical conditions. Before considering pacemaker implantation, reversible causes of sinus node dysfunction should be ruled out (Table 33-1). The indications for permanent pacing in sinus node dysfunction are summarized in Appendix Table 33-3. When sinus pauses or bradycardia coincide temporally with the patient’s symptoms and a causal link can be established, a pacemaker is indicated; this is a class I indication. Conversely, when the patient’s typical symptoms occur during periods when monitoring reveals a normal heart rate, pacemaker implantation would not be expected to provide any benefit; this is, therefore, a class III indication.
Table 33-1 Reversible Causes of Sinus Bradycardia and Atrioventricular Block
| TYPE OF CAUSE | SPECIFIC CAUSE |
|---|---|
| Cardiac | Myocardial ischemia |
| Viral myocarditis | |
| Lyme disease | |
| Rheumatic fever | |
| Endocarditis | |
| Post–cardiac surgery | |
| Post–cardiac transplant | |
| Athletic training | |
| Autonomic nervous system | Neurocardiogenic syncope |
| Carotid hypersensitivity | |
| Vagal stimulation | |
| Drugs and medications | β-Adrenergic blockers |
| Calcium channel blockers | |
| Clonidine | |
| Digitalis | |
| Ivabradine | |
| Reserpine, methyldopa | |
| Class IA antiarrhythmic drugs | |
| Class IC antiarrhythmic drugs | |
| Class III antiarrhythmic drugs | |
| General anesthetics | |
| Tricyclic antidepressants | |
| Phenothiazines | |
| Lithium | |
| Phenytoin | |
| Cholinesterase inhibitors | |
| Hypothermia | |
| Hypothyroidism | |
| Neurologic | Elevated intracranial pressure |
| Spinal cord injury | |
| Electrolyte imbalances | Hypokalemia |
| Hyperkalemia | |
| Hypercalcemia | |
| Pulmonary | Obstructive sleep apnea |
| Prolonged hypoxia |
In patients with suspected sinus node dysfunction, particularly in those manifesting some degree of activity intolerance, exercise testing can be a very helpful adjunctive assessment of sinus node function. Chronotropic incompetence is often defined as failure to achieve a heart rate of 80% of age-adjusted maximum predicted heart rate with exercise.4 However, the critical issue in such cases is whether heart rate is sufficient to meet physiologic demands. The clinician should, therefore, not place too much importance on the specific rate achieved but should determine whether sinus node function is the main factor limiting the patient’s ability to exercise. Where this is the case, pacemaker implantation is warranted; this is a class I indication, even when heart rate is normal at rest and sinus pauses are not identified on monitoring.
Disorders of Atrioventricular Conduction
The function of the atrioventricular (AV) node is to delay impulse propagation from atria to ventricles to the extent necessary to optimize ventricular filling. This delay varies physiologically over a large range and is heavily influenced by autonomic tone and heart rate. The function of the bundle of His, which passes from the AV node to the ventricle through the central fibrous body, is to transmit the electrical impulse rapidly from the atrium to the ventricle. Conduction time through the bundle of His is rapid and does not vary with heart rate under normal conditions. Conduction slowing or block can occur in the AV node, the bundle of His, or both, and characteristic electrocardiogram (ECG) patterns are present, as well as differences in prognosis, depending on the location and severity of the block. In general, when the block is above the level of the His bundle (supra-His), prognosis for progression to a high-grade block is better than when the block is at or below the level of the His bundle (intra-His or infra-His).5 Symptoms caused by an AV block can include fatigue, lightheadedness, and syncope; a persistent high-grade AV block can result in heart failure caused by bradycardia and loss of AV synchrony and can predispose to ventricular arrhythmias.
First-Degree Atrioventricular Block
First-Degree AV block is defined as P-R interval exceeding 0.2 seconds and is often reflective of incipient AV nodal disease, though it can be a normal finding in patients at rest with high vagal tone. Recent data from the Framingham cohort suggest that in the long term, patients with first-degree AV block have a significantly higher risk of requiring pacemaker implantation and have a higher mortality rate.6 However, with a few exceptions (discussed below), the short-term prognosis for those with isolated first-degree AV block is excellent, so pacemaker implantation is, in general, not indicated in asymptomatic patients as a prophylactic measure (class III). However, a few indications for pacing are recognized for first-degree AV block (summarized in Appendix Table 33-4).
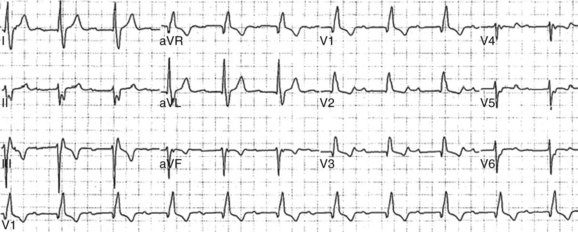
Some patients with marked first-degree AV block (P-R interval >0.3 seconds) have symptoms that may warrant pacemaker implantation.7 In these patients, ventricular activation is so delayed that the subsequent atrial activation occurs shortly after the QRS complex on the surface ECG, resulting in atrial contraction against closed AV valves (Figure 33-1). Patients with severe left ventricular dysfunction and markedly prolonged P-R intervals may experience hemodynamic compromise caused by impaired ventricular filling and diastolic AV valvular regurgitation.8 Often, reducing the dosages of AV nodal blocking medications in these patients can shorten the P-R interval and improve symptoms. Where this is not possible, restoration of AV synchrony with dual-chamber pacing and a normal AV delay can solve the problem, and this is a class IIa indication. However, ventricular pacing under these circumstances carries with it the potential deleterious effects of intraventricular dyssynchrony, so consideration should be given to biventricular pacing in such instances, especially when left ventricular function is not normal (see below).
