CHAPTER 10 Continuous Passive Motion
INTRODUCTION
In 1960, Salter and Field16 showed that immobilization of a rabbit knee joint under continuous compression, provided by either a compression device or forced position, resulted in pressure necrosis of cartilage. In 1965, Salter and colleagues17 reported the deleterious effects of immobilization on the articular cartilage of rabbit knee joints and the resultant lesion that they termed obliterative degeneration of articular cartilage. Salter15 believed that, “The relative place of rest and of motion is considerably less controversial on the basis of experimental investigation than on the basis of clinical empiricism.” He reasoned that because immobilization is obviously unhealthy for joints, and if intermittent movement is healthier for both normal and injured joints, then perhaps continuous motion would be even better. Because of the fatigability of skeletal muscle, and because a patient could not be expected to move his or her own joint constantly, he concluded that for motion to be continuous, it would also have to be passive. Thus, he invented the concept of continuous passive motion, which has come to be known as simply CPM. Salter also believed that CPM would have an added advantage; namely, that if the movement was reasonably slow, it should be possible to apply it immediately after injury or operation without causing the patient undue pain.
PRINCIPLES OF USE
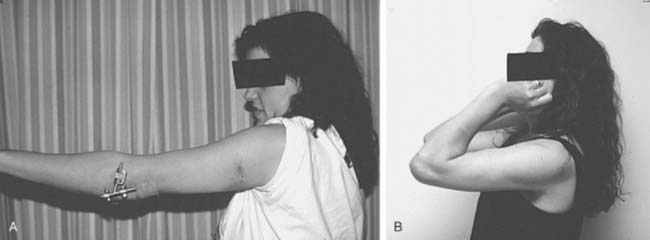
Once CPM is started, it is optimal that the full potential range of motion of that specific joint be used (Fig. 10-1A and B). Essentially, the tissues are being squeezed alternately in flexion and extension. CPM causes a sinusoidal oscillation in hydraulic pressure within and around the joint.2,9 This not only rids them of excess blood and fluid but prevents further edema from accumulating.8 In the first 24 hours, swelling can develop in minutes (due to bleeding), so CPM should be virtually continuous. This has a beneficial effect on healing soft tissues similar to that seen with compressive therapy after eccentric muscle injury.6 Bathroom privileges are allowed, and the patient is instructed to come out of the CPM device once every hour for 5 minutes. This safety precaution is to reduce the risk of a pressure or stretch related nerve palsy. As the number of days following surgery increases, the amount of time required for swelling to develop increases also, so that longer periods out of the machine are permitted.
CPM requires close supervision by someone skilled with its use, so it is mandatory that the patient and family are involved and educated from the beginning regarding the principles of use and how to monitor the limb. Frequent checking and slight adjustments of position prevent pressure-related problems. The arm tends to slip out of the machine, so it must frequently be pulled back into it. Nurses do not always have sufficient time, or sometimes the experience, to look after these needs. The patients and their families develop a keen sense of responsibility very quickly and become an invaluable asset. A preoperative instructional video is useful to educate them and should be watched again postoperatively.
PAIN CONTROL
We favor the use of an indwelling catheter for continuous brachial plexus block anesthesia (see Fig. 10-1C).13–17 This permits a range from analgesia to anesthesia by varying the dose of bupivacaine, a long-acting local anesthetic. The initial bolus dose may be sufficient to cause a complete or near-complete motor and sensory block. Motor blockade requires splinting of the wrist to protect it. Moderate or complete anesthesia, as opposed to analgesia with minimal anesthesia, requires careful attention to the status of the limb overall, because the patient’s protective pain response is no longer present. Insidious development of a nerve palsy during CPM may be less likely to go unnoticed if some motor and sensory function are still present in each nerve during CPM.
ADVANTAGES
There are a number of advantages to the use of CPM. Most surgeons are aware from the total knee experience that analgesic consumption is diminished because the patients are more comfortable (although not always during the first day or two). Swelling is diminished.
Although most experience with CPM has been in the knees, several studies have documented the efficacy of CPM for the elbow.1,5,11,12 In two separate studies, postoperative CPM was found to improve elbow motion following open reduction internal fixation (ORIF) of distal humeral fractures in children and adolescents.11,12 CPM has been also documented to be effective in assisting with restoration of elbow motion after surgical release1 or resection of heterotopic ossification.5
My personal experience using CPM in strict accordance with the principles just outlined has convinced me that motion is obtained faster and more completely than that obtained without the use of CPM, despite the studies that failed to show such a benefit in the knee (Fig. 10-2A and B).7,8,18,19 This can be explained on the basis of how CPM has been routinely used. Typical protocols involve starting with a small range of motion tolerated by the patient, for example 30 degrees, and gradually increasing the range each day. This pattern of use is not in compliance with the essential principles of CPM. What such a protocol does is to increase swelling and bleeding due to constant tissue irritation.
