CHAPTER 339 Craniofacial Injuries
Epidemiology
The causes of craniofacial trauma reflect the general pattern of neurotrauma but with significant regional variations. Worldwide, modes of transportation are the main cause of neurotrauma and craniofacial trauma. In high-income countries, an overall fall in transport injuries, the use of air bags in motor vehicles, and the use of helmets by motorcyclists have reduced the incidence of maxillofacial injury. Falls in infancy and old age and pedestrian and bicycle accidents have become major causes in some countries.1 There remains a high incidence in motorbike riders, particularly adolescents. Facial fractures are more common with open face helmets, and the most severe injuries occur in riders with no helmet.2 Furthermore, with the development of efficient retrieval systems, more patients with severe injuries survive to reach trauma centers. In developing countries, the continuing rise in the incidence of transport-related neurotrauma3 and the corresponding rise in severe head injuries are accompanied by a parallel increase in craniofacial injury, although these figures are not well documented.
Other causes of craniofacial trauma include falls, assaults,4,5 sporting injuries, industrial accidents, and missile injuries.1,2,6,7
Severe craniofacial fractures, typified by panfacial fracture involving all regions of the face, are most often associated with motor vehicle accidents. In this group, major injuries to other systems are common.8
In organizing multidisciplinary care and planning preventive strategies, an understanding of the causes and incidences in a particular community is essential.4,5,9
Functional Anatomy
The Anterior Cranium
Posteriorly, the ethmoid bone attaches to the body of the sphenoid, which is the roof of the sphenoid sinuses. Laterally, the lesser wings of the sphenoid form the crescentic posterior borders of the anterior fossa. The optic canal is formed by the two roots of the lesser wing of the sphenoid and runs forward and laterally in the superolateral wall of the sphenoid sinus to the orbital apex.10
The Facial Skeleton
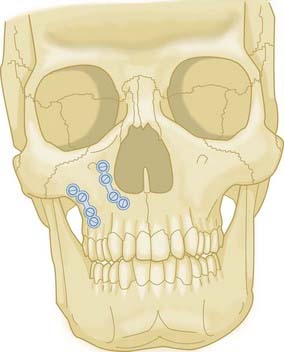
The midfacial skeleton is designed to transmit the powerful forces of mastication to the base of the skull. The strong horizontal elements in the maxillae, the alveoli, and the hard palate make up a foundation to support three paired vertical buttresses. The load path for the distribution of force consists of the two buttresses on the piriform margin, from the region of the lateral incisor to the medial orbital margin, and two buttresses from the region of the molar tooth to the body of the zygoma on each side. It is these buttresses that provide the ideal places for stabilization, particularly with plates and screws (see Fig. 339-11).11
Pathophysiology
The Cranial Cavity
The dura of the anterior fossa floor is firmly adherent to the cribriform plate, where it is penetrated by filaments of the olfactory nerves accompanied by sheaths of arachnoid. Fractures of the anterior fossa floor may lacerate the dura. A dural arachnoid tear with a fracture that communicates with the nose or paranasal sinuses will lead to a cerebrospinal fluid (CSF) fistula12 (see Chapter 341).
Optic Nerve
Traumatic injury to the optic nerve is indicated by a dilated, sometimes irregular pupil with hippus; the pupil does not show a direct or consensual light reaction but does react to contralateral light. With a partial injury, some light reactions may be seen.13 Flash evoked potentials may help diagnose early injury in unconscious patients and children.14
The optic nerve may be compressed by a displaced fracture through the optic canal, by contusion or hematoma within the canal without a fracture, or by direct injury to the orbit.15,16
The Globe and Orbit
The globe can be injured by direct penetration or by blunt force. The globe is robust and cushioned by the surrounding soft tissue and will resist a blunt force sufficient to cause a blow-out fracture of the floor or medial wall.17 Nonetheless, the incidence of ocular injury with an orbital fracture is about 20%.18 Blunt injuries to the globe include corneal abrasions, hyphema, vitreous hemorrhage, and retinal detachment.
Mechanisms of Injury
Penetrating and Missile Wounds
Gunshot wounds may be penetrating, perforating, or ablative, depending on the velocity and nature of the projectile. A low-velocity missile typically causes a penetrating injury. The missile remains embedded in the tissue and will cause little damage unless it strikes a vital structure. The facial bones are fractured and the skin lacerated without tissue loss. Most civilian gunshot wounds are of low to medium velocity, and the tissue damage is restricted to the path of the projectile. Penetrating brain injuries carry high mortality, nearly 70% in a recent report.19
Initial Management
There may be profuse bleeding, hypovolemic shock, and hypotension. They are often associated with injuries elsewhere in the body. Consequently, less severe craniofacial injuries may be overlooked in the urgency to manage severe injuries elsewhere in the body.21
Specific Acute Problems with Craniofacial Injuries
Breathing
Securing the Airway
The airway may be secured in the following ways:
Clinical Assessment
Neurological
Facial nerve function can be assessed by observation and by the response to painful stimuli.
Investigations
Later Imaging
Standard Radiographic Projections
Computed Tomography
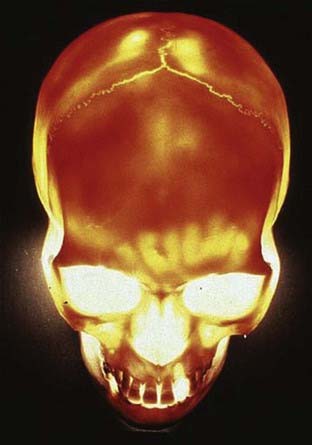
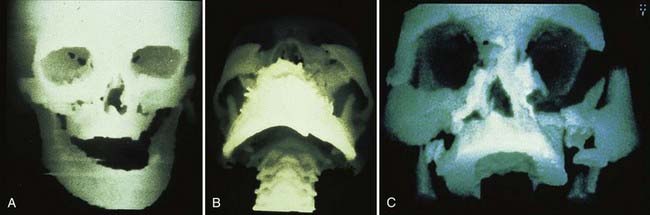
Three-Dimensional Computed Tomography Reconstructions
The acquired CT slices, usually axial, can be used to produce three-dimensional representations of the skeleton, soft tissue, or both. These representations can be viewed from any direction and greatly facilitate an understanding of the anatomy of facial fractures.23–26 These data can also be used to produce solid nylon models for planning surgical reconstruction and as a template on which a prosthesis can be manufactured.