Finally, patients with several neuromuscular diseases (see Appendix Table 33-5) often have rapidly progressive AV conduction system disease. Even in asymptomatic patients with these disorders, marked first-degree AV block should prompt consideration of pacemaker implantation as a prophylactic measure.
Type I Second-Degree Atrioventricular Block
Second-degree AV block is divided into type I and type II on the basis of the ECG pattern. In type I, the P-R interval lengthens before the nonconducted beat and shortens on the first beat after the nonconducted beat (Wenckebach conduction); in type II, the P-R interval is fixed. In general, type I second-degree AV block suggests a supra-His level of block and is associated with a more benign prognosis, while type II occurs with intra-His or infra-His conduction system disease and has a higher rate of progression to complete heart block.5 It should be remembered that in pathologic conditions, it is possible for any component of the conduction system, even the structures below the AV node, to exhibit Wenckebach conduction. Thus, type I second-degree AV block has a benign prognosis only when it is caused by supra-His block, which is usually the case when the QRS is narrow.
Regardless of the level of block, patients with symptomatic bradycardia resulting from second-degree AV block from irreversible causes or essential drug therapy should undergo permanent pacemaker implantation (class I). In the setting of high vagal tone such as sleep or in highly conditioned athletes at rest, type I second-degree AV block is frequently observed and is a normal finding.9 For asymptomatic patients, pacemaker implantation is therefore not recommended (class III). However, as with first-degree AV block, patients with type I second-degree AV block can have symptoms caused by loss of AV synchrony, and pacemaker implantation should be considered for this indication (class IIa) as well as for symptomatic bradycardia. Indications for pacing in type I second-degree AV block are summarized in Appendix Table 33-4.
High-Grade Atrioventricular Block
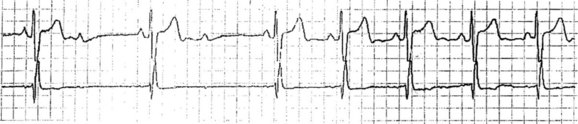
Patients with type II second-degree AV block (Figure 33-2) have a higher rate of progression to third-degree AV block, particularly in the setting of intraventricular conduction abnormalities. From the point of view of cardiac pacing, advanced second-degree AV block and third-degree AV block should be grouped together in a single high-risk category, and pacemaker implantation is the only reasonable treatment when reversible causes cannot be identified (see Appendix Table 33-6). Randomized clinical trials comparing pacing with conservative management are not available, but considerable nonrandomized evidence exists that pacing for patients with high-grade AV block results in a prolongation of life and reduction in morbidity.10
Third-degree AV block and consequent AV dissociation are almost always symptomatic, though the symptoms can vary in severity from mild dizziness and exercise intolerance to syncope or even sudden death, depending on the rate of the escape rhythm. In addition to medications that affect AV nodal conduction, a number of reversible causes of high-grade AV block, including myocardial ischemia, exist, and these should be ruled out before considering permanent pacing (see Table 33-1). Often, a careful history and an ECG are sufficient to rule out reversible causes of complete heart block, but where uncertainty remains, it is appropriate to perform further diagnostic testing. Brief periods of third-degree heart block can occur in situations of high vagal tone; where these are transient or occur exclusively in sleep and are accompanied by adequate escape rhythms, pacemaker implantation is not always warranted.
Disorders of Intraventricular Conduction
The functions of the distal limbs of the conduction system (bundle branches, fascicles, and Purkinje fibers) are to transmit the electrical impulse rapidly to ventricular muscle and to ensure coordinated activation of the ventricles. The bundle of His bifurcates into the right bundle branch and the left bundle branch at the crest of the interventricular septum. Bundle branches then ramify into complex networks of specialized conduction fibers, known as fascicles. On the left, this complex fascicular system is conventionally divided into the left anterior fascicle and the left posterior fascicle. Dysfunction and failure of impulse transmission can occur in any combination of these bundles and fascicles, with or without superimposed AV block, leading to a variety of intraventricular conduction disturbances. Cardiac pacing has a role in a subset of patients with intraventricular conduction system disease (see Appendix Table 33-7).
Hemiblocks and Bundle Branch Block
Individuals without conduction system disease may develop bundle branch block or fascicular block at very high heart rates, during tachyarrhythmias, or, less commonly, at very low heart rates (phase 4 aberrancy). Also, a small percentage of normal healthy individuals have right or left bundle branch block as a congenital variant. In general, block of a single fascicle (right bundle branch block, left anterior hemiblock, or left posterior hemiblock), with or without accompanying first-degree AV block, does not warrant consideration of pacemaker implantation without evidence of high-grade AV block.11 The only major exceptions to this rule are patients with selected neuromuscular diseases, in whom any fascicular block may warrant consideration of pacemaker implantation because of the unpredictable nature of disease progression (class IIb).