COMPLICATIONS
I do not generally use CPM in the presence of ligament injuries or potential joint instability because it is not possible to keep the elbow perfectly aligned with the axis of rotation of the machine. Malalignment would stress the ligaments and bony stabilizers of the joint.
1 Aldridge J.M.3rd, Atkins T.A., Gunneson E.E., Urbaniak J.R. Anterior release of the elbow for extension loss. J. Bone Joint Surg. Am.. 2004;86A:1955.
2 Breen T.F., Gelberman R.H., Ackerman G.N. Elbow flexion contractures: Treatment by anterior release and continuous passive motion. J. Hand Surg. Br. 1988;13-B:286.
3 Brown A.R., Weiss R., Greenberg C., Flatow E.L., Bigliani L.U. Interscalene block for shoulder arthroscopy: comparison with general anesthesia. Arthroscopy. 1993;9:295.
4 Gaumann D.M., Lennon R.L., Wedel D.J. Continuous axillary block for postoperative pain management. Reg. Anesth. 1988;13:77.
5 Ippolito E., Formisano R., Caterini R., Farsetti P., Penta F. Resection of elbow ossification and continous passive motion in postcomatose patients. J. Hand Surg. Am. 1999;24:546-553.
6 Kraemer W.J., Bush J.A., Wickham R.B., Denegar C.R., Gomez A.L., Gotshalk L.A., Duncan N.D., Volek J.S., Putukian M., Sebastianelli W.J. Influence of compression therapy on symptoms following soft tissue injury from maximal eccentric exercise. J. Orthop. Sports Phys. Ther. 2001;31:282.
7 O’Driscoll S.W., Giori N.J. Continuous passive motion (CPM): Theory and principles of clinical application. J. Rehabil. Res. Dev. 2000;37:179.
8 O’Driscoll S.W., Kumar A., Salter R.B. The effect of continuous passive motion on the clearance of a hemarthrosis from a synovial joint: an experimental investigation in the rabbit. Clin. Orthop. 1983;176:305.
9 O’Driscoll S.W., Kumar A., Salter R.B. The effect of the volume of effusion, joint position and continuous passive motion on intra-articular pressure in the rabbit knee. J. Rheumatol. 1983;10:360.
10 Pope R.O., Corcoran S., McCaul K., Howie D.W. Continuous passive motion after primary total knee arthroplasty. J. Bone Joint Surg. Br. 1997;79:914.
11 Remia L.F., Richards K., Waters P.M. The Bryan-Morrey triceps-sparing approach to open reduction of T-condylohumeral fractures in adolescents: Cybex evaluation of triceps function and elbow motion. J. Pediatr. Orthop. 2004;24:615.
12 Re P.R., Waters P.M., Hreski T. T-condylar fractures of the distal humerus in children and adolescents. J. Pediatr. Orthop. 1999;19:313.
13 Salter R.B. Motion vs. rest. Why immobilize joints? J. Bone Joint Surg. 1982;64-B:251.
14 Romness D.W., Rand J.A. The role of continuous passive motion following total knee arthroplasty. Clin. Orthop.. 1988;226:34.
15 Salter R.B. Motion vs. rest. Why immobilize joints? J. Bone Joint Surg. 1982;64-B:251.
16 Salter R.B., Field P. The effects of continuous compression on living articular cartilage. An experimental investigation. J. Bone Joint Surg. 1960;42-A:31.
17 Salter, R. B., McNeill, O. R., and Carbin, R.: The pathological changes in articular cartilage associated with persistent joint deformity. An experimental investigation. Studies of the rheumatoid diseases. Third Canadian Conference on Research in Rheumatic Diseases. Toronto, 1965, p. 33.
18 Schroeder L.E., Horlocker T.T., Schroeder D.R. The efficacy of axillary block for surgical procedures about the elbow. Anesth. Analg. 1996;83:747.
19 Stinson L.J., Lennon R., Adams R., Morrey B. The technique and efficacy of axillary catheter analgesia as an adjunct to distraction elbow arthroplasty: a prospective study. J. Shoulder Elbow Surg. 1993;2:182.