Management
Brain Injury
Craniocerebral injuries may be classified into five main clinical groups:
Orbital Injury
Optic Nerve Injury
Management of traumatic optic nerve injury remains controversial, and the debate whether observation alone is better than steroids, surgical decompression, or a combination of the two remains unresolved.29–36 A regimen of megadose methylprednisolone (loading dose of up to 30 mg/kg; maintenance dose of up to 5 mg/kg per hour for 72 hours) followed by a gradual reduction has been recommended37; however, the International Optic Nerve Trauma Study found no benefit from either corticosteroid therapy or optic nerve decompression.32 A Cochrane review published in 2005 noted a high rate of spontaneous recovery and concluded that traumatic optic nerve injury initially seen more than 8 hours after injury should not be treated with steroids; for those seen within 8 hours, the evidence of benefit was weak.38 Several papers have reported some good results after endoscopic decompression.33,39,40 A small study reported better results in those operated early30; however, a further Cochrane review in 2007 was unable to find sufficient evidence from the small retrospective series available and noted the risk for complications.41
Definitive Repair
In deciding on the appropriateness of early versus delayed surgery,42–44 the following principles need to be observed:
Priorities and Staging of Procedures
Timing of Repair
Some advocate very early definitive surgery, within 24 to 48 hours as a general rule, under the rationale that reconstruction should be undertaken before contractile scar tissue prevents correct positioning of soft tissues, particularly those within the orbit.45 In our experience, repair of facial fractures is rarely urgent and can be carried out in one or more elective procedures 7 to 10 days after the injury or longer, depending on the state of the patient, without compromising the result. This allows time for clinical stabilization of the patient and preparation of a multidisciplinary treatment plan, which may involve ophthalmology, dentistry, and ear, nose, and throat specialists, as well as neurosurgical and craniofacial specialists.
Surgical Principles
There are three important anatomic sites of injury to the craniofacial interface.
Craniofacial Exposures
Surgical treatment is typically based on wide exposure of the craniofacial skeleton via a bicoronal scalp flap or periorbital, intraoral, and extraoral incisions. Recently, endoscopy has been used for some orbital fractures, for fractures of the mandibular condyles, and for repair of anterior cranial base fractures with CSF rhinorrhea (see Chapter 341).
The Bicoronal Scalp Flap
This flap is placed behind the patient’s hairline when possible. The incision may be a straight line from ear to ear, as is usual in neurosurgery, or a wavy or zigzag line, which gives a better cosmetic result (Fig. 339-3). The flap is raised in a subgaleal plane to 2 to 4 cm above the supraorbital rim or the site of any fractures of the frontal bone. From this level the dissection proceeds subpericranially over the orbital rim and into the orbit. The supraorbital neurovascular bundle is carefully preserved, if necessary by fracturing the margins of the supraorbital notch with a fine osteotome.
Subciliary lower eyelid incisions or transconjunctival incisions with or without a lateral canthotomy provide excellent exposure of the orbital floor.46
Bone Grafting
After severe injuries bone is often missing from one or more of the vertical bony pillars of the midface.43 The thin bone of the floor and medial wall of the orbit may be lost with orbital fractures.
Common donor sites for harvesting bone are the iliac crest, rib cage and skull vault (calvaria). Many factors are important for the survival of bone grafts, the most important being rigid fixation followed by good soft tissue coverage, preferably with a periosteal surface.47 Other factors include a well-vascularized bed in the host tissues and prevention of hematoma formation.
Donor Sites
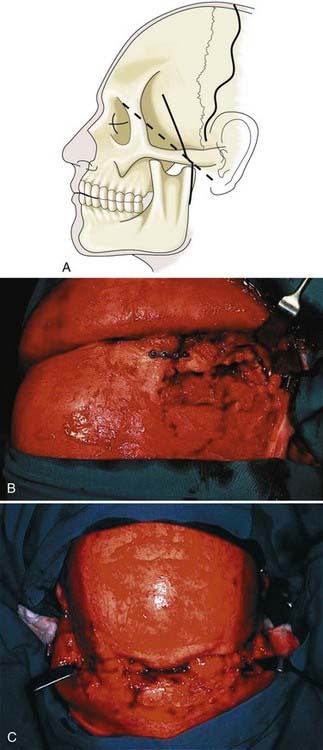
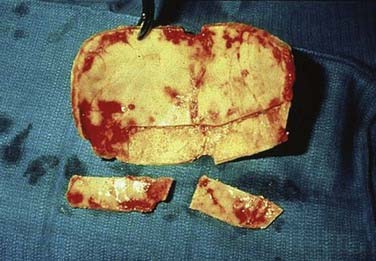
Calvarial Grafts
Calvarial bone has the disadvantage of being more rigid than either iliac bone or rib. The outer table can be safely split from the skull at sites where there is a well-formed diploic space (Fig. 339-4), as is usual in the parietal area; however, radiographs must be examined to determine whether the skull is thick enough to perform the maneuver safely. The sagittal sinus and its parasagittal venous tributaries must be avoided, and great care should be taken to avoid penetrating the dura mater. When a small square of bone is needed, as for the orbital floor, the pericranium can be left attached to prevent fragmentation of the graft. Contour defects are hard to avoid when the outer table is harvested. The inner table can be harvested when a craniotomy is being performed and the calvaria is thick enough.