Although complete left bundle branch block can be seen in the presence of disease of both the anterior and posterior fascicular systems (particularly in the setting of a large myocardial infarction), it more commonly results from a proximal lesion in the conduction system and should not be grouped with bifascicular blocks. If a patient presents with bundle branch block with left-axis, first-degree AV block and syncope, it may be reasonable to assess intraventricular conduction with an invasive electrophysiology study. An H-V interval less than 0.1 seconds or the finding of pathologic infra-His block with pacing may warrant consideration of pacemaker implantation.12
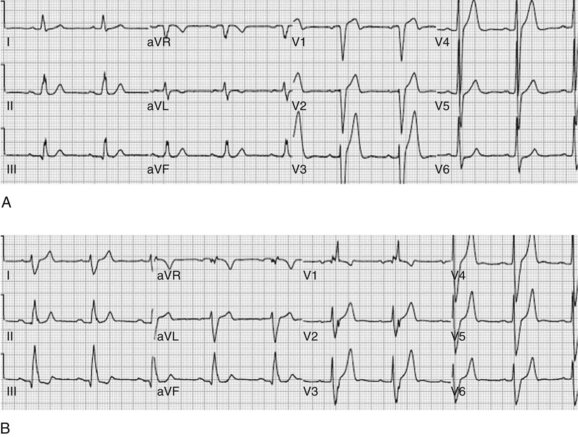
When complete left bundle branch block alternates with right bundle branch block, it suggests the presence of severe, widespread infra-His conduction system disease. The same is true when right bundle branch block with left anterior hemiblock alternates with right bundle branch block with left posterior hemiblock. Whether this alternation occurs within a single ECG or rhythm strip, or on successive ECGs recorded on separate days, this condition carries a high risk for progression to complete heart block and is a class I indication for pacemaker implantation, even in the absence of symptoms (Figure 33-3).
Chronic Bifascicular Block
Chronic bifascicular block is present with involvement of one of the left-sided fascicles plus the right bundle branch. Trifascicular block is a somewhat confusing term often used to refer to bifascicular block in the presence of first-degree AV block. The prognostic significance of bifascicular blocks varies according to the site of the block and the presence or absence of other forms of heart disease. With a few important exceptions (detailed below), the annual rate of progression to complete heart block in the asymptomatic patient is low, even though most patients who develop third-degree AV block have bifascicular block at some point.13 When bifascicular block is accompanied (even transiently) by type II second-degree AV block, advanced second-degree AV block, or third-degree AV block, a high risk of progression to complete heart block is present, and pacemaker implantation is warranted whether or not symptoms are present (class I).
Disorders of the Autonomic Nervous System
The cardiovascular system, and the sinoatrial (SA) node and AV node within the heart, are richly innervated with parasympathetic and sympathetic fibers. Particular forms of autonomic nervous system dysfunction can cause symptomatic bradycardia, which, in some cases, can be responsive to cardiac pacing (see Appendix Table 33-8).
Neurocardiogenic Syncope
Even in patients with some degree of cardioinhibition, SA nodal and AV nodal functions are typically normal, so cardiac pacing is not first-line therapy. The large, randomized, placebo-controlled Vasovagal Pacemaker Study II (VPS-II) has been performed to test pacing in neurocardiogenic syncope.14 The results showed no aggregate benefit to pacing in general, though it may be reasonable to use pacing in certain subpopulations (patients with prolonged asystole, minimal prodrome, or no response to other treatments). For patients with symptomatic documented cardioinhibition either on tilt-table testing or spontaneously, a class IIb indication for permanent pacing is present, if the bradycardia is refractory to lifestyle changes and maneuvers. For patients in high-risk occupations (transportation, construction, operation of heavy machinery) or for those with prolonged periods of asystole (<5 seconds), pacemaker implantation may be the safest course. However, these patients should be cautioned that pacing will not prevent attacks and may not be sufficient to abort the attacks once they are in progress. The main role for pacing in these situations is to blunt the severity of the episodes, and in some cases, when minimal prodromal symptoms are present, pacing can provide additional time for the patient to undertake abortive maneuvers.
Iatrogenic Bradycardia
Medications
All patients presenting with symptomatic bradycardia should be thoroughly questioned about medication use, and, where possible, medications that cause bradycardia should be discontinued. Commonly prescribed classes of medications that can cause bradycardia are listed in Table 33-1. In many instances, these medications may have strong indications (for example, β-blockers in patients with coronary artery disease). It may, therefore, be necessary to implant a permanent pacemaker, which will help continue therapy with essential medications (class I). The risks of pacemaker implantation should be carefully weighed against the risk of discontinuing the medication in question, and pacemaker implantation should only be undertaken when the risk/benefit profile is favorable. In this context, it should be emphasized that clinically relevant doses of AV nodal blocking agents commonly unmask pre-existing AV nodal disease but typically do not cause AV block in patients with otherwise normal conduction. In one series, while 41% of patients with high-grade AV block experienced short-term resolution with cessation of nodal blocking drugs,15 more than half these patients subsequently experienced recurrence of high-grade AV block off the medication. Only about 15% of patients with high-grade AV block while on nodal agents had lasting resolution of AV block with cessation of drug therapy. Thus, it is important to monitor closely even those patients with short-term resolution of AV block after cessation of nodal agents, as the majority of these individuals will eventually need pacemaker implantation.
Procedures and Surgeries
The AV conduction axis can sustain significant damage during cardiac surgery, particularly aortic and mitral valve surgery, and temporary pacing is often necessary post-operatively.16 When AV conduction does not recover after a reasonable period (we typically wait 7 days), a permanent pacemaker should be implanted (class I).17,18
Tachyarrhythmias
Although medications, catheter ablation, and ICD implantation are the primarily modalities for treating tachyarrhythmias, cardiac pacing does have a role in certain circumstances, both for termination of supraventricular tachyarrhythmias and for prevention of triggered ventricular arrhythmias (see Appendix Table 33-9). Although pacing is used in the automatic detection and termination of ventricular tachycardia, pacing systems with this capacity should also have the ability to defibrillate in the event that pacing accelerates the rhythm or causes degeneration into ventricular fibrillation. Pacemakers without ICD function should therefore not be implanted for detection and termination of ventricular tachycardia.
