CHAPTER 22 Current Concepts in Fractures of the Distal Humerus
INTRODUCTION
Recovery of painless and satisfactory elbow function after a fracture of the distal humerus requires anatomic reconstruction of the articular surface, restitution of the overall geometry of the distal humerus and stable fixation of the fracture fragments to allow early and full rehabilitation.2,4,5,7–9,14 Although these goals are obvious, the orthopedic community would agree that they may be technically difficult to achieve, especially in the presence of substantial osteoporosis or comminution.14
The techniques proposed by the AO/ASIF group had been standard for fixation of distal humerus fractures in the past.8,14 Their recommended technique included fixation of the articular fragments with screws and column stabilization with two plates at a 90-degree angle to one another.3,8,19 Fracture stability is only as secure as the fixation of the distal fragment to the shaft. Using standard AO/ASIF techniques, different authors have reported unsatisfactory results in 20% to 25% of patients.2,4,5,7–9
Improvements in the treatment of these fractures recently have been predicated on understanding and overcoming the limitations and reasons for failure of previous techniques. When treatment of severe distal humerus fractures fails, it typically is due to either nonunion at the supracondylar level or stiffness resulting from prolonged immobilization that has been used in an attempt to avoid failure of inadequate fixation.14 Either way, the limiting factor is fixation of the distal fragments to the shaft. In an effort to increase the yield of excellent and satisfactory results obtained after fixation of distal humerus fractures and to reproducibly obtain stable fixation in the presence of osteoporosis or comminution, I recommend (and have used for two decades) an alternative philosophy and technique based on principles that maximize fixation in the distal fragments and compression at the supracondylar level.11–13,15,17 The key to the stability achieved with this fixation construct is that it combines the features and stability of an arch while locking the two columns of the distal humerus together. The stability achieved allows routine commencement of an intensive rehabilitation program postoperatively, including full active motion with no external protection.
PRINCIPLE-BASED FIXATION
PRINCIPLES AND TECHNICAL OBJECTIVES
Before discussing the details of surgical techniques, it is imperative that the treating surgeon understand the principles (Box 22-1) and technical objectives (Box 22-2) that, if followed and achieved respectively, will maximize the likelihood of a successful outcome from treatment of these fractures.






EXPOSURE
The operation is performed with the patient in the supine position. A sterile tourniquet is inflated only for dissection of the ulnar nerve, which is transposed anteriorly. The triceps-anconeus reflecting pedicle (TRAP) approach provides adequate exposure for a surgeon experienced with the technique.10 This technique involves combining the Bryan-Morrey and modified Kocher approaches to reflect the triceps in continuity with the anconeus. However, I believe that an olecranon osteotomy provides even greater exposure and is recommended in the setting of intra-articular comminution. The TRAP approach is indicated if total elbow replacement is necessary.
PRINCIPLE-BASED SURGICAL TECHNIQUE
The surgical technique is performed in five steps:
Stability and function are restored by achieving eight technical objectives (see Box 22-2) derived from the principles of (1) maximizing fixation in the distal fragments, and (2) ensuring that all fixation in the distal segment contributes to stability at the supracondylar level (see Box 22-1) (Fig. 22-1).
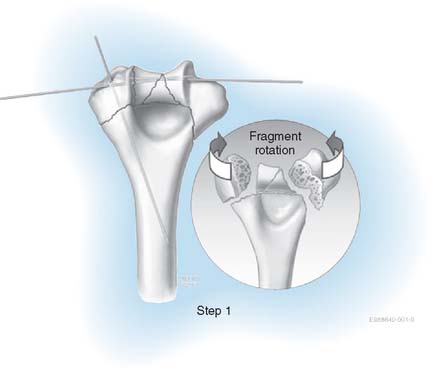
STEP 1. ARTICULAR SURFACE REDUCTION
Once the fracture is exposed, the first step is reassembly of the articular surface. The proximal ulna and radial head can be used as a template for the reconstruction of the distal humerus. The articular fragments are provisionally fixed with smooth Kirschner wires (K wires) (Fig. 22-2). In cases with extensive comminution, fine threaded wires (1 to 1.5 mm) are used, then cut off and left in as definitive adjunctive fixation. K wires permit assembly of the joint surface fragments in a manner that is analogous to the use of dowels in furniture making. It is necessary that these wires be placed close to the subchondral level so as not to interfere with the passage of screws from the plates into the distal fragments; specifically, no screws are placed in the distal fragments until the plates are applied. The articular fragments are fixed in the following order:
