Chapter 12 Cranial Nerve Innervation of Ocular Structures
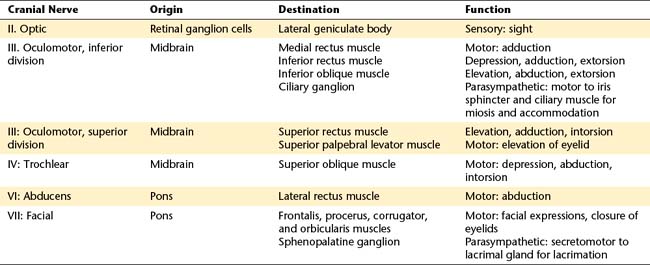
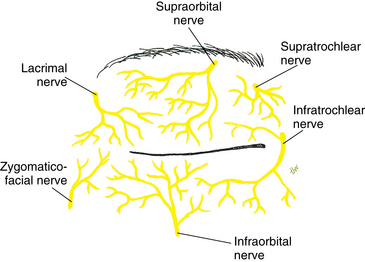
The orbital structures are innervated by cranial nerves (CNs) II, III, IV, V, VI, and VII (Table 12-1). Motor functions of the striated muscles are controlled by CN III, the oculomotor nerve; CN IV, the trochlear nerve; CN VI, the abducens nerve; and CN VII, the facial nerve. CN V, the trigeminal nerve, carries the sensory supply from the orbital structures. CN II, the optic nerve, carries visual information and is discussed in Chapter 13. This chapter discusses sensory and motor innervation of the orbit, including pathways, functions, and presenting signs of dysfunction.
The Nervous System
Efferent fibers, either somatic or autonomic, carry information from the CNS to the target structures: muscles, organs, or glands. The efferent pathway in the somatic system generally consists of a fiber that runs the distance from the CNS to the target muscle. The autonomic pathway generally has a synapse within its efferent pathway (see Chapter 14).
Afferent Pathway: Orbital Sensory Innervation
The eye is richly supplied with sensory nerves that carry sensations of touch, pressure, warmth, cold, and pain. Sensations from the cornea, iris, conjunctiva, and sclera consist primarily of pain; even light touching of the cornea is registered as irritation or pain.1
Trigeminal Nerve
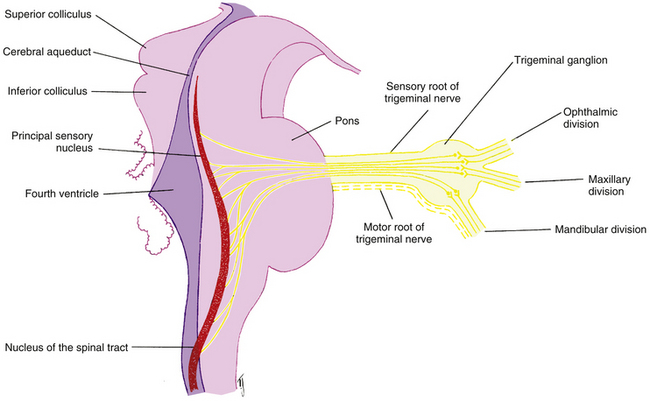
The fibers of the trigeminal nerve (CN V) serving ocular structures are sensory and originate in the innervated structures. The description of the pathways of these nerves begins at the involved structures and follows the nerves as they join to become larger nerves, come together in the ganglion of the fifth cranial nerve, and then exit the ganglion and enter the pons. It is hoped that this presentation, although unconventional, will enable the reader to keep in mind the actual direction of the action potential, and thus the information flow, in these fibers. Figure 12-1 shows the major branches and paths of the trigeminal nerve within the orbit.
Ophthalmic Division of Trigeminal Nerve
Nasociliary Nerve
Sensory fibers from the structures of the medial canthal area—caruncle, canaliculi, lacrimal sac, medial aspect of the eyelids, and skin at the side of the nose —join to form the infratrochlear nerve. This nerve penetrates the orbital septum, enters the orbit below the trochlea, and runs along the upper border of the medial rectus muscle, becoming the nasociliary nerve as other branches join it (see Figure 12-1).
Sensory fibers from the skin along the center of the nose, the nasal mucosa, and the ethmoid sinuses form the anterior ethmoid nerve; fibers from the ethmoid sinuses and the sphenoid sinus form the posterior ethmoid nerve. The ethmoid nerves enter the orbit with their companion arteries through foramina within the frontoethmoid suture.2 Both nerves join the nasociliary nerve as it runs along the medial aspect of the orbit (see Figure 12-1).
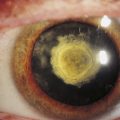
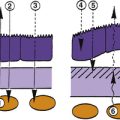
Corneal sensory innervation is dense, estimated to be 400 times as dense as other epithelial tissue innervation.3 Three networks of nerves are formed. One is located in the corneal epithelium, another (the subepithelial plexus) is in the anterior stroma, and the third, the stromal plexus, is in the middle of the stroma4 (Figure 12-2). No nerves are found in posterior stroma, Descemet’s membrane, or endothelium. The fibers from these plexus come together in peripheral stroma and radiate out into the limbus as 70 to 80 branches; they become myelinated in the last 2 mm of the cornea.5–7
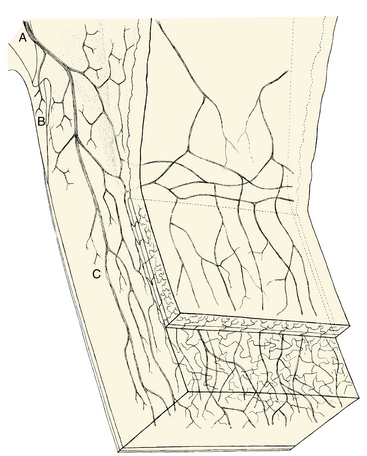
FIGURE 12-2 Innervation of limbus and cornea.