Multiple-Site Pacing
Biventricular Pacing in Heart Failure
Dyssynchronous ventricular contraction caused by abnormal ventricular activation can be deleterious. Many patients with heart failure caused by left ventricular (LV) systolic dysfunction have broad QRS intervals arising from the involvement of the intraventricular conduction system, and some have a broad QRS intervals in the setting of frequent RV apical pacing. Two landmark clinical trials, Comparison of Medical Therapy, Pacing, Defibrillation in Chronic Heart Failure (COMPANION) and Cardiac Resynchronization-Heart Failure trial (CARE-HF), have established a role for biventricular pacing or cardiac resynchronization therapy (CRT) in selected patients with heart failure with reduced ejection fraction, both for reduction of symptoms and reduction in mortality.19,20 These studies included patients with LVEF 35% or less and QRS interval less than 0.12 seconds regardless of the type of intraventricular conduction abnormality. Thus far, the guidelines have focused on patients with New York Heart Association (NYHA) class III and ambulatory class IV symptoms who are already on recommended medical therapy. The importance of ensuring that patients with heart failure are on medical therapy cannot be overemphasized, as patients can move from NYHA class III/IV to class I on medications alone, and the ejection fraction can improve significantly. Among these patients, biventricular device implantation for restoration of mechanical synchrony is a class I indication for those in sinus rhythm and class IIa for those in atrial fibrillation or who depend on ventricular pacing. Although the guidelines do not describe an indication for patients with NYHA class IV symptoms who depend on positive inotropes or are nonambulatory, we have occasionally found that such patients can benefit dramatically from CRT, to the point of weaning the patients off inotropes so that the patients can leave the hospital.19,21
Recently, results from the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT) trial22 have shown that with biventricular ICD implantation, a significant reduction occurs in mortality rates and hospitalizations for heart failure, even in NYHA class I/II patients, which has raised the possibility of a considerable expansion in the indications for CRT.19 At the time of the writing of this chapter, these data did not yet affect clinical practice but are likely to have a major impact in the near future. As for now, the 2008 ACC/AHA/HRS guidelines recognize a class IIb indication for patients with LVEF less than 35% and NYHA class I or II heart failure when pacemaker implantation is planned for other indications and frequent ventricular pacing is expected.
Multiple-Site Atrial Pacing
A number of small clinical series and one moderate-sized randomized trial have been performed to evaluate the potential for multiple-site atrial pacing to reduce atrial fibrillation. Thus far, with the possible exception of patients with marked intra-atrial conduction delay that manifests as surface P-wave duration less than 0.18 seconds, no benefit in terms of symptoms, reduction in atrial fibrillation, or adverse cardiac events have been reported.23 Therefore, no recognized indication for pacing to prevent atrial fibrillation in patients without any other indication for permanent pacing (class III) exists at present.
Permanent Pacing in Specific Clinical Situations
Myocardial Infarction
It is common for patients to sustain damage to the cardiac conduction system from myocardial infarction (MI), and the guidelines recognize a separate class of indications for this group of patients, since acquired AV block in the post-MI setting has a distinct prognostic significance. As with all patients manifesting intraventricular conduction disturbances, all symptomatic AV blocks that are not transient warrant permanent pacing (class I). The guidelines also recognize additional class I indications for patients who have no symptoms but have persistent second-degree AV block with alternating bundle branch block, third-degree AV block, and transient second-degree or third-degree AV block that is believed to be either intra-His or Infra-His. Pacemaker implantation can also be considered for patients with persistent second-degree or third-degree AV block that is supra-His (class IIb). However, AV block that is transient and not accompanied by intraventricular conduction defects or that is accompanied only by left anterior fascicular block has a low rate of progression to complete heart block, and prophylactic pacemaker implantation is not recommended (Appendix Table 33-10). Similarly, bundle branch block or fascicular block without AV block does not warrant pacemaker implantation, nor does persistent first-degree AV block with bundle branch block that predates the infarction (class III).
Hypertrophic Cardiomyopathy
Some randomized clinical trials have demonstrated subjective improvement in symptoms as well as in physiologic endpoints, but others have shown no overall improvement in the quality of life or any alteration in the course of the disease.24,25 Patients with hypertensive hypertrophic cardiomyopathy and older adults may be subpopulations that derive more benefit, whereas pacing is more difficult in those with rapid atrial rates or brisk AV nodal conduction. Overall, data are inconclusive but certainly do not support the idea of routine pacing in these patients. However, the guidelines do recognize a class IIb indication for medically refractory symptomatic hypertrophic cardiomyopathy with resting or provoked outflow tract obstruction (Appendix Table 33-11). Asymptomatic patients, those with symptoms that are medically controlled, and those with symptoms but no documented outflow tract obstruction are not candidates for pacing (class III).
After Cardiac Transplantation
Patients who have received transplants are also vulnerable to coronary vasculopathy, which frequently manifests as conduction system dysfunction.26,27 Therefore, after transplantation, pacemaker implantation can be considered in patients with recurrent syncope of undetermined cause, even without clear evidence of bradyarrhythmia (class IIb). Conduction system dysfunction can also be evident in acute rejection. While comprehensive data are not available on the long-term prognosis of patients with bradyarrhythmias and syncope in the setting of rejection, it is reasonable to consider permanent pacing if the bradyarrhythmia is persistent, even after the rejection has been controlled (Appendix Table 33-12).