Specific Fracture Patterns
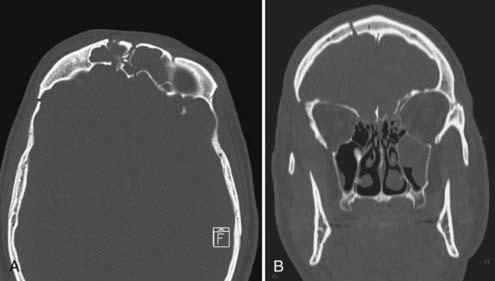
Fractures Involving the Frontal Sinus
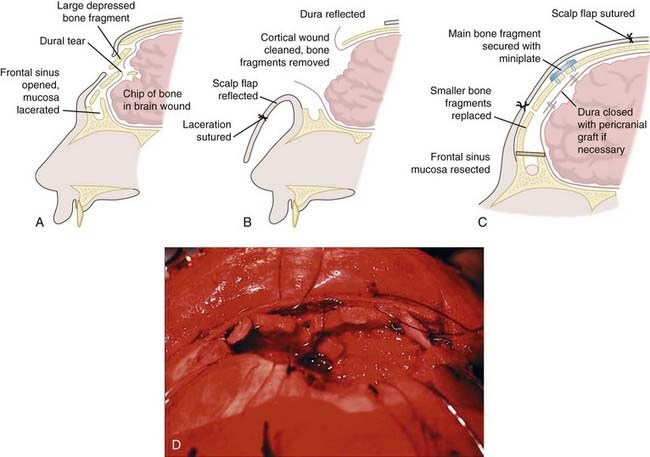
A compound depressed fracture of the frontal sinus involving the anterior and posterior walls is best approached through a bicoronal scalp flap (Figs. 339-5 and 339-6). A small frontal craniotomy is made above the sinus area to expose the posterior wall of the sinus, and the depressed fracture is approached extradurally. If the dura is torn, the posterior wall of the frontal sinus is drilled away and the sinus mucosa stripped. The dura is repaired in a watertight manner by primary suture or by patching with a graft of temporal fascia or pericranium placed intradurally if possible. The sinus ostia can be plugged with muscle. A pericranial graft attached inferiorly is turned forward and sutured to the dura to seal the frontal sinus. If soft tissue injuries prevent such grafting, a free graft of temporal fascia can be laid over the exposed frontal sinus and sutured to the dura and to the pericranium. The technique is designed to obliterate the sinus. The anterior wall of the frontal sinus is preserved. If it is comminuted, the fragments are wired or plated in good position.48
A simple posterior wall fracture without a dural fistula need not be treated.
Naso-orbito-ethmoid Fractures
These fractures may be unilateral or bilateral, simple or comminuted, closed or compound. They may occur in isolation or in association with more extensive fracturing of the forehead, orbit, or maxilla.49
Fractures of the Zygoma
The zygomatic bone forms part of the lateral wall and floor of the orbit and makes an essential contribution to orbital contour and facial width and projection.52
Detailed ophthalmologic examination is essential.
Treatment
An undisplaced zygomatic fracture requires no operative intervention.
An isolated, displaced zygomatic arch fracture is usually treated by closed reduction.53
Comminuted and grossly displaced orbitozygomatic fractures are almost always caused by high-velocity impacts and are associated with major midface or panfacial fractures. Gruss and colleagues advised first restoring the anterior projection of the zygomatic arch because this is key to restoring facial projection.52 The zygomatic arch is the significant reference point with respect to midfacial width and anteroposterior projection in panfacial fractures. CT will indicate the possibility of loss of bone in the orbital floor. In severe fractures, the medial orbital wall can be damaged as well, and bone grafting may be necessary in both these sites to restore orbital volume. The orbital wall components of zygomatic fractures do not require exploration if CT shows no displacement.
Orbital Injury
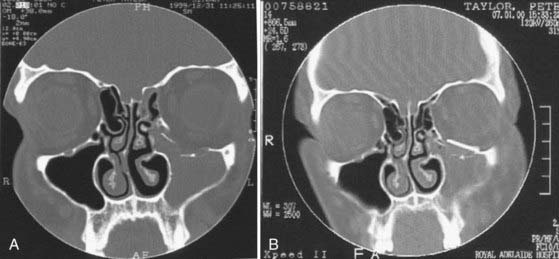
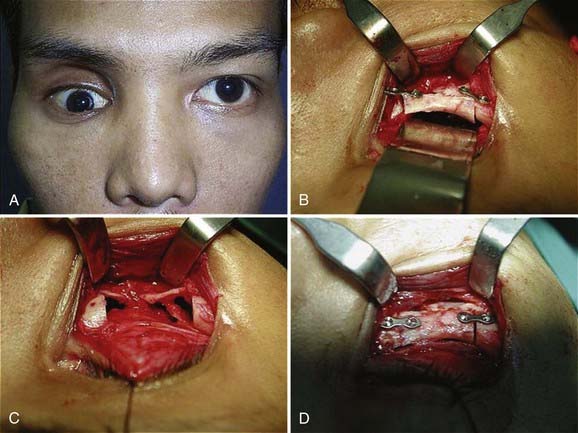
The floor is approached through a transconjunctival incision or subciliary lower eyelid incision (Figs. 339-7 and 339-8).
The most common complication is enophthalmos, which is often due to inadequate exposure of the full extent of the bony defect, particularly a medial orbital wall fracture. Ocular and canthal dystopia results from inaccurate reduction of the zygoma and failure to maintain the bony attachments of the medial canthus and restore the lateral canthal region.54 There may be damage to the globe or impaired motility from scarring or tethering.
