CHAPTER 7 Conditions of the Reproductive Organs
UTERINE FIBROIDS
Uterine fibroids (properly called leiomyomata or myomas) are solid, well-defined benign monoclonal tumors of the smooth muscle cells of the uterus (Fig. 7-1).1,2 They range in size from microscopic to many pounds in weight, and may be singular or clustered. Multiple myomas in the same uterus are not clonally related.3 Fibroid size is described in comparison to a pregnant uterus (i.e., a fibroid the size of a 16-week pregnancy). As many as 20% to 40% of all women develop fibroids by age 40.1 Approximately 17% of all hysterectomies performed in the United States are for uterine myomas, with a peak incidence of surgery occurring for women around age 45, making fibroids the primary annual cause of premenopausal hysterectomy in the United States.3,4 They are rare in a premenarchal young women and shrinkage typically occurs in post-menopausal women with the natural decline in estrogen levels, unless stimulated by exogenous estrogen (foreign estrogens usually a result of environmental exposure, for example, from pesticides or plastics).1 For unknown reasons, fibroids are two to three times more common in black women than white, Asian, and Hispanic women.1,3 Fibroids are classified according to their site of growth in the uterine or surrounding tissue as submucosal, intramural, and subserous (see Figure 7-1). They also may occur in the cervix (cervical fibroids), between the uterine broad ligaments (interligamentous fibroids), or they may be attached to a stalk (pedunculated fibroids) and protrude into the uterine cavity (pedunculated submucosal fibroids) or through the cervix.1,3
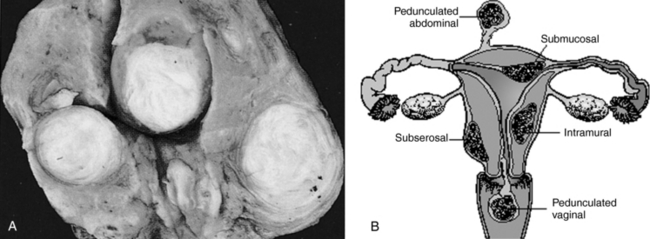
Figure 7-1 Uterine fibroids.
Salvo S: Mosby’s Pathology for Massage Therapists, St. Louis, 2004, Mosby.
The exact etiology of uterine fibroids remains undetermined.5 Leiomyomas are hormone dependent. This is evidenced by the fact that they develop during hormonally active years and decline during menopause, fibroid tissue has an increased number of estrogen and progesterone receptors, fibroid tissue is hyperestrogenic, hypersensitive to estrogen, and does not possess the normal regulatory mechanism that limits estrogen response, the peak mitotic activity occurs during the luteal phase, and they respond to treatment with gonadotropin-releasing hormone (GnRH) agonists.3, 6 7 8 Growth factor also plays a role in leiomyomata development.3,9 As estrogen and progesterone levels rise, insulin is released causing the transient hypoglycemia commonly experienced premenstrually. When plasma glucose levels fall, pituitary growth hormone is released, exerting bodywide effects. Its action on hepatocytes causes the release of insulin-like growth factors (IGFs). In a study by Vollenhoven et al., it is postulated that the net effect of these changes increases the bioavailability of free (bioactive) IGF, which may play a major role in promoting fibroid growth.9 A further study by De Leo and Morgante states that concentrations of epidermal growth factor, insulin-like growth factor 1 (IGF 1), and platelet-derived growth factor (PDGF AB) are present in myomatous tissues together with their receptors.6 Prolactin also may be a factor. Leiomyomata express a number of hormones, including parathyroid hormone–related protein (a growth factor), prolactin, and IGF.3
Factors that might increase fibroid development and growth include:
The use of oral contraceptives is not associated with any changes in fibroid size, and may even be protective; however, one study reported a slight increase in risk with a history of OC use beginning in the early teenage years. 2 3 4
PATHOPHYSIOLOGY
Myoma risk is inversely related to increasing parity and age at last pregnancy, and is decreased by smoking (due to its inhibition of estrogen) and increased by obesity (likely due to increased estrogen levels) and hypertension. 1 2 3,10 Fibroids occur in 1% to 2% of pregnancies. However, it is uncertain whether this relationship is entirely causal. Infertility, as well as early pregnancy loss, may be due to mechanical obstruction of implantation or distortion of the cervix or endometrium. Once a pregnancy is established, it is rare for myomata to interfere with its progress, and most proceed uncomplicated. However, a higher rate of cesarean section has been noted, and premature labor may result from very large myomata.1 Degeneration of fibroids, caused by hemorrhagic infarction, may rarely occur during late pregnancy and is marked by pain, and also may be accompanied by rebound tenderness, fever, nausea, vomiting, and leukocytosis.3 Treatment consists of rest and analgesia; surgery is a last resort.
Anemia and fatigue can be caused by excessive blood loss associated with fibroids. Pressure on the bowel or bladder can cause constipation, urinary frequency, and dyspareunia. Large fibroids may mask the diagnosis of serious gynecologic neoplasm. Rapidly growing fibroids may indicate a more serious pathology such as leiosarcoma and should be investigated. Malignancy is rarely associated with uterine fibroids; however, they occur with increased frequency in endometrial hyperplasia and are associated with a fourfold increased risk of developing endometrial cancer.1
SYMPTOMS
Most women with myomas are asymptomatic, never knowing that they have them unless informed of such by gynecologic examination. This was actually discovered based on ultrasound and autopsy results revealing that many more women had fibroids than had ever been diagnosed or treated for symptoms.2 The most common symptoms are menorrhagia and the physical effects caused by large myomata such as increased pelvic pressure, frequent urination, difficulty with defecation, and dyspareunia with deep penetration.1,3,5 Abnormal uterine bleeding is present in about 30% of all patients, and periods are typically heavy and prolonged, often with premenstrual and postmenstrual spotting.2,4 Uterine bleeding caused