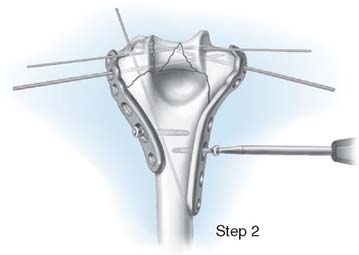
STEP 2. PLATE APPLICATION AND PROVISIONAL FIXATION
We routinely use precontoured medial and lateral plates from the Mayo Congruent Elbow Plate System (Acumed, Hillsboro, OR) (Fig. 22-3). The medial plate can be extended to the articular margin in very distal or comminuted fractures and is contoured to the shape of the medial epicondyle. The ulnar nerve must be transposed if this extended plate is used. The distal end placed more posteriorly to prevent impinging on, or cutting into, the common extensor tendon and lateral collateral ligament complex. Both plates should be slightly undercontoured to provide additional compression at the metaphyseal region when applied. The length of the plates is selected so that at least three screws are placed both medially and laterally proximal to the metaphyseal component of the fracture. These plates are designed so that in any combination they will end at different levels to avoid the creation of a stress riser proximally. The plates are then provisionally applied according to the following steps:
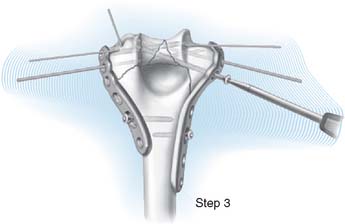
STEP 3. DISTAL FIXATION
Once the plates are provisionally applied, medial and lateral screws are introduced distally to provide stable fixation of the intraarticular fragments and rigid anchorage to the plates (Fig. 22-4).
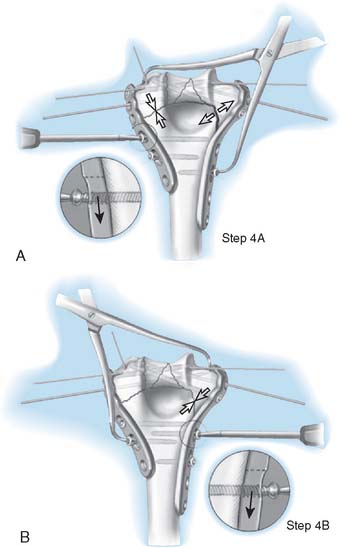
STEP 4. SUPRACONDYLAR COMPRESSION
The plates are then fixed proximally under maximum compression at the supracondylar level (Fig. 22-5A and B).
STEP 5. FINAL FIXATION
The smooth Steinmann pins are removed, and then the remainder of the screws are inserted (Fig. 22-6). The intraoperative elbow motion should be full unless significant swelling has already developed. One deep and one subcutaneous drain are placed during the closure. The skin should be closed with staples or interrupted sutures.
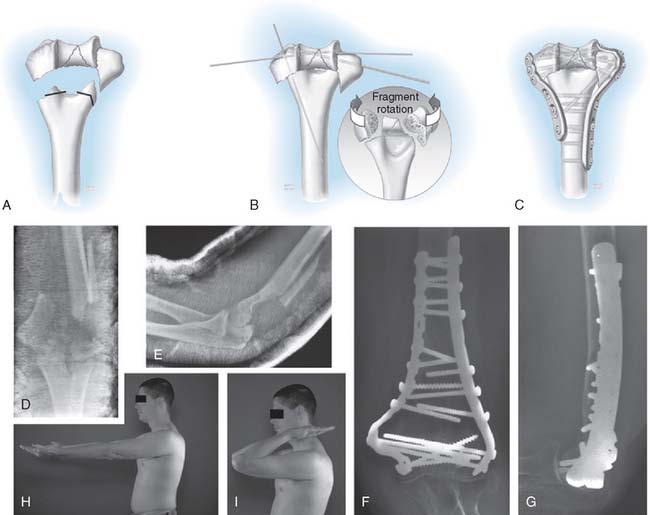
DEALING WITH METAPHYSEAL BONE LOSS
Adequate bony contact with interfragmentary compression in the supracondylar region is necessary to ensure the stability of the construct and eventual fracture union. If metaphyseal bone loss or comminution precludes an anatomic reconstruction with satisfactory bony contact, the humerus can be shortened at the metadiaphyseal fracture site, provided that the overall alignment and geometry of the distal humerus is correct. We refer to this alternative reconstructive technique as supracondylar shortening (Fig. 22-7A to G). This technique is especially useful in cases of combined soft tissue and bone loss. Shortening by 1 cm or less has only a slight effect on triceps strength in terminal extension,6 and in cases of severe soft tissue and bone loss, up to 2 cm of shortening can be tolerated without serious disturbance of elbow biomechanics.6
POSTOPERATIVE MANAGEMENT
STRUCTURAL STABILITY VERSUS FRACTURE STABILITY
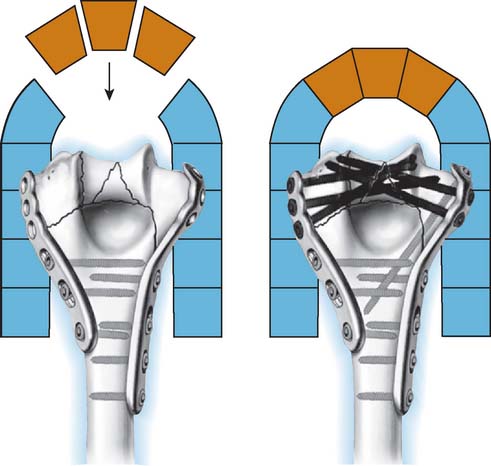
I wish to emphasize that this principle-based technique is not just a different method of fracture fixation. It is a whole new concept based on the idea that stability of the distal humerus is achieved by the creation of an architectural structure. The bone fragments rely on their integration with the whole structure for stability, rather than on fixation of each bone fragment by screw threads. The concept is borrowed from modern architecture and the application of civil engineering principles to surgery. The interdigitation of screws within the distal segment rigidly attaches the articular fragments to the shaft by linking the two columns together. This permits stability to be achieved in such cases as low transcondylar (Fig. 22-8A to D) or severely comminuted (Fig. 22-9A to D) fractures.