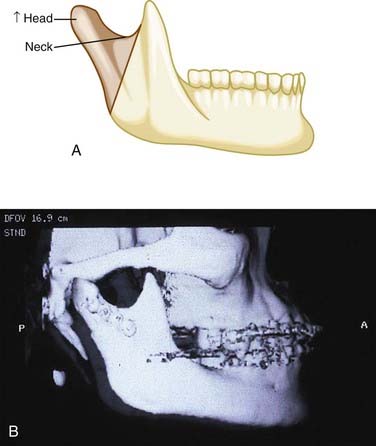
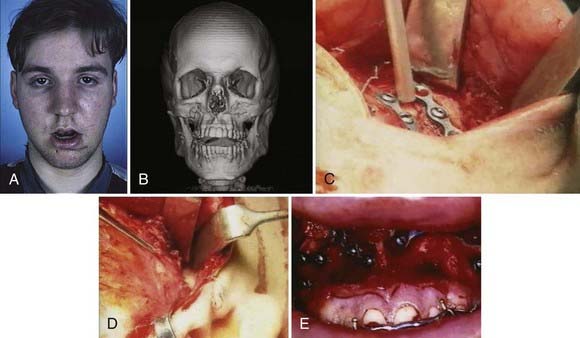
Fractures of the Mandible
Fractures of the mandible are relevant to craniofacial surgery as an important component of panfacial fractures. Correct realignment of the mandible is mandatory for rebuilding the maxilla and the orbits to restore correct facial proportions (Fig. 339-9).
Stable fractures without displacement are best treated conservatively.
Maxillary Fracture Patterns
Maxillary fractures are still most often classified according to the original description by Le Fort (Fig. 339-10), although fractures rarely conform to this pattern and more detailed and accurate descriptions are now based on CT scanning.55
Management
Conservative management is undertaken in the following two situations:
Displaced upper jaw fractures require open reduction and internal fixation.43
Different sequences must be considered when the bones of the upper midface are also fractured and when there is a simultaneous mandibular fracture.57
When the upper jaw fracture is associated with displaced orbital fractures, particularly the zygomatic or naso-orbital component, these are first stabilized. The occlusal complex, which consists of the upper and lower jaws united, is then brought up to the stabilized upper midface, and the final fixation, with or without bone grafting, is carried out along the lines of the buttresses (Fig. 339-11).
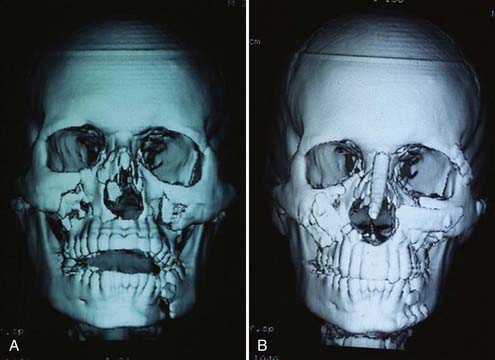
Multiple and Panfacial Fractures
Severe impact to the central part of the face may damage all regions to varying degrees (Fig. 339-12). Because the fracture patterns are extremely variable, there is no standard approach to management. Repair requires repositioning existing bone, replacing severely comminuted or lost bone with primary autogenous bone grafts, and replacing or expanding craniofacial soft tissues to the pretraumatic state.
Gruss and associates grouped these complex injuries into three broad anatomic divisions43:
In most cases there are three key anatomic sites of injury:
Treatment
Sequence of Repair
The sequence of repair depends on the status of the boundaries of the injured face—the calvarial vault above and the mandible below.58
There are other situations in which repair proceeds from below upward. If the mandibular arch is disrupted, especially if it is foreshortened as a result of fracture or fracture-dislocation of the condylar processes, it should be repaired initially to establish a solid basis and posterior facial height. Once the mandible is rigidly restored, the midface can be disimpacted and placed in the predicted occlusion. Intermaxillary fixation is then instituted. Repair subsequently proceeds from above down to meet the already fixed maxillary-mandibular segment. Miniplate fixation or bone grafting is used to reconstitute the four anterior buttresses (Fig. 339-13).
Sagittal Fractures of the Midface
Vertical fractures through the alveolar process and palate occur in 24% of Le Fort fractures, and 78% are associated with mandibular fractures.59 They require careful presurgical dental modeling, sequential repair as outlined, and on occasion, open fixation of the hard palate fracture.
Infancy and Childhood
The skeleton and dentition in children are evolving entities. Development of the skeleton and soft tissues is interrelated and dependent on the functional status of the matrix on which the tissues are growing. Both trauma and surgical intervention can interfere with the growth processes in ways that may not be apparent until years later.60,61
The most common causes of injury are falls in play or sports.4,61
Pediatric injuries in motor vehicle accidents often result from severe impact, and associated injuries have been reported in more than 60% of children.60,63
The facial skeleton at birth contains relatively more cancellous bone and cartilage than the adult facial skeleton. It contains all the unerupted teeth and has not yet been weakened by development of the paranasal sinuses. This accounts for the resilience of the infant’s mandible and midfacial complex to impact. Greenstick fractures are more common. Before completion of eruption of the permanent dentition (5 to 12 years), the presence of unerupted teeth predisposes the bones of the midface and mandible to more oblique and sagittal fractures through the developing tooth crypts.64
The most common facial fractures in childhood are nasal and mandibular.65,66 Isolated fractures of the midface are rare. Orbital roof fractures may be overlooked and should be considered if there is evidence of injury about the eye.67,68
By 7 years, orbitocranial growth is very nearly completed. After the age of 12 years, sinus aeration is near completion, adult dentition is established, and mineralization of the skeleton becomes complete. The facial skeleton has changed from a solid resilient mass to a complex system of robust but rigid pillars and thin plates. The fracture patterns therefore become those of the adult.12
General Principles
For fractures with minimal displacement, treatment should be conservative.
Greenstick fractures should be reduced without fixation.
Severely displaced fractures need to be reduced and fixed with minimal exposure.