Indications for Temporary Pacing
Temporary Pacing Modalities
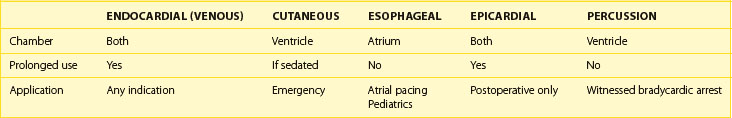
Temporary cardiac pacing can be achieved with any of several modalities (see Table 33-2). Precordial percussion can result in ventricular systoles in the setting of an asystolic arrest and can be used until transcutaneous electrodes can be placed. In general, given its morbidity, transcutaneous pacing should be reserved for emergent situations and ideally in unconscious or sedated patients.28,29 Esophageal pacing is similarly morbid and often requires relatively large amounts of current delivery for ventricular capture. It is seldom used in adult patients but may have a role in infants and children for the diagnosis and pace termination of atrial arrhythmias. Epicardial lead placement is usually performed as a prophylactic measure against bradycardia after cardiac surgery. It is common for inflammation to occur around the epicardial pacing leads, which results in a rise in pacing threshold and ultimately failure of the pacing system.30
Acute Myocardial Infarction
A variety of conduction disturbances can occur during acute MI, and any component of the conduction system can be involved. The ACC/AHA guidelines on the management of acute MI contain a section on the indications for temporary pacemaker insertion based on the prognostic significance of various bradyarrhythmias in the setting of acute MI.31
The development of new intraventricular conduction abnormalities in acute MI, particularly in conjunction with an anterior MI, is ominous and portends a worse prognosis in terms of the infarct size, hemodynamics, and the development of a complete heart block. A simple risk score (Table 33-3) has been devised to stratify patients and identify the development of a complete heart block in the setting of an acute MI.32 Temporary pacemaker placement should be considered for patients at a moderate-to-high risk of progression to complete heart block, even without symptoms or hemodynamic compromise. These include patients with pre-existing intraventricular conduction system disease with new AV block and patients with new intraventricular conduction system disease (see Appendix Table 33-13). It should be emphasized that these guidelines are distinct from those governing the indications for permanent pacing after the acute phase of MI. Many patients will need pacing only for the acute phase, particularly after successful revascularization.
Table 33-3 Risk Score for Prediction of High-Grade Atrioventricular Block in Acute Myocardial Infarction
| ABNORMALITY | POINTS |
|---|---|
| First-degree AV block | 1 |
| Type I second-degree AV block | 1 |
| Type II second-degree AV block | 1 |
| LAFB or LPFB | 1 |
| RBBB or LBBB | 1 |
| TOTAL SORE | RISK OF COMPLETE HEART BLOCK |
|---|---|
| 0 | 1.2% |
| 1 | 7.8% |
| 2 | 25% |
| 3 | 36.4% |
AV, Atrioventricular; LAFB, left anterior fascicular block; LPFB, left posterior fascicular block; RBBB, right bundle branch block; LBBB, left bundle branch block.
Modified from Lamas GA, Muller JE, Turi ZG, et al: A simplified method to predict occurrence of complete heart block during acute myocardial infarction, Am J Cardiol 57:1213–1219, 1986.
Bradyarrhythmias
In patients with significant bradycardia accompanied by symptoms of cerebral hypoperfusion, hemodynamic compromise, heart failure, or cardiac ischemia is present and in whom chronotropic agents are either ineffective or contraindicated, temporary pacemaker insertion should be considered. Often, such patients will ultimately require permanent pacemaker implantation, but necessary cardiac pacing should not be delayed while the workup for the cause of bradycardia is under way. Many reversible causes of bradycardia and conduction system abnormalities exist (see Table 33-1), and temporary pacing can be invaluable while the appropriate diagnostic testing is performed. Temporary pacing may also be required for pacemaker-dependent patients who require lead or device revision, with an obligatory delay between explantation of an old device and implantation of a new device (for example, in pacemaker lead infection).
Appendix Table 33-1 Classification of Indications for Pacemaker Implantation
| INDICATION | DESCRIPTION |
|---|---|
| Class I | Pacing is useful and effective and should be considered. |
| Class IIa | The weight of evidence is in favor of the usefulness or effectiveness of pacing, but some divergence of opinion exists. It is reasonable to consider pacing. |
| Cass IIb | The usefulness and effectiveness of pacing is less well established, and considerable divergence of opinion exists. Pacing can be considered. |
| Class III | Pacing is not useful or effective and in some cases may be harmful. Pacing should not be considered. |
| LEVEL OF EVIDENCE | |
| A | Data are derived from multiple randomized clinical trials or meta-analyses, and multiple populations were evaluated. |
| B | Data are derived from a single randomized trial or nonrandomized study, or limited populations were evaluated. |
| C | Only consensus opinion of experts, case studies, with very limited populations evaluated, or pacing is standard of care. |
Appendix Table 33-2 Clinical Manifestations of Sinus Node Dysfunction
| SYNDROME | DESCRIPTION |
|---|---|
| Sinus bradycardia | Resting heart rate <60 beats/min with typical symptoms |
| Sinus arrest | Symptomatic sinus pause <3 seconds while awake |
| Tachyarrhythmia-bradyarrhythmia syndrome | Alternating periods of tachyarrhythmia, usually atrial fibrillation, with sinus bradycardia Postconversion sinus pauses |
| Chronotropic incompetence | Failure to augment heart rate appropriately with exercise. Inability to achieve 80% of age-appropriate maximum predicted heart rate |
Appendix Table 33-3 Permanent Pacing for SND
| CLASS | INDICATION |
|---|---|
| Class I | SND with documented symptomatic bradycardia |
| Symptomatic chronotropic incompetence | |
| Symptomatic sinus bradycardia resulting from essential drug therapy | |
| Class IIa | SND with heart rate <40 beats/min and symptoms of bradycardia, without a demonstration of association between symptoms and bradycardia |
| Unexplained syncope with SND, either spontaneous or provoked | |
| Class IIb | Minimally symptoms with chronic heart rate <40 beats/min while awake |
| Class III | Asymptomatic SND |
| Symptomatic SND resulting from non-essential drug therapy | |
| SND with symptoms that occur in the absence of bradycardia |
SND, Sinus node dysfunction.