(From Hogan MJ, Alvarado JA, Weddell JE, editors: Histology of the human eye, Philadelphia, 1971, Saunders.)
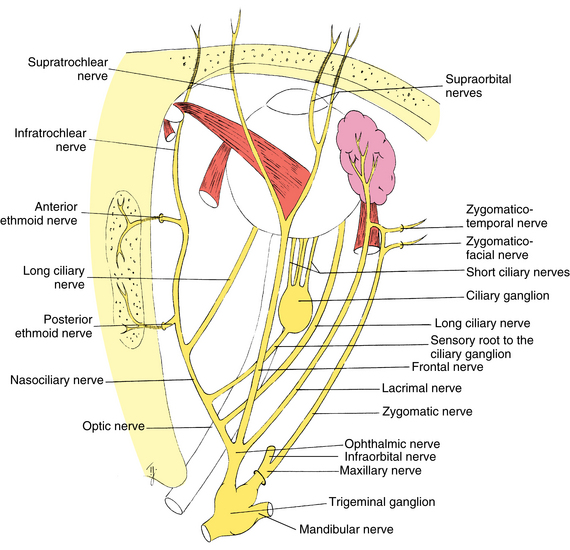
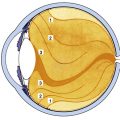
Some of these branches join with nerves from other anterior segment structures to form two long ciliary nerves. These long ciliary nerves, one on the lateral side and one on the medial side of the globe, course between the choroid and sclera to the back of the eye, where they leave the globe at points approximately 3 mm on each side of the optic nerve (Figure 12-3). (In addition to afferent fibers, the long ciliary nerves transmit sympathetic fibers to the dilator muscle of the iris.) The two long ciliary nerves then join the nasociliary nerve.
Clinical Comment: (Scleral) Nerve Loops (of Axenfeld)
A slight variation can occur in the pathway of the long ciliary nerve in which the fibers loop into the sclera from the suprachoroidal space, forming a dome-shaped elevation about 2 mm from the limbus on either the nasal or the temporal side. Often this raised area is pigmented, usually blue or black, and should be differentiated from a melanoma.8 The nerve loop may be painful when touched, a characteristic that should aid in its diagnosis.5
The other branches radiating from the cornea into the limbus join other sensory nerves from the anterior segment; they enter the choroid, join with the choroidal nerves, then course to the back of the eye, where they leave as 6 to 10 short ciliary nerves (see Figure 12-3). The short ciliary nerves exit the sclera in a ring around the optic nerve in company with the short posterior ciliary arteries and enter the ciliary ganglion (see Figure 12-1). The sensory fibers do not synapse but pass through the ganglion, leaving as the sensory root of the ciliary ganglion, which then joins the nasociliary nerve. (The short ciliary nerves carry sympathetic and parasympathetic fibers in addition to sensory fibers.)
Thus, the nasociliary nerve is formed by the joining of the infratrochlear nerve, the anterior and posterior ethmoid nerves, the long ciliary nerves, and the sensory root of the ciliary ganglion (see Figure 12-1). The nasociliary nerve exits the orbit by passing through the oculomotor foramen within the common tendinous ring and the superior orbital fissure into the cranial cavity.
Clinical Comment: Herpes Zoster
HERPES ZOSTER is an acute CNS infection caused by the varicella-zoster virus. Signs and symptoms include pain and rash in the distribution area supplied by the affected sensory nerves.9 It is believed that the virus lies dormant in a sensory ganglion and, on becoming activated, migrates down the sensory pathway to the skin.10 An eruption of herpes zoster is more common in elderly persons but may occur at any age and may be related to a delayed hypersensitivity reaction.11 Approximately 10% of all cases affect the ophthalmic division of the trigeminal nerve.12 Involvement of the tip of the nose often indicates that the eye will also be involved, reflecting the distribution of the nasociliary branches. This association of ocular involvement with zoster affecting the tip of the nose is the Hutchinson sign.13
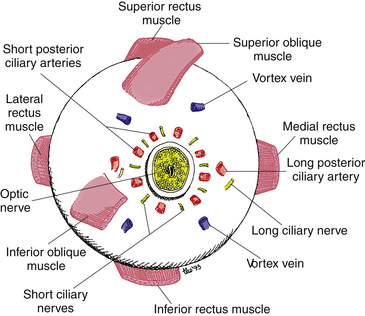
Frontal Nerve
Sensory fibers from the skin and muscles of the forehead and upper eyelid come together and form the supratrochlear nerve. This nerve enters the orbit by piercing the superior medial corner of the orbital septum (Figure 12-4).
Sensory fibers from the skin and muscles of the forehead and upper eyelid form a second nerve, the supraorbital nerve, lateral to the supratrochlear nerve. The supraorbital nerve enters the orbit as one or two branches: one branch enters through the supraorbital notch, accompanying the supraorbital artery. The supraorbital nerve joins the supratrochlear nerve midway in the orbit and forms the frontal nerve (see Figure 12-1). The frontal nerve courses back through the orbit between the levator muscle and the periorbita, exiting the orbit through the superior orbital fissure above the common tendinous ring.
Lacrimal Nerve
Sensory fibers from the lateral aspect of the upper eyelid and temple area come together and enter the lacrimal gland; they join the sensory fibers that serve the gland itself to form the lacrimal nerve. The lacrimal nerve leaves the gland and runs posteriorly along the upper border of the lateral rectus muscle (see Figure 12-1). It receives a branch from the zygomatic nerve containing the autonomic innervation of the lacrimal gland. The lacrimal nerve exits the orbit through the superior orbital fissure above the muscle cone.