Teeth should be preserved whenever possible.
Long-term follow-up is essential to detect any growth abnormality and determine the need for later operations such as bone grafting.69
Gunshot Wounds
Management
For low-velocity injuries, the missile tract should be excised and the fractures fixed early.
The maxillofacial region has an excellent blood supply, and the risk for secondary infection and secondary hemorrhage is slight; hence treatment consists of minimal débridement and early closure with reconstruction in the early phase. Gruss and coworkers recommended the following70:
Timing of Repair
With moderate injuries, all necessary surgery may be achieved in one early operation without extra stress on the patient. In those requiring complex surgery, reconstruction of the bony and soft tissues of the face and skull should be undertaken in the first 7 to 21 days after injury.70
Soft Tissue Injury
Tattooed Foreign Matter
Foreign material may be embedded to varying depths in the skin, particularly with abrasions. The tattooed material should be removed as soon as possible by scrubbing with a soft nylon brush. Deeply embedded matter may need to be removed with fine-tipped scissors or a scalpel.71
Puncture Wounds
Puncture wounds can be deceptive, with the depth and direction of penetration not being clear from superficial examination.72 Deeply situated vital structures may be injured. The penetrating object is not usually sterile, and the distal part may break off. The wound should be carefully explored with a blunt instrument. Radiography or CT may show embedded matter. MRI may be necessary to identify wood or glass fragments. Penetration near a major vessel may require angiography.
Wounds near the upper eyelid, especially in children, should be treated with caution because an object such as pencil or chopstick can quite easily penetrate the thin orbital roof,73 yet there may be little or no external signs of penetration. Careful neurological and neuro-ophthalmologic assessment should be undertaken, and if deep penetration is suspected, scanning should be performed to identify the bony defect and the track. Retained wood fragments should be removed because they present a risk of infection. Penetration by metal objects may be treated with antibiotics alone.
Complications
Dural Fistula
Fractures of the midface (Le Fort I and II) and nasoethmoid fractures may lead to cranionasal fistulas through the cribriform plates and frontal, ethmoid, or sphenoid sinuses.74 CSF rhinorrhea should be searched for in all patients who may have an anterior fossa fracture and confirmed by β2-transferrin testing. It has been estimated that 35% of patients with severe facial fractures have a CSF fistula and that 60% will cease within 10 days. This may be assisted by accurate reduction of the facial fractures. If the leak persists beyond 10 days, surgical treatment may be necessary (see Chapter 341).
Infection
Craniofacial wounds are naturally contaminated by the flora of the skin, upper respiratory tract, and mouth, as well as by organisms introduced by the injury. Nonetheless, the incidence of infection of scalp and facial wounds is low as a result of the rich blood supply and because the number of endogenous potential pathogens is low.75
Vascular Injury
Severe frontal impact may result in vascular injury that is often not apparent or overlooked in the early assessments.76,77 Such injuries include carotid cavernous fistulas and carotid or vertebral artery dissection, thrombosis, or aneurysm.
Carotid-Cavernous Fistulas
The most common cause of carotid cavernous fistulas is head trauma, usually blunt and less often penetrating.78 They occur in approximately 1% of patients with facial fractures.79 The internal carotid artery is vulnerable to shearing forces acting between the fixed points of attachment at its dural entry and exit to the cavernous sinus. The fistula may result from a tear in the artery itself or from a tear in meningeal branches of the internal carotid or external carotid arteries within the cavernous sinus. Traumatic fistulas are most often due to a single tear in the internal carotid artery and are high flow. The visual symptoms and signs are chiefly due to the elevated venous pressure. Flow in the superior and inferior ophthalmic veins is frequently reversed, with engorgement and dilation of these vessels. High venous pressure causes chemosis, proptosis, and elevated intraocular pressure and glaucoma; venous distention may also cause paralysis of the third, fourth, and sixth cranial nerves. There is often a latent interval between injury and the signs of a fistula. In such cases, it is considered likely that a minor tear in the internal carotid artery gave rise to a traumatic aneurysm and that delayed rupture of the aneurysm led to the fistula. A few patients suffer cerebral ischemia from diversion of arterial blood into the fistula (steal effect),80 especially if the circle of Willis is markedly asymmetric.81 Nontraumatic fistulas are more often due to tears in meningeal branches and are low flow.
Internal Carotid Artery Injury
The intracranial internal carotid artery may be injured in association with fractures through the petrous temporal bone within the carotid canal or by fractures at the anterior clinoid process.76,82–86 The onset of ischemic symptoms is immediate in a third of patients and occurs within 24 hours in a third. Treatment is generally conservative. Some have suggested extracranial/intracranial bypass for bilateral injuries. Traumatic aneurysms of the supraclinoid internal carotid artery have also been reported.87
Impairments and Disabilities
Neuropsychological
Frontal impact injury may result in a wide range of neuropsychological disabilities that are often attributable to direct injury to the frontal lobes. With severe injuries, brain damage may be widespread. In one study, 83% of patients with a Le Fort pattern of fracture had neuropsychological deficits consistent with brain injury.89 In addition, facial disfigurement may cause considerable emotional distress and social isolation. Neuropsychological assessment and counseling are essential components of a craniofacial service.
Chen CT, Huang F, Tsay PK, et al. Endoscopically assisted transconjunctival decompression of traumatic optic neuropathy. J Craniofac Surg. 2007;18:19.
Cooter RD, David DJ. Computer-based coding of fractures in the craniofacial region. Br J Plast Surg. 1989;42:17.
Crompton J, Hammerton M. Ocular injuries. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:397.
David DJ. Exploration of the orbital floor through a conjunctival approach. Aust N Z J Surg. 1974;44:25.
Gassner R, Tuli T, Hachl O, et al. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004;62:399.
Gruss JS. Complex craniomaxillofacial trauma: evolving concepts in management. A trauma unit’s experience—1989 Fraser B. Gurd lecture. J Trauma. 1990;30:377.