Appendix Table 33-4 Permanent Pacing for First-Degree and Type 1 Second-Degree AV Block
| CLASS | INDICATION |
|---|---|
| Class I | Symptomatic bradycardia resulting from type I second-degree AV block |
| Class IIa | First-degree AV block or type I second-degree AV block with symptoms similar to those of pacemaker syndrome or hemodynamic compromise |
| Class IIb | Neuromuscular diseases with first-degree AV block or type I second-degree AV block |
| Class III | Asymptomatic first-degree AV block or type I second-degree AV block |
AV, Atrioventricular.
Appendix Table 33-5 Neuromuscular Disorders Associated with Conduction System Disease
| SYNDROME |
Appendix Table 33-6 Pacing for High-Grade Atrioventricular block
| CLASS | INDICATION |
|---|---|
| Class I | Symptomatic bradycardia or ventricular arrhythmias due to AV block |
| Essential drug therapy that results in symptomatic bradycardia | |
| Awake, asymptomatic patients in sinus rhythm with periods of asystole <3.0 seconds, escape rate <40 beats/min, or escape rhythm that is below the AV node | |
| Awake asymptomatic patients with atrial fibrillation, bradycardia, and one or more pauses of at least ≥5 seconds | |
| After catheter ablation of the AV junction | |
| AV block after cardiac surgery that is not expected to resolve | |
| Neuromuscular diseases, with or without symptoms | |
| Asymptomatic patients with average awake ventricular rates of 40 beats/min or faster if cardiomegaly or left ventricular dysfunction is present, or if the site of block is below the AV node | |
| Exercise-induced second-degree or third-degree AV block in the absence of myocardial ischemia | |
| Class IIa | Persistent third-degree AV block with an escape rate <40 beats/min in an asymptomatic patient without cardiomegaly |
| Asymptomatic second-degree AV block at intra-His or infra-His levels found at electrophysiology study | |
| Asymptomatic type II second-degree AV block with a narrow QRS | |
| Class IIb | AV block in the setting of drug use or toxicity that is expected to recur even when the drug is withdrawn |
| Class III | Reversible AV block that is expected to resolve and is unlikely to recur |
AV, Atrioventricular.
Appendix Table 33-7 Permanent Pacing for Intraventricular Conduction Disturbances
| CLASS | INDICATION |
|---|---|
| Class I | Alternating bundle branch block |
| Bifascicular block with type II second-degree or third-degree AV block | |
| Class IIa | Bifascicular block and syncope when other causes have been excluded |
| Bifascicular block with H-V interval >0.1 second | |
| Bifascicular block with nonphysiologic pacing-induced infra-His block | |
| Class IIb | Bifascicular block with neuromuscular disease |
| Class III | Bifascicular block without AV block or symptoms |
| Trifascicular block without symptoms |
AV, Atrioventricular.
Appendix Table 33-8 Permanent Pacing for Autonomic Nervous System Dysfunction
| CLASS | INDICATION |
|---|---|
| Class I | Carotid sinus hypersensitivity causing syncope |
| Class IIa | Carotid sinus hypersensitivity with asystole of <3 seconds and syncope when other causes have been excluded |
| Class IIb | Neurocardiogenic syncope with significant symptoms and documented bradycardia either spontaneously or at tilt-table testing |
| Class III | Carotid sinus hypersensitivity with vague symptoms or no symptoms |
| Situational vasovagal syncope in which avoidance behavior is effective and preferred |
Appendix Table 33-9 Permanent Pacing for Termination and Prevention of Tachyarrhythmias
| CLASS | INDICATION |
|---|---|
| Class I | Sustained, pause-dependent ventricular tachycardia, with or without Q-T interval prolongation |
| Class IIa | High-risk patients with congenital LQTS |
| Recurrent supraventricular tachycardia that is reproducibly terminated by pacing when catheter ablation, drugs, or both fail to control the arrhythmia or produce intolerable side effects | |
| Class IIb | Prevention of symptomatic, drug-refractory atrial fibrillation in patients with coexisting sinus node dysfunction |
| Class III | Frequent or complex ventricular ectopy without sustained ventricular tachycardia in the absence of LQTS |
| Torsades de pointes ventricular tachycardia from reversible causes | |
| Prevention of atrial fibrillation without any other indication for pacemaker implantation |
LQTS, Long QT syndrome.