Ophthalmic Nerve Formation
After exiting the orbit, the nasociliary nerve, the lacrimal nerve, and the frontal nerve join and form the ophthalmic division of the trigeminal nerve (see Figure 12-1). The ophthalmic nerve then enters the lateral wall of the cavernous sinus, coursing between the two dural layers.14 While in the wall of the sinus the nerve receives sensory fibers from the oculomotor, trochlear, and abducens nerves. Some of these fibers probably carry proprioceptive information from the extraocular muscles.15
Maxillary Division of Trigeminal Nerve
Infraorbital Nerve
The infraorbital nerve, formed by sensory fibers from the cheek, upper lip, and lower eyelid, enters the maxillary bone through the infraorbital foramen (Figure 12-5). It runs posteriorly through the infraorbital canal and groove; while it is in the maxillary bone, branches join from the upper teeth and maxillary sinus. As the nerve leaves the infraorbital groove it exits the orbit through the inferior orbital fissure and joins other fibers in forming the maxillary nerve.
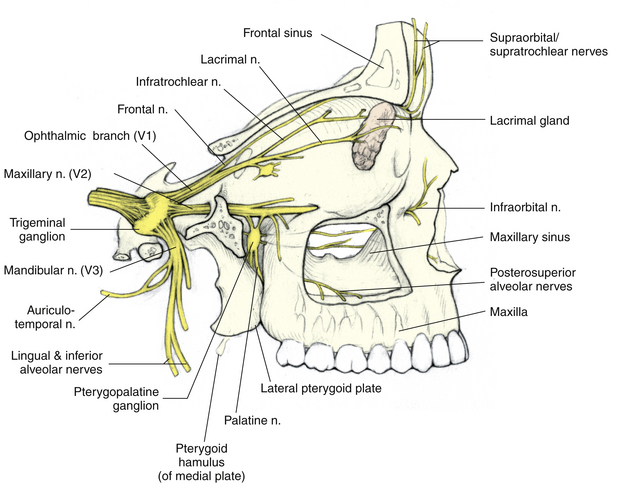
FIGURE 12-5 Three divisions of trigeminal nerve.
(From Mathers LH, Chase RA, Dolph J, et al: Clinical anatomy principles, St Louis, 1996, Mosby.)
Clinical Comment: Referred Pain
REFERRED PAIN is pain felt in an area remote from the actual site of involvement; however, the two areas usually are connected by a sensory nerve network. Frequently, the pathways of the trigeminal nerve are involved in referred pain. A common example is a momentary severe bilateral frontal headache sometimes experienced when an individual eats ice cream.5 An abscessed tooth can cause pain described by a patient as ocular pain and should be suspected when no orbital cause for the pain can be found. This situation likely occurs because the overload of sensation carried by the infraorbital nerve from the upper teeth is interpreted by the brain as coming from another area also served by the trigeminal nerve.
Zygomatic Nerve
Sensory fibers from the lateral aspect of the forehead enter the orbit through a foramen in the zygomatic bone as the zygomaticotemporal nerve. Fibers from the lateral aspect of the cheek and lower eyelid enter the orbit through a foramen in the zygomatic bone as the zygomaticofacial nerve.13 These two nerves join to become the zygomatic nerve and course along the lateral orbital wall, exiting the orbit through the inferior orbital fissure and joining with the maxillary nerve (see Figure 12-1).
Maxillary Nerve Formation
Having been formed by the joining of the infraorbital nerve, the zygomatic nerve, and nerves from the roof of the mouth, upper teeth and gums, and mucous membranes of the cheek, the maxillary nerve traverses the area between the maxilla and the sphenoid bone. As it passes near the pterygopalatine fossa, it receives some autonomic fibers from the pterygopalatine ganglion (see Figure 12-5). (These autonomic fibers are destined for the lacrimal gland and are discussed in Chapter 14.) The maxillary nerve enters the skull through the foramen rotundum.
Trigeminal Nerve Formation
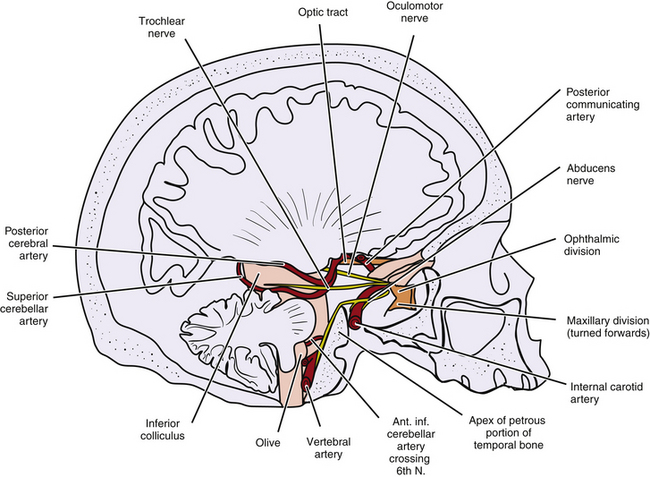
As the ophthalmic and maxillary divisions enter the skull, they run posteriorly within the lateral wall of the cavernous sinus (Figure 12-6).16,17 The mandibular division lies just below the cavernous sinus. The sensory fibers from the three divisions enter the trigeminal ganglion (gasserian ganglion, semilunar ganglion), where they synapse. The ganglion, flattened and semilunar in shape, is located lateral to the internal carotid artery and the posterior portion of the cavernous sinus. The motor fibers of the mandibular division, which innervate the muscles of mastication, pass along the lower edge of the ganglion.18 Only the sensory fibers synapse within the ganglion.