The concept follows the architectural principles of an arch, in which two columns are anchored at their base (on the shaft of the humerus) and linked together at the top (long screws from the plates on each side interdigitating within the articular segment). The interdigitation is best achieved by contact between the screws. However, multiple screws separated by small gaps within the bone will function as a “rebar” construct (steel rods inside concrete). Fixation of the bone fragments is thus reliant not on screw purchase in the bone, but on the stability of the hardware framework, in just the same way that a modern building derives its stability from the grid work of steel assembled and bolted or welded together inside its walls and columns.
The screws in the distal segment are converted into fixed angle screws by two of the technical objectives. First, several long screws in the distal fragments lock together by interdigitation. Second, these screws pass through a plate on one side and into a bone fragment on the other side that itself is also anchored by a plate. From an engineering perspective, this technique of creating fixed angle screws enhances fixation in the distal fragments. It also permits rigid linkage and compression between the distal segment and the shaft. The combined use of clamps, strong and slightly undercontoured plates, dynamic compression holes, and selected metaphyseal shortening provides interfragmentary compression at the supracondylar level. The stability of the construct is such that a rehabilitation program can be commenced in the immediate postoperative period without fear of hardware failure.
Role of Locking Screws
Although fixed angle locking plates are available, I prefer to use variable angle locking screws (TAPLOC Acumed, Hillsboro, OR) for the distal segment to prevent the problem of incorrect screw positioning due to the fixed angles predetermined other plate designs. With the use of locking screws, fewer screws are thought necessary. However, based on my experience, and that of colleagues, I do not believe that locking screws are necessary if the principles and technical objectives for structural stability are achieved.
POTENTIAL COMPLICATIONS
The main complications that have been reported after internal fixation of distal humerus fractures are residual decreased range of motion, fixation failure with nonunion or malunion, nerve dysfunction, extensor mechanism dysfunction, post-traumatic degenerative changes, wound and skin problems, and avascular necrosis.1,2,4,5,7–9,20 The combination of ischemic skin and a subcutaneous hematoma is an indication for surgical lavage and reclosure of the wound.
PITFALLS AND TIPS
Excessive contouring of the distal end of the lateral plate can cause entrapment of the common extensor origin or lateral collateral ligament complex. This can result in loss of motion and even necrosis of the underlying soft tissues. This is avoided by placing the plate such that it stops at the epicondyle rather than distal to it and by ensuring that the plate does not wrap around the epicondyle and compress the soft tissues. This will give the appearance on the postoperative radiograph of the tip of the plate sitting away from the bone, but this space is required to accommodate the soft tissues under the plate.
The single biggest impediment to successful application of this principle-based technique is the misconception that plates must be applied in two perpendicular planes. Although that used to be true when very weak 3.5 one-third tubular plates were used, it most certainly is not true when strong plates are used. The “parallel” double-plate construct has been shown to provide excellent stability even in the presence of supracondylar gaps.18 In fact, Schemitsch et al.18 showed that the combination of a medial reconstruction and lateral DuPont plate in parallel planes was stronger than two reconstruction plates placed in two planes 90 degrees to each other, as is recommended by the AO/ASIF group and currently employed by most surgeons. When failure occurs, it is likely to start in the lateral column. With only one to three short screws into the capitellum, it can pull away from a posteriorly placed plate (Fig. 22-10A to C). We strongly recommend the use of this technique for comminuted distal humerus fractures, and prefer its use routinely for less complex fractures as well, because the stability is such that intensive rehabilitation is possible. However, for noncomminuted fractures in good quality bone, either technique can be used reliably.