Appendix Table 33-10 Permanent Pacing After the Acute Phase of Myocardial Infarction
| CLASS | INDICATION |
|---|---|
| Class I | Persistent and symptomatic second-degree or third-degree AV block |
| Persistent second-degree intra-His or infra-His AV block with alternating bundle branch block, or third-degree intra-His or infra-His AV block | |
| Transient second-degree or third-degree intra-His or infra-His AV block with associated bundle branch block | |
| Class IIa | None |
| Class IIb | Persistent asymptomatic second-degree or third-degree supra-His AV block |
| Class III | Transient AV block without intraventricular conduction defects |
| Transient AV block with isolated left anterior fascicular block | |
| Bundle branch block or fascicular block without AV block | |
| Persistent first-degree AV block with bundle branch block that is not new |
AV, Atrioventricular.
Appendix Table 33-11 Permanent Pacing to Treat Obstruction in Hypertrophic Cardiomyopathy
| CLASS | INDICATION |
|---|---|
| Class I | None |
| Class IIa | None |
| Class IIb | Medically refractory symptomatic patients with hypertrophic cardiomyopathy and significant resting or provoked outflow tract obstruction |
| Class III | Patients without symptoms or with medically controlled symptoms |
| Symptomatic patients without LVOT obstruction |
Appendix Table 33-12 Permanent Pacing After Cardiac Transplantation
| CLASS | INDICATION |
|---|---|
| Class I | Persistent inappropriate symptomatic bradycardia not expected to resolve |
| Class IIa | None |
| Class IIb | Prolonged bradycardia that limits recovery after cardiac transplantation |
| Syncope after cardiac transplantation, even when bradycardia has not been documented |
Appendix Table 33-13 Temporary Pacing in Acute Myocardial Infarction
| CLASS | INDICATION |
|---|---|
| Class I | Asystole |
| Symptomatic bradycardia | |
| Third-degree AV block | |
| Alternating bundle branch block: RBBB/LBBB or RBBB + LAFB/LPFB | |
| Type II second-degree AV block with new bundle branch block | |
| Type II second-degree AV block with bifascicular block | |
| Class IIa | Type II second-degree AV block with narrow QRS |
| Type II second-degree AV block with any fascicular block (anterior MI) | |
| Type II second-degree AV block with old bundle branch block | |
| Type I second-degree AV block with new bundle branch block | |
| Type I second-degree AV block with bifascicular block | |
| First-degree AV block with new bundle branch block | |
| First-degree AV block with bifascicular block | |
| Class IIb | Type II second-degree AV block with old bundle branch block |
| Type I second-degree AV block with old bundle branch block | |
| First-degree AV block with old bundle branch block | |
| Class III | First-degree AV block with normal QRS |
| Type I second-degree AV block with normal QRS | |
| Accelerated idioventricular rhythm | |
| Old bundle branch block or fascicular block without AV block |
AV, Atrioventricular; LAFB, left anterior fascicular block; LPFB, left posterior fascicular block; RBBB, right bundle branch block; LBBB, left bundle branch block; MI, myocardial infarction.
Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350(21):2140-2150.
Cheng S, Keyes MJ, Larson MG, et al. Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. JAMA. 2009;301(24):2571-2577.
Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352(15):1539-1549.
Connolly SJ, Sheldon R, Thorpe KE, et al. Pacemaker therapy for prevention of syncope in patients with recurrent severe vasovagal syncope: Second Vasovagal Pacemaker Study (VPS II): A randomized trial. JAMA. 2003;289(17):2224-2229.
Edhag O, Swahn A. Prognosis of patients with complete heart block or arrhythmic syncope who were not treated with artificial pacemakers. A long-term follow-up study of 101 patients. Acta Med Scand. 1976;200(6):457-463.
Epstein AE, Dimarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. Heart Rhythm. 2008;5(6):e1-e62.
Lamas GA, Muller JE, Turi ZG, et al. A simplified method to predict occurrence of complete heart block during acute myocardial infarction. Am J Cardiol. 1986;57(15):1213-1219.
Menozzi C, Brignole M, Alboni P, et al. The natural course of untreated sick sinus syndrome and identification of the variables predictive of unfavorable outcome. Am J Cardiol. 1998;82(10):1205-1209.
Moss AJ, Hall WJ, Cannom DS, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events (MADIT-CRT). N Engl J Med. 2009;361:1-10.
Ryan TJ, Antman EM, Brooks NH, et al. 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction: Executive summary and recommendations: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation. 1999;100(9):1016-1030.
Scheinman MM, Peters RW, Suave MJ, et al. Value of the H-Q interval in patients with bundle branch block and the role of prophylactic permanent pacing. Am J Cardiol. 1982;50(6):1316-1322.
Vardas PE, Auricchio A, Blanc JJ, et al. Guidelines for cardiac pacing and cardiac resynchronization therapy: The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007;28(18):2256-2295.
Zeltser D, Justo D, Halkin A, et al. Drug-induced atrioventricular block: Prognosis after discontinuation of the culprit drug. J Am Coll Cardiol. 2004;44(1):105-108.
1 Epstein AE, Dimarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. Heart Rhythm. 2008;5(6):e1-e62.
2 Vardas PE, Auricchio A, Blanc JJ, et al. Guidelines for cardiac pacing and cardiac resynchronization therapy: The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007;28(18):2256-2295.
3 Menozzi C, Brignole M, Alboni P, et al. The natural course of untreated sick sinus syndrome and identification of the variables predictive of unfavorable outcome. Am J Cardiol. 1998;82(10):1205-1209.