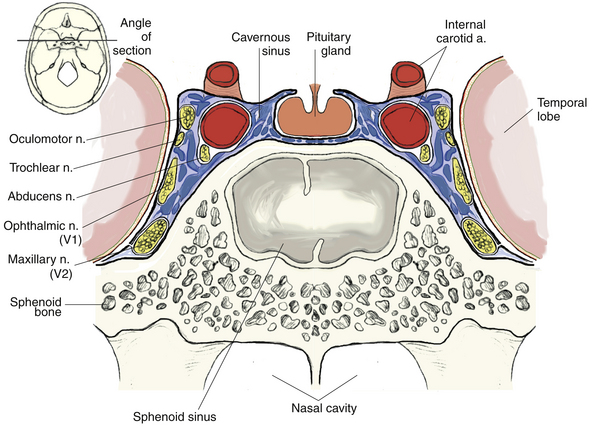
FIGURE 12-6 Detailed cross section of cavernous sinus.
(From Mathers LH, Chase RA, Dolph J, et al: Clinical anatomy principles, St Louis, 1996, Mosby.)
The fibers leave the trigeminal ganglion and enter the lateral aspect of the pons as either the sensory root or the motor root of the trigeminal nerve. The sensory root carries information from the structures of the face and head, including all orbital structures. After entering the brain stem, these fibers form an ascending and a descending tract, both terminating in sensory nuclei of the trigeminal nerve (Figure 12-7). The ascending tract terminates in the principal sensory nucleus in the pons; it registers the sensations of touch and pressure.1 The descending tract, which carries pain and temperature sensations, courses through the pons and medulla to the elongated nucleus of the spinal tract.1 The tract extends into the second cervical segment of the spinal cord.19 Information from the trigeminal nuclei is relayed to the thalamus.
Clinical Comment: Oculocardiac Reflex
THE OCULOCARDIAC REFLEX consists of bradycardia (slowed heartbeat), nausea, and faintness and can be elicited by pressure on the globe or stretch on the extraocular muscles (e.g., during ocular surgery).20–22 Fibers from the trigeminal spinal nucleus project into the reticular formation near the vagus nerve nuclei and can activate vagus synapses, precipitating this reflex. The motor aspect of the reflex can be blocked by retrobulbar anesthesia or intravenous or intramuscular atropine.1,13,23,24
Efferent Pathway: Motor Nerves
Oculomotor Nerve: Cranial Nerve III
Oculomotor Nucleus
The oculomotor nucleus is located in the midbrain, at the level of the superior colliculus, ventral to the cerebral aqueduct, and dorsal to the medial longitudinal fasciculus (Figure 12-8).28 It extends in a column from the posterior edge of the floor of the third ventricle to the trochlear nucleus.2,13
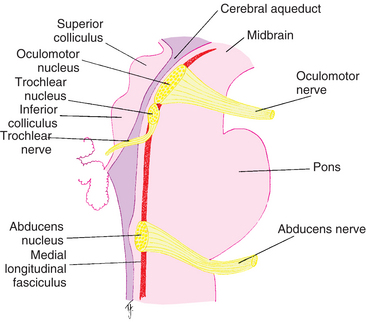
FIGURE 12-8 Sagittal section through brainstem showing trigeminal, oculomotor, trochlear, abducens, and facial nuclei.
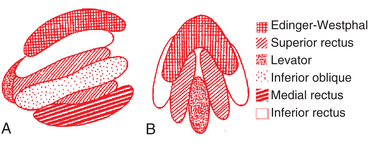
A definitive area or subnucleus within the oculomotor nucleus controls each muscle. The proposed arrangement of the subnuclei are postulated primarily on the basis of animal models.23,25–27 The nucleus for the medial rectus is located toward the lower border of the oculomotor nucleus; the inferior rectus nucleus lies toward the upper border, with the nucleus for the inferior oblique between. The nucleus of the superior rectus lies in the medial and caudal two thirds of the oculomotor nucleus. Each of these subnuclei are found in the right and left oculomotor nucleus. The nucleus for the levator muscle is single and is located centrally in the caudal area (Figure 12-9).
Fibers to the inferior rectus, inferior oblique, and medial rectus muscles supply the ipsilateral eye; fibers innervating the superior rectus muscle decussate and supply the contralateral eye. The decussating fibers pass through the opposite superior rectus nucleus; thus damage to the right oculomotor nucleus might have bilateral superior rectus muscle involvement.27–30 The centrally placed caudal nucleus provides innervation for both levator muscles.
An autonomic nucleus, the accessory third nerve nucleus (Edinger-Westphal nucleus), supplies parasympathetic innervation to the ciliary and iris sphincter muscles. It is located in the rostral, ventral portion of the oculomotor nucleus30,31 (see Figure 12-9).
Oculomotor Nerve Pathway
Fibers from each of the individual nuclei join, forming the fascicular part of the nerve that passes through the red nucleus and the decussating fibers of the superior cerebellar peduncle.32 These fibers emerge just medial to the cerebral peduncles and within the interpeduncular fossa on the anterior aspect of the midbrain as the oculomotor nerve. The nerve passes between the superior cerebellar and posterior cerebral arteries as it runs forward, lateral to, and slightly inferior to the posterior communicating artery of the circle of Willis (Figure 12-10). The nerve pierces the roof of the cavernous sinus and runs within the two dural layers of its lateral wall above the trochlear nerve2,14,16 (see Figure 12-6). While in the cavernous sinus, the oculomotor nerve sends small sensory branches (likely proprioceptive) to the ophthalmic nerve and receives sympathetic fibers from the plexus around the internal carotid artery.2,19
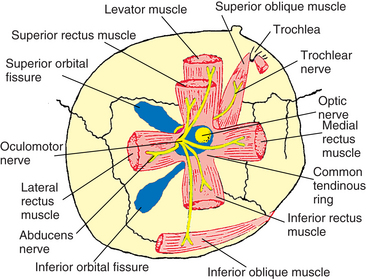
The oculomotor nerve exits the sinus and enters the orbit through the superior orbital fissure, having divided into superior and inferior divisions; both divisions are located within the oculomotor foramen. The superior branch runs medially above the optic nerve and enters the superior rectus on its inferior surface; additional fibers either pierce the muscle or pass around its border to innervate the levator14,33 (Figure 12-11).