The efficacy of this approach to achieving structural stability was conclusively documented in a series of 32 consecutive complex distal humeral fractures.16 Twenty-six fractures were AO type C3, and 14 were open. Despite extensive comminution, bone loss, osteoporosis, or open wounds, neither hardware failure nor fracture displacement occurred in any patient. Union of 31 of the 32 fractures was achieved primarily. No patients required surgery to treat elbow stiffness unless heterotopic ossification had formed. There was one deep infection that resolved without hardware removal and did not impede union. At the time of the most recent follow-up, 28 elbows were either not painful or only mildly painful, and the mean flexion-extension arc was 99 degrees.
1 Ackerman G., Jupiter J.B. Non-union of fractures of the distal end of the humerus. J. Bone Joint Surg. 1988;70-A:75.
2 Gabel G.T., Hanson G., Bennett J.B., Noble P.C., Tullos H.S. Intraarticular fractures of the distal humerus in the adult. Clin. Orthop. Rel. Res. 1987;216:99.
3 Helfet D.L., Hotchkiss R.N. Internal fixation of the distal humerus: A biomechanical comparison of methods. J. Orthop. Trauma. 1990;4:260.
4 Henley M.B., Bone L.B., Parker B. Operative management of intra-articular fractures of the distal humerus. J. Orthop. Trauma. 1987;1:24.
5 Holdsworth B.J., Mossad M.M. Fractures of the adult distal humerus. J. Bone Joint Surg. 1990;72-B:362.
6 Hughes R.E., Schneeberger A.G., An K.N., Morrey B.F., O’Driscoll S.W. Reduction of triceps muscle force after shortening of the distal humerus: a computational model. J. Shoulder Elbow Surg. 1997;6:444.
7 John H., Rosso R., Neff U., Bodoky A., Regazzoni P., Harder F. Operative treatment of distal humeral fractures in the elderly. J. Bone Joint Surg. 1994;76-B:793.
8 Jupiter J.B., Neff U., Holzach P., Allgower M. Intercondylar fractures of the humerus. J. Bone Joint Surg. 1985;67-A:226.
9 Letsch R., Schmit-Neuerburg K.P., Sturmer K.M., Walz M. Intraarticular fractures of the distal humerus. Surgical treatment and results. Clin. Orthop. Rel. Res. 1989;241:238.
10 O’Driscoll S. The triceps-reflecting anconeus pedicle (TRAP) approach for distal humeral fractures and nonunions. Orthop. Clin. North Am. 2000;31:91.
11 O’Driscoll S.W. Optimizing stability in distal humeral fracture fixation. J. Shoulder Elbow Surg. 2005;14(1 Suppl S):186S.
13 O’Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: pearls and pitfalls. Instr. Course Lect. 2003;52:113.
12 O’Driscoll S.W., Sanchez-Sotelo J., Torchia M.E. Management of the smashed distal humerus. Orthop. Clin. North Am. 2002;33:19.
14 Ring D., Jupiter J.B. Fractures of the distal humerus. Orthop. Clin. North Am. 2000;31:103.
15 Sanchez-Sotelo J., Torchia M., O’Driscoll S.W. Principle-based internal fixation of distal humerus fractures. Tech. Hand Up. Extrem. Surg. 2001;5:179.
16 Sanchez-Sotelo J., Torchia M.E., O’Driscoll S.W. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. J. Bone Joint Surg. Am. 2007;89:961.
17 Sanchez-Sotelo J., Torchia M.E., O’Driscoll S.W. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. J. Bone Joint Surg. Am. 2008;90(Suppl 2):31.
18 Schemitsch E.H., Tencer A.F., Henley M.B. Biomechanical evaluation of methods of internal fixation of the distal humerus. J. Orthop. Trauma. 1994;8:468-475.
19 Self J., Viegas S.F., Buford W.L., Patterson R.M. A comparison of double-plate fixation methods for complex distal humerus fractures. J. Shoulder Elbow Surg. 1995;4:11.
20 Sodergard J., Sandelin J., Bostman O. Postoperative complications of distal humeral fractures. 27/96 adults followed up for 6 (2-10) years. Acta Orthop. Scand. 1992;63:85.