Gruss JS. Fronto-naso-orbital trauma. Clin Plast Surg. 1982;9:577.
Gruss JS, Antonyshyn O, Phillips JH. Early definitive bone and soft-tissue reconstruction of major gunshot wounds of the face. Plast Reconstr Surg. 1991;87:436.
Hanieh A, Moore MH. Immaturity and senescence. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:501.
Hemmy DC, David DJ, Herman GT. Three-dimensional reconstruction of craniofacial deformity using computed tomography. Neurosurgery. 1983;13:534.
Leipziger LS, Manson PN. Nasoethmoid orbital fractures. Current concepts and management principles. Clin Plast Surg. 1992;19:167.
Liebenberg WA, Demetriades AK, Hankins M, et al. Penetrating civilian craniocerebral gunshot wounds: a protocol of delayed surgery. Neurosurgery. 2005;57:293.
Lo YL, Yang TC, Liao CC, et al. Diagnosis of traumatic internal carotid artery injury: the role of craniofacial fracture. J Craniofac Surg. 2007;18:361.
Markowitz BL, Manson PN. Panfacial fractures: organization of treatment. Clin Plast Surg. 1989;16:105.
McKinney A, Ott F, Short J, et al. Angiographic frequency of blunt cerebrovascular injury in patients with carotid canal or vertebral foramen fractures on multidetector CT. Eur J Radiol. 2007;62:385.
Moore MH, David DJ, Cooter RD. Oblique craniofacial fractures in children. J Craniofac Surg. 1990;1:4.
Shenaq SM, Wildberger JE. Maxillofacial and scalp injury in neurotrauma. In: Narayan RK, Dinh T, Povlishock JT, editors. Neurotrauma. New York: McGraw Hill; 1996:225.
Simpson DA, Abbott J. Pathology of injury and repair. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:119.
Singh DJ, Bartlett SP. Pediatric craniofacial fractures: long-term consequences. Clin Plast Surg. 2004;31:499.
Smoot EC3rd, Jernigan JR, Kinsley E, et al. A survey of operative airway management practices for midface fractures. J Craniofac Surg. 1997;8:201.
Trott JA, David D. Definitive management: principles, priorities and basic techniques. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:233.
Yu-Wai-Man P, Griffiths PG. Steroids for traumatic optic neuropathy. Cochrane Database Syst Rev. 4, 2007. CD006032
Yu Wai Man P, Griffiths PG. Surgery for traumatic optic neuropathy. Cochrane Database Syst Rev. 4, 2005. CD005024
1 Iida S, Hassfeld S, Reuther T, et al. Maxillofacial fractures resulting from falls. J Craniomaxillofac Surg. 2003;31:278.
2 Rocchi G, Fadda MT, Marianetti TM, et al. Craniofacial trauma in adolescents: incidence, etiology, and prevention. J Trauma. 2007;62:404.
3 Akama MK, Chindia ML, Macigo FG, et al. Pattern of maxillofacial and associated injuries in road traffic accidents. East Afr Med J. 2007;84:287.
4 Eggensperger Wymann NM, Holzle A, Zachariou Z, et al. Pediatric craniofacial trauma. J Oral Maxillofac Surg. 2008;66:58.
5 Kontio R, Suuronen R, Ponkkonen H, et al. Have the causes of maxillofacial fractures changed over the last 16 years in Finland? An epidemiological study of 725 fractures. Dent Traumatol. 2005;21:14.
6 Ong TK, Dudley M. Craniofacial trauma presenting at an adult accident and emergency department with an emphasis on soft tissue injuries. Injury. 1999;30:357.
7 Taher AA. Management of weapon injuries to the craniofacial skeleton. J Craniofac Surg. 1998;9:371.
8 Follmar KE, Debruijn M, Baccarani A, et al. Concomitant injuries in patients with panfacial fractures. J Trauma. 2007;63:831.
9 Fasola AO, Nyako EA, Obiechina AE, et al. Trends in the characteristics of maxillofacial fractures in Nigeria. J Oral Maxillofac Surg. 2003;61:1140.
10 DeLano MC, Fun FY, Zinreich SJ. Relationship of the optic nerve to the posterior paranasal sinuses: a CT anatomic study. AJNR Am J Neuroradiol. 1996;17:669.
11 Rudderman RH, Mullen RL. Biomechanics of the facial skeleton. Clin Plast Surg. 1992;19:11.
12 Caldicott WJ, North JB, Simpson DA. Traumatic cerebrospinal fluid fistulas in children. J Neurosurg. 1973;38:1.
13 Simpson DA. Clinical examination and grading. In: Reilly PL, Bullak R, editors. Head Injury: Pathophysiology and Management. 2nd ed. London: Hodder Arnold; 2005:143.
14 Cornelius CP, Altenmuller E, Ehrenfeld M. The use of flash visual evoked potentials in the early diagnosis of suspected optic nerve lesions due to craniofacial trauma. J Craniomaxillofac Surg. 1996;24:1.
15 Nayak SR, Kirtane MV, Ingle MV. Fracture line in post head injury optic nerve damage. J Laryngol Otol. 1991;105:203.
16 Stonecipher KG, Conway MD, Karcioglu ZA, et al. Hematoma of the optic nerve sheath after penetrating trauma. South Med J. 1990;83:1230.
17 Converse J, Smith B. Orbital and naso-frontal fractures. et al. Converse J, editor. Reconstructive Plastic Surgery: Principles and Procedures in Correction, Reconstruction and Transplantation, 2nd ed, Philadelphia: WB Saunders, 1977.
18 Barry C, Coyle M, Idrees Z, et al. Ocular findings in patients with orbitozygomatic complex fractures: a retrospective study. J Oral Maxillofac Surg. 2008;66:888.