The inferior branch runs below the optic nerve and divides into three branches. One branch enters the medial rectus on its lateral surface, and one enters the inferior rectus on its upper surface (see Figure 12-11). The third branch gives off parasympathetic fibers that form the parasympathetic root extending to the ciliary ganglion; then it runs along the lateral border of the inferior rectus, crossing it to enter the inferior oblique muscle near its midpoint.5,14,34,35
Trochlear Nerve: Cranial Nerve IV
The trochlear nerve innervates the superior oblique muscle.
Trochlear Nucleus
The trochlear nucleus is located in the midbrain, at the level of the inferior colliculus, anterior to the cerebral aqueduct, dorsal to the medial longitudinal fasciculus, and below the oculomotor nucleus32 (see Figure 12-8). The fibers travel dorsally and decussate. CN IV is the only cranial nerve to cross; thus the trochlear nucleus innervates the contralateral superior oblique muscle.
Trochlear Nerve Pathway
Of the cranial nerves, the trochlear nerve is the only one that leaves the dorsal aspect of the CNS. It is the most slender of the cranial nerves, and its attachment is very delicate. (The small diameter of the nerve probably reflects the fact that it supplies only one muscle, the most slender of the extraocular muscles.) As the trochlear nerve emerges from the dorsal midbrain immediately below the inferior colliculus, it decussates and curves around the cerebral peduncle at the upper border of the pons, approximately paralleling the superior cerebellar and posterior cerebral arteries. It passes between these two vessels and runs forward lateral to the oculomotor nerve (see Figure 12-10).
The trochlear nerve enters the wall of the cavernous sinus and lies between the oculomotor nerve and the ophthalmic division of the trigeminal nerve (see Figure 12-6).5,16 While in the sinus, the trochlear nerve sends sensory fibers (likely proprioceptive) to the ophthalmic nerve. It enters the orbit through the superior orbital fissure above the common tendinous ring, outside the muscle cone (see Figure 12-11). The trochlear nerve runs with the frontal nerve to the medial side of the orbit above the levator and superior rectus muscles and enters the upper surface of the superior oblique muscle.10
Abducens Nerve: Cranial Nerve VI
The abducens nerve innervates the lateral rectus muscle.
Abducens Nucleus
The abducens nucleus is located near the inferior dorsal midline of the pons beside the floor of the fourth ventricle (see Figure 12-8). The fibers from the nucleus pass through the pons and lie adjacent to the corticospinal tract for part of their path32; they exit in the groove between the pons and the medulla oblongata. The abducens nucleus also contains internuclear neurons that communicate with the nucleus for the contralateral medial rectus muscle in the oculomotor complex via the medial longitudinal fasciculus.36 This is the pathway for conjugate horizontal eye movements. This pathway receives information from higher CNS centers, including the paramedial pontine reticular formation, the cerebellum, and the vestibular nucleus. Thus coordinated movement of the ipsilateral lateral rectus muscle and the contralateral medial rectus muscle results in conjugate horizontal eye movement.36
Abducens Nerve Pathway
In its long, tortuous, intracranial course, the abducens nerve runs along the occipital bone at the base of the skull and up along the posterior slope of the petrous portion of the temporal bone, makes a sharp bend over the petrous ridge (see Figure 12-10), and enters the cavernous sinus.5,13,37 Within the sinus it lies near the lateral wall of the internal carotid artery6,38 (see Figure 12-6). Small sympathetic branches leave the internal carotid plexus and travel with the abducens nerve. The abducens carries these autonomic fibers and sensory fibers, which are possibly proprioceptive, to the ophthalmic division of the trigeminal nerve.38 The abducens nerve enters the orbit through the superior orbital fissure within the common tendinous ring and innervates the lateral rectus muscle on the medial surface (see Figure 12-11).
Superior Orbital Fissure
The trochlear, frontal, and lacrimal nerves as well as the superior ophthalmic vein are located in the superior orbital fissure above the muscle cone. The superior and inferior divisions of the oculomotor nerve, the abducens nerve, and the nasociliary nerve are located within the superior orbital fissure and the common tendinous ring. The inferior ophthalmic vein lies below the fissure and the tendinous ring (see Figure 8-15).
Control of Eye Movements
Communication among areas of the CNS is necessary to produce controlled and coordinated eye movements. The corticonuclear tract contains fibers that travel from the cerebral hemispheres to the nuclei of CNs III, IV, and VI; the tectobulbar tract connects the superior colliculus to the CN III, IV, and VI nuclei. The medial longitudinal fasciculus extends from the midbrain into the spinal cord and connects the vestibular nucleus, the oculomotor nucleus, the abducens nucleus, and the trochlear nucleus, providing a connection between eye movement control and the vestibular apparatus (see Figure 12-8).