4 Katritsis D, Camm AJ. Chronotropic incompetence: A proposal for definition and diagnosis. Br Heart J. 1993;70(5):400-402.
5 Dhingra RC, Denes P, Wu D, et al. The significance of second degree atrioventricular block and bundle branch block. Observations regarding site and type of block. Circulation. 1974;49(4):638-646.
6 Cheng S, Keyes MJ, Larson MG, et al. Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. JAMA. 2009;301(24):2571-2577.
7 Kim YH, O’Nunain S, Trouton T, et al. Pseudo-pacemaker syndrome following inadvertent fast pathway ablation for atrioventricular nodal reentrant tachycardia. J Cardiovasc Electrophysiol. 1993;4(2):178-182.
8 Brecker SJ, Xiao HB, Sparrow J, Gibson DG. Effects of dual-chamber pacing with short atrioventricular delay in dilated cardiomyopathy. Lancet. 1992;340(8831):1308-1312.
9 Talan DA, Bauernfeind RA, Ashley WW, et al. Twenty-four hour continuous ECG recordings in long-distance runners. Chest. 1982;82(1):19-24.
10 Edhag O, Swahn A. Prognosis of patients with complete heart block or arrhythmic syncope who were not treated with artificial pacemakers. A long-term follow-up study of 101 patients. Acta Med Scand. 1976;200(6):457-463.
11 Rotman M, Triebwasser JH. A clinical and follow-up study of right and left bundle branch block. Circulation. 1975;51(3):477-484.
12 Scheinman MM, Peters RW, Suave MJ, et al. Value of the H-Q interval in patients with bundle branch block and the role of prophylactic permanent pacing. Am J Cardiol. 1982;50(6):1316-1322.
13 Fisch GR, Zipes DP, Fisch C. Bundle branch block and sudden death. Prog Cardiovasc Dis. 1980;23(3):187-224.
14 Connolly SJ, Sheldon R, Thorpe KE, et al. Pacemaker therapy for prevention of syncope in patients with recurrent severe vasovagal syncope: Second Vasovagal Pacemaker Study (VPS II): A randomized trial. JAMA. 2003;289(17):2224-2229.
15 Zeltser D, Justo D, Halkin A, et al. Drug-induced atrioventricular block: Prognosis after discontinuation of the culprit drug. J Am Coll Cardiol. 2004;44(1):105-108.
16 Huynh H, Dalloul G, Ghanbari H, et al. Permanent pacemaker implantation following aortic valve replacement: Current prevalence and clinical predictors. Pacing Clin Electrophysiol. 2009;32(12):1520-1525.
17 Meimoun P, Zeghdi R, D’Attelis N, et al. Frequency, predictors, and consequences of atrioventricular block after mitral valve repair. Am J Cardiol. 2002;89(9):1062-1066.
18 Chung MK. Cardiac surgery: Postoperative arrhythmias. Crit Care Med. 2004;28(10 Suppl):N136-144.
19 Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350(21):2140-2150.
20 Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352(15):1539-1549.
21 Lindenfeld J, Feldman AM, Saxon L, et al. Effects of cardiac resynchronization therapy with or without a defibrillator on survival and hospitalizations in patients with New York Heart Association class IV heart failure. Circulation. 2007;115(2):204-212.
22 Moss AJ, Hall WJ, Cannom DS, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events (MADIT-CRT). N Engl J Med. 2009;361:1-10.
23 D’Allonnes GR, Pavin D, Leclercq C, et al. Long-term effects of biatrial synchronous pacing to prevent drug-refractory atrial tachyarrhythmia: A nine-year experience. J Cardiovasc Electrophysiol. 2000;11(10):1081-1091.
24 Erwin JPIII, Nishimura RA, Lloyd MA, Tajik AJ. Dual chamber pacing for patients with hypertrophic obstructive cardiomyopathy: A clinical perspective in 2000. Mayo Clin Proc. 2000;75(2):173-180.
25 Nishimura RA, Trusty JM, Hayes DL, et al. Dual-chamber pacing for hypertrophic cardiomyopathy: A randomized, double-blind, crossover trial. J Am Coll Cardiol. 1997;29(2):435-441.
26 Scott CD, Dark JH, McComb JM. Sinus node function after cardiac transplantation. J Am Coll Cardiol. 1994;24(5):1334-1341.
27 Heinz G, Hirschl M, Buxbaum P, et al. Sinus node dysfunction after orthotopic cardiac transplantation: Postoperative incidence and long-term implications. Pacing Clin Electrophysiol. 1992;15(5):731-737.
28 Klein LS, Miles WM, Heger JJ, Zipes DP. Transcutaneous pacing: Patient tolerance, strength-interval relations and feasibility for programmed electrical stimulation. Am J Cardiol. 1988;62(16):1126-1129.
29 Zoll PM, Zoll RH, Falk RH, et al. External noninvasive temporary cardiac pacing: Clinical trials. Circulation. 1985;71(5):937-944.
30 Elmi F, Tullo NG, Khalighi K. Natural history and predictors of temporary epicardial pacemaker wire function in patients after open heart surgery. Cardiology. 2002;98(4):175-180.
31 Ryan TJ, Antman EM, Brooks NH, et al. 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction: Executive summary and recommendations: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation. 1999;100(9):1016-1030.
32 Lamas GA, Muller JE, Turi ZG, et al. A simplified method to predict occurrence of complete heart block during acute myocardial infarction. Am J Cardiol. 1986;57(15):1213-1219.