19 Liebenberg WA, Demetriades AK, Hankins M, et al. Penetrating civilian craniocerebral gunshot wounds: a protocol of delayed surgery. Neurosurgery. 2005;57:293.
20 Ahmad F, Kirkpatrick NA, Lyne J, et al. Buckling and hydraulic mechanisms in orbital blowout fractures: fact or fiction? J Craniofac Surg. 2006;17:438.
21 Katzen JT, Jarrahy R, Eby JB, et al. Craniofacial and skull base trauma. J Trauma. 2003;54:1026.
22 Smoot EC3rd, Jernigan JR, Kinsley E, et al. A survey of operative airway management practices for midface fractures. J Craniofac Surg. 1997;8:201.
23 Hemmy DC, David DJ, Herman GT. Three-dimensional reconstruction of craniofacial deformity using computed tomography. Neurosurgery. 1983;13:534.
24 Gillespie JE, Isherwood I, Barker GR, et al. Three-dimensional reformations of computed tomography in the assessment of facial trauma. Clin Radiol. 1987;38:523.
25 Levy RA, Edwards WT, Meyer JR, et al. Facial trauma and 3-D reconstructive imaging: insufficiencies and correctives. AJNR Am J Neuroradiol. 1992;13:885.
26 Zinreich SJ. 3-D reconstruction for evaluation of facial trauma. AJNR Am J Neuroradiol. 1992;13:893.
27 Crompton J, Hammerton M. Ocular injuries. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:397.
28 Specht CS, Varga JH, Jalali MM, et al. Orbitocranial wooden foreign body diagnosed by magnetic resonance imaging. Dry wood can be isodense with air and orbital fat by computed tomography. Surv Ophthalmol. 1992;36:341.
29 Girard BC, Bouzas EA, Lamas G, et al. Visual improvement after transethmoid-sphenoid decompression in optic nerve injuries. J Clin Neuroophthalmol. 1992;12:142.
30 Gupta AK, Gupta AK, Gupta A, et al. Traumatic optic neuropathy in pediatric population: early intervention or delayed intervention? Int J Pediatr Otorhinolaryngol. 2007;71:559.
31 Guy J, Sherwood M, Day AL. Surgical treatment of progressive visual loss in traumatic optic neuropathy. Report of two cases. J Neurosurg. 1989;70:799.
32 Levin LA, Beck RW, Joseph MP, et al. The treatment of traumatic optic neuropathy: the International Optic Nerve Trauma Study. Ophthalmology. 1999;106:1268.
33 Li KK, Teknos TN, Lai A, et al. Extracranial optic nerve decompression: a 10-year review of 92 patients. J Craniofac Surg. 1999;10:454.
34 Mahapatra AK. Does optic nerve injury require decompression? J Indian Med Assoc. 1990;88:82.
35 Schroder M, Kolenda H, Loibnegger E, et al. [Optic nerve damage following craniocerebral trauma. A critical analysis of trans-ethmoid decompression of the optic nerve.]. Laryngorhinootologie. 1989;68:534.
36 Spoor TC, Hartel WC, Lensink DB, et al. Treatment of traumatic optic neuropathy with corticosteroids. Am J Ophthalmol. 1990;110:665.
37 Cepela MA, George CE. Orbital trauma. Curr Opin Ophthalmol. 1997;8:64.
38 Yu-Wai-Man P, Griffiths PG. Steroids for traumatic optic neuropathy. Cochrane Database Syst Rev. 2007;4:CD006032.
39 Chen CT, Huang F, Tsay PK, et al. Endoscopically assisted transconjunctival decompression of traumatic optic neuropathy. J Craniofac Surg. 2007;18:19.
40 Li HB, Shi JB, Cheng L, et al. Salvage optic nerve decompression for traumatic blindness under nasal endoscopy: risk and benefit analysis. Clin Otolaryngol. 2007;32:447.
41 Yu Wai Man P, Griffiths PG. Surgery for traumatic optic neuropathy. Cochrane Database Syst Rev. 2005;4:CD005024.
42 Becelli R, Renzi G, Perugini M, et al. Craniofacial traumas: immediate and delayed treatment. J Craniofac Surg. 2000;11:265.
43 Gruss JS, Phillips JH. Complex facial trauma: the evolving role of rigid fixation and immediate bone graft reconstruction. Clin Plast Surg. 1989;16:93.
44 Gruss JS, Pollock RA, Phillips JH, et al. Combined injuries of the cranium and face. Br J Plast Surg. 1989;42:385.
45 Gruss JS. Complex craniomaxillofacial trauma: evolving concepts in management. A trauma unit’s experience—1989 Fraser B. Gurd lecture. J Trauma. 1990;30:377.
46 David DJ. Exploration of the orbital floor through a conjunctival approach. Aust N Z J Surg. 1974;44:25.
47 Rahn BA. Theoretical considerations in rigid fixation of facial bones. Clin Plast Surg. 1989;16:21.
48 Rohrich RJ, Hollier LH. Management of frontal sinus fractures. Changing concepts. Clin Plast Surg. 1992;19:219.
49 Gruss JS. Fronto-naso-orbital trauma. Clin Plast Surg. 1982;9:577.
50 Leipziger LS, Manson PN. Nasoethmoid orbital fractures. Current concepts and management principles. Clin Plast Surg. 1992;19:167.
51 Trott JA, David D. Definitive management: principles, priorities and basic techniques. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:233.
52 Gruss JS, Van Wyck L, Phillips JH, et al. The importance of the zygomatic arch in complex midfacial fracture repair and correction of posttraumatic orbitozygomatic deformities. Plast Reconstr Surg. 1990;85:878.
53 Gillies HD, Kilner TP, Stone D. Fractures of the malar-zygomatic compound, with description of a new x-ray position. Br J Surg. 1927;14:651.