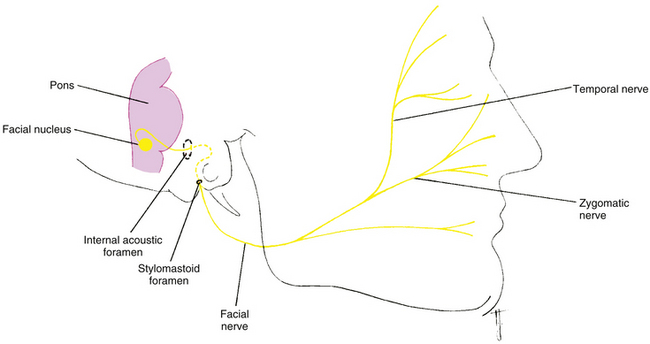
Facial Nerve: Cranial Nerve VII
The facial nerve has two roots: the large motor root innervates the facial muscles, and the smaller root contains sensory and parasympathetic fibers. The sensory fibers carry taste sensations from the tongue. The parasympathetic nerves supply secretomotor fibers to various glands of the face; those supplying the lacrimal gland are discussed in Chapter 14.
Facial Nucleus
The motor nucleus of the facial nerve is located in the reticular formation of the pons. The upper segment of the nucleus supplies the frontalis, procerus, corrugator superciliaris, and orbicularis muscles, and the lower segment supplies the remaining facial muscles.39,40
Facial Nerve Pathway
The fibers leave the facial nucleus, arch around the abducens nucleus, and emerge as the facial nerve from the brain stem at the lower border of the pons. The facial nerve enters the internal acoustic foramen in the petrous portion of the temporal bone and runs through a canal in the bone. While in the temporal bone, parasympathetic fibers en route to the lacrimal gland are given off as the greater petrosal nerve.39,40 The motor fibers of the facial nerve emerge through the stylomastoid foramen, pass below the external auditory canal, travel over the mandibular ramus, and divide into several branches (Figure 12-12). The upper two — the temporal and zygomatic branches — supply the frontalis, procerus, corrugator, and orbicularis muscles.
Clinical Comment: Cranial Nerve Damage
In some studies of isolated extraocular muscle nerve paralysis, the sixth cranial nerve is reported to be affected most often, and the fourth cranial nerve affected least often.41–43 The tortuosity and length of the abducens nerve make it susceptible to compression and stretching injuries and may explain why it is damaged so frequently.16
A number of clinical signs and symptoms accompany damage to the motor nerves that innervate the extraocular muscles. Muscle paresis or paralysis will be evident in testing ocular motility (as described in Chapter 10). In acquired extraocular muscle impairment, a patient often attempts to minimize diplopia by carrying the head in a compensatory position. If a horizontal deviation is present, the head will be turned to the right or left. With a vertical deviation, the head is raised or lowered, and if a torsional deviation occurs the head is tilted toward the shoulder usually away from the involved side.35 With right superior oblique involvement the head may be turned to the left, positioned down, and tilted toward the left shoulder44,45 (Figure 12-13).
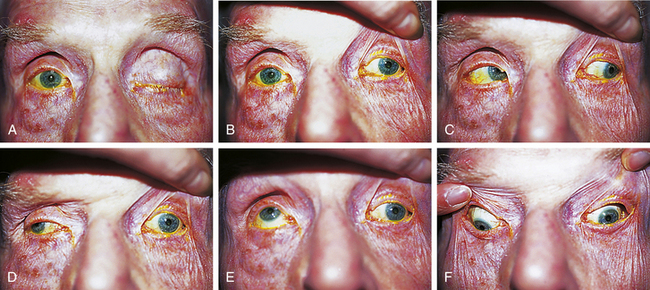
Clinical Comment: Oculomotor Damage
Midbrain Involvement
A lesion in the midbrain can affect the entire oculomotor nucleus or selectively affect only some subnuclei; however, such selective damage is unusual.28 If the lesion affects the entire oculomotor nucleus, the muscles involved are the ipsilateral medial rectus, inferior rectus, and inferior oblique, contralateral superior rectus, and both levators. The ipsilateral superior rectus might be involved as well because the decussating fibers pass through the contralateral superior rectus nucleus.28,32 Dilation of the pupil may also be present. The trochlear nucleus is near the oculomotor nucleus, and if it too is involved, the contralateral superior oblique muscle will be affected. The clinical presentation would show the ipsilateral eye positioned out in primary position and only able to move in as far as the midline. The contralateral eye would be unable to elevate in abduction and unable to depress in adduction.
Intracranial Involvement
The oculomotor nerve lies near several blood vessels in its intracranial path and frequently is affected by an aneurysm of the posterior communicating artery.46An aneurysm of the superior cerebellar artery or the posterior cerebral artery could also impinge on the nerve, damaging fibers.
Once the oculomotor nerve exits the midbrain, all its fibers supply the ipsilateral eye, and the dysfunction is unilateral. Damage to the nerve results in ptosis because of levator muscle paralysis; in primary position, the eye is positioned out because of the unopposed action of the superior oblique and lateral rectus muscles (Figure 12-14, A and B). (Because the superior oblique muscle is unaffected, the eye also should be positioned down, but clinically this is not always evident.47) The eye cannot adduct (Figure 12-14, D) and, in the abducted position, cannot move up or down (Figure 12-14, E and F).2 If injury involves the cerebral peduncles, a contralateral hemiparesis will be present.48 In paralysis of the iris sphincter and ciliary muscle, the pupil will be dilated, and accommodation will not occur.
Incomplete lesions of the oculomotor nerve are possible. In external ophthalmoplegia, the extraocular muscles are paralyzed and the intrinsic muscles (those to the iris sphincter and the ciliary muscle) are spared; in internal ophthalmoplegia the internal muscles are paralyzed and the extraocular muscles are spared. As the oculomotor nerve exits the midbrain, the parasympathetic fibers are superficial, and as the nerve nears the orbit, the parasympathetic fibers move into the center of the nerve and therefore are better protected in compressive lesions. The parasympathetic fibers are often spared in ischemic lesions, accounting for normal pupillary responses usually seen with diabetic ophthalmoplegia.28,49–51 Third nerve palsies that include a dilated pupil are highly suspicious of a compressive lesion.
Aberrant Regeneration of the Oculomotor Nerve
After injury, the brain may attempt to repair a nerve, and some attempts may be misdirected, eliciting an unusual clinical presentation. Lid elevation might occur with downward gaze or adduction.32 Some cases even can involve pupil responses; fibers going to the inferior oblique may sprout branches that also innervate the sphincter, causing pupillary constriction on elevation. Fibers innervating the medial rectus may send sprouts that innervate the sphincter, causing miosis with adduction or convergence.
Clinical Comment: Trochlear Damage
When the superior oblique muscle is affected by trochlear nerve damage, the eye is elevated in primary gaze and is unable to move down in the adducted position. The head may be tilted toward the opposite shoulder to compensate for the unopposed extortion of the inferior oblique muscle5 (see Figure 12-13). Under the age of 10 years, palsies involving the trochlear nerve are usually congenital, and between 21 and 40 years of age the usual cause is trauma; otherwise the palsy may be idiopathic.52–54
Intracranial Involvement
For the most part, the trochlear nerve follows the same path as the oculomotor nerve and is susceptible to the same injuries. Damage to the trochlear nerve affects the ipsilateral superior oblique muscle, causing the eye to be elevated in primary gaze and unable to move down in the adducted position (Figure 12-15).
Clinical Comment: Abducens Damage
Damage to the abducens nerve results in paralysis of the lateral rectus muscle; because of the unopposed action by the medial rectus muscle, a convergent strabismus is evident.55 The eye will be unable to abduct (Figure 12-16). The patient might try to compensate for the diplopia by turning the face toward the paralyzed side.5
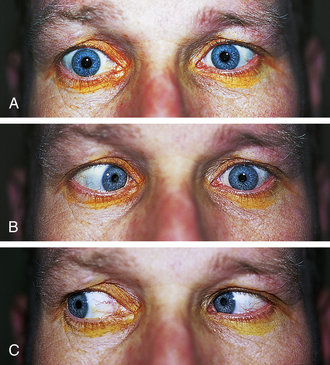
FIGURE 12-16 Sixth nerve palsy OS. A, Primary position, left eye positioned in. B, Unable to abduct; C, Normal adduction.
(From Kanski JJ: Clinical ophthalmology: a systematic approach, ed 5, Oxford, UK, 2003, Butterworth-Heinemann.)
Intracranial Involvement
The course of the abducens nerve renders it particularly susceptible to increased intracranial pressure, which causes the brain stem to be displaced posteriorly, stretching the nerve over the bony prominence of the temporal bone.13,37,41 Fractures of the base of the skull and aneurysms of the basilar and carotid arteries can affect the abducens nerve.
1. Burton H. Somatic sensations from the eye. In: Hart W.M.Jr., editor. Adler’s physiology of the eye. ed 9. St Louis: Mosby; 1992:71.
2. Warwick R. Eugene Wolff’s anatomy of the eye and orbit, ed 7. Philadelphia: Saunders; 1976. p 275
3. Ehlers N. Hjortdal J: The cornea. Fischbarg J., editor. The biology of the eye, vol 10. Elsevier; 2006:83-111.
4. Oliveira-Soto L., Efron N. Morphology of corneal nerves using confocal microscopy. Cornea. 2001;20(4):374.
5. Wirtschafter J.D. The peripheral courses of the third, fourth, fifth, sixth, and seventh cranial nerves. In: Reeh M.J., Wobig J.L., Wirtschafter J.D., editors. Ophthalmic anatomy. San Francisco: American Academy of Ophthalmology; 1981:234.
6. Müller L.J., Pels E., Vrensen G.F. Ultrastructural organization of human corneal nerves. Invest Ophthalmol Vis Sci. 1996;37(4):476.
7. Müller L.J., Pels E., Vrensen G.F., et al. Architecture of human corneal nerves. Invest Ophthalmol Vis Sci. 1997;38(5):985.
8. Catania L.J. Primary care of the anterior segment. East Norwalk, Conn: Appleton & Lange; 1988. p 74
9. Berkow R., editor. The Merck manual, ed 14. Rahway, NJ: Merck; 1982:187.
10. Bartlett J.D., Jaanus S.D. Clinical ocular pharmacology, ed 2. Boston: Butterworth-Heinemann; 1989. p 544
11. Schlaegel T.F. Uveitis associated with viral infections. In: Duane T.D., Jaeger E.A., editors. Clinical ophthalmology. Philadelphia: Harper & Row, 1982.
12. Kanski J.J. Clinical ophthalmology, ed 3. London: Butterworth-Heinemann; 1994. p 111
13. Doxanas M.T., Anderson R.L. Clinical orbital anatomy. Baltimore: Williams & Wilkins; 1984. p 131
14. Iaconetta G., de Notaris M., Cavallo L.M., et al. The oculomotor nerve: microanatomical and endoscopic study. Neurosurgery. 2010;66:593-601.
15. Feldon S.E., Burde R.M. The oculomotor system. In Hart W.M.Jr., editor: Adler’s physiology of the eye, ed 9, St Louis: Mosby, 1992.
16. Umansky J., Nathan H. The lateral wall of the cavernous sinus: with special reference to the nerves related to it. J Neurosurg. 1982;56:228.
17. Nuza A.B., Taner D. Anatomical variations of the intracavernous branches of the internal carotid artery with reference to the relationship of the internal carotid artery and sixth cranial nerve. A microsurgical study. Acta Anat. 1990;138:238.
18. Beck R.W., Smith C.H. Trigeminal nerve. Tasman W., Jaeger E.A., editors. Duane’s foundations of clinical ophthalmology, vol 1. Philadelphia: Lippincott, 1994.