54 Wolfe SA. Treatment of post-traumatic orbital deformities. Clin Plast Surg. 1988;15:225.
55 Cooter RD, David DJ. Computer-based coding of fractures in the craniofacial region. Br J Plast Surg. 1989;42:17.
56 Thaller SR, Kawamoto HK. A histologic evaluation of fracture repair in the midface. Plast Reconstr Surg. 1990;85:196.
57 Markowitz BL, Manson PN. Panfacial fractures: organization of treatment. Clin Plast Surg. 1989;16:105.
58 Shenaq SM, Dinh T. Maxillofacial and scalp injury in neurotrauma. In: Narayan RK, Wildberger JE, Povlishock JT, editors. Neurotrauma. New York: McGraw Hill; 1996:225.
59 Antoniades K, Dimitriou C, Triaridis C, et al. Sagittal fracture of the maxilla. J Craniomaxillofac Surg. 1990;18:260.
60 Hanieh A, Moore MH. Immaturity and senescence. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:501.
61 Singh DJ, Bartlett SP. Pediatric craniofacial fractures: long-term consequences. Clin Plast Surg. 2004;31:499.
62 Gassner R, Tuli T, Hachl O, et al. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004;62:399.
63 Ferreira PC, Amarante JM, Silva PN, et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005;115:1500.
64 Moore MH, David DJ, Cooter RD. Oblique craniofacial fractures in children. J Craniofac Surg. 1990;1:4.
65 Kaban LB, Mulliken JB, Murray JE. Facial fractures in children: an analysis of 122 fractures in 109 patients. Plast Reconstr Surg. 1977;59:15.
66 McCoy FJ, Chandler RA, Crow ML. Facial fractures in children. Plast Reconstr Surg. 1966;37:209.
67 Clauser L, Dallera V, Sarti E, et al. Frontobasilar fractures in children. Childs Nerv Syst. 2004;20:168.
68 Greenwald MJ, Boston D, Pensler JM, et al. Orbital roof fractures in childhood. Ophthalmology. 1989;96:491.
69 Ousterhout DK, Vargervik K. Maxillary hypoplasia secondary to midfacial trauma in childhood. Plast Reconstr Surg. 1987;80:491.
70 Gruss JS, Antonyshyn O, Phillips JH. Early definitive bone and soft-tissue reconstruction of major gunshot wounds of the face. Plast Reconstr Surg. 1991;87:436.
71 Tan E. Injuries of Soft Tissues, Ducts and Nerves. Edinburgh: Churchill Livingstone; 1995.
72 Balasubramanian C, Kaliaperumal C, Jadun CK, et al. Transorbital intracranial penetrating injury—an anatomical classification. Surg Neurol. 2009;71:238-240.
73 Park SH, Cho KH, Shin YS, et al. Penetrating craniofacial injuries in children with wooden and metal chopsticks. Pediatr Neurosurg. 2006;42:138.
74 Morgan BD, Madan DK, Bergerot JP. Fractures of the middle third of the face—a review of 300 cases. Br J Plast Surg. 1972;25:147.
75 Simpson DA, Abbott J. Pathology of injury and repair. In: David DJ, Simpson DA, editors. Craniomaxillofacial Trauma. Edinburgh: Churchill Livingstone; 1995:119.
76 Lo YL, Yang TC, Liao CC, et al. Diagnosis of traumatic internal carotid artery injury: the role of craniofacial fracture. J Craniofac Surg. 2007;18:361.
77 McKinney A, Ott F, Short J, et al. Angiographic frequency of blunt cerebrovascular injury in patients with carotid canal or vertebral foramen fractures on multidetector CT. Eur J Radiol. 2007;62:385.
78 Gratz KW, Imhof HG, Valavanis A. Traumatic carotid cavernous sinus fistula due to a gun shot injury. Int J Oral Maxillofac Surg. 1991;20:280.
79 Chang CJ, Chen YR, Noordhoff MS, et al. Facial bone fracture associated with carotid-cavernous sinus fistula. J Trauma. 1990;30:1335.
80 Watanabe A, Ishii R, Suzuki Y, et al. The cerebral circulation in cases of carotid cavernous fistula. Findings of single photon emission computed tomography. Neuroradiology. 1990;32:108.
81 Iida K, Uozumi T, Arita K, et al. Steal phenomenon in a traumatic carotid-cavernous fistula. J Trauma. 1995;39:1015.
82 Ajir F, Tibbetts JC. Post-traumatic occlusion of the supraclinoid internal carotid artery. Neurosurgery. 1981;9:173.
83 Carter DA, Mehelas TJ, Savolaine ER, et al. Basal skull fracture with traumatic polycranial neuropathy and occluded left carotid artery: significance of fractures along the course of the carotid artery. J Trauma. 1998;44:230.
84 Morgan MK, Besser M, Johnston I, et al. Intracranial carotid artery injury in closed head trauma. J Neurosurg. 1987;66:192.
85 Yang TC, Lo YL, Huang YC, et al. Traumatic anterior cerebral artery aneurysm following blunt craniofacial trauma. Eur Neurol. 2007;58:239.
86 York G, Barboriak D, Petrella J, et al. Association of internal carotid artery injury with carotid canal fractures in patients with head trauma. AJR Am J Roentgenol. 2005;184:1672.
87 Pozzati E, Gaist G, Servadei F. Traumatic aneurysms of the supraclinoid internal carotid artery. J Neurosurg. 1982;57:418.
88 Ferreras J, Junquera LM, Garcia-Consuegra L. Intracranial placement of a nasogastric tube after severe craniofacial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:564.
89 Wood MM, Reilly PL, David DJ. Neuropsychologic outcome after craniofacial fracture. J Craniofac Surg. 1990;1:163.
90 Jimenez DF, Sundrani S, Barone CM. Posttraumatic anosmia in craniofacial trauma. J Craniomaxillofac Trauma. 1997;3:8.