19. Warwick R., Williams P.L., editors. Gray’s anatomy, ed 35. Philadelphia: Saunders; 1973:1001-1006.
20. Stott D.G. Reflex bradycardia in facial surgery. Br J Plast Surg. 1989;42(5):595.
21. Eustis H.S., Eiswirth C.C., Smith D.R. Vagal responses to adjustable sutures in strabismus correction. Am J Ophthalmol. 1992;114(3):307.
22. Hampl K.F., Marsch S.C., Schneider M., et al. Vasovagal heart block following cataract surgery under local anesthesia. Ophthalmic Surg. 1993;24(6):422.
23. Chong J.L., Tan S.H. Oculocardiac reflex in strabismus surgery—a study of singapore patients under general anesthesia. Singapore Med J. 1990;31(1):38.
24. Grover V.K., Bhardwaj N., Shobana N., et al. Oculocardiac reflex during retinal surgery using peribulbar block and nitrous narcotic anesthesia. Ophthalmic Surg Lasers. 1998;29(3):207. (abstract)
25. Warwick R. Representation of the extraocular muscles in the oculomotor nucleus of the monkey. J Comp Neurol. 1953;98:449.
26. Warwick R. Oculomotor organization. In: Bender M.B., editor. The oculomotor system. New York: Harper & Row; 1964:173.
27. Castro O., Johnson L.N., Mamourian A.C. Isolated inferior oblique paresis from brain stem infarction. Arch Neurol. 1990;47:235.
28. Brazis P.W. Localization of lesions of the oculomotor nerve: recent concepts. Mayo Clin Proc. 1991;66(10):1029.
29. Bienfans D.C. Crossing axons in the third nerve nucleus. Invest Ophthalmol. 1975;12:927.
30. Marinkovic S., Marinkovic Z., Filipovic B. The oculomotor nuclear complex in humans: microanatomy and clinical significance. Neurology. 1989;38(2):135.
31. Jampel R.S., Mindel J. The nucleus for accommodation in the midbrain of the macaque. Invest Ophthalmol. 1967;6:40.
32. Brazis P.W. Isolated palsies of cranial nerves III, IV, and VI. Semin Neurol. 2009;29:14-28.
33. Sacks J.G. Peripheral innervation of the extraocular muscles. Am J Ophthalmol. 1983;95:520.
34. Krewson W. Comparison of the oblique extraocular muscles. Arch Ophthalmol. 1944;32:204.
35. Reeh M.J., Wobig J.L., Wirtschafter J.D. Ophthalmic anatomy. San Francisco: American Academy of Ophthalmology; 1981. p 75
36. Müri R.M., Chermann J.F., Cohen L., et al. Ocular motor consequences of damage to the abducens area in humans. J Neuroophthalmol. 1996;16(3):191.
37. Umansky F., Valarezo A., Elidan J. The microsurgical anatomy of the abducens nerve in its intracranial course. J Neurosurg. 1991;75(2):294.
38. Romero F.R., Ramos J.G., Chaddad-Neto F., et al. Microsurgical anatomy and injuries of the abducens nerve. Arq Neuropsiquiatr. 2009;67:96-101.
39. Monkhouse W.S. The anatomy of the facial nerve. Ear Nose Throat J. 1990;69:677.
40. Proctor B. The anatomy of the facial nerve. Otolaryngol Clin North Am. 1991;24:479.
41. Chi S.L., Bhatti M.T. The diagnostic dilemma of neuro-imaging in acute isolated sixth nerve palsy. Curr Opin Ophthalmol. 2009;20:423-426.
42. Rush J.A., Younge B.R. Paralysis of cranial nerves III, IV, and VI. Arch Ophthalmol. 1981;99:76.
43. Tiffin P.A., MacEwen C.J., Craig E.A., et al. Acquired palsy of the oculomotor, trochlear, and abducens nerves. Eye. 1996;10:377.
44. Eskridge J.B. Evaluation and diagnosis of incomitant ocular deviations. J Am Optom Assoc. 1989;60(5):375.
45. Rubin M.M. Trochlear nerve palsy simulating an orbital blowout fracture. J Oral Maxillofac Surg. 1992;50:1238.
46. Troost B.T., Glaser J.S. Aneurysms, arteriovenous communications and related vascular malformations. In: Glaser J.S., editor. Neuro-ophthalmology. Hagerstown, Md: Harper & Row; 1978:319.
47. Jampel R.S. Ocular torsion and the function of the vertical extraocular muscles. Am J Ophthalmol. 1975;79:292.
48. Adams M.E., Linn J., Yousry I. Pathology of the ocular motor nerves III, IV, and VI. Neuroimaging Clin North Am. 2008;18:261-282.
49. Goldstein J.E., Cogan D.G. Diabetic ophthalmoplegia with special reference to the pupil. Arch Ophthalmol. 1960;64:592.
50. Gray L.G. A clinical guide to third nerve palsy. Opt J Rev Optom. 1994;1:86.
51. Ing E.B., Leavitt J.A., Younge B.R. Incidence of pupillary involvement in ischemic oculomotor nerve palsies. Ann Ophthalmol. 2000;32(2):90.
52. Burger L.J., Kalvin N.H., Smith J.L. Acquired lesions of the fourth cranial nerve. Brain. 1970;93:567.
53. Young B.R., Sutla F. Analysis of trochlear nerve palsies: diagnosis, etiology, and treatment. Mayo Clin Proc. 1977;52:11.
54. Gunderson C.A., Maxow M.L., Avilla C.W. Epidemiology of CN IV palsies. Am J Orthop. 2001;51:99.
55. Galetta S.L., Smith J.L. Chronic isolated sixth nerve palsies. Arch Neurol. 1989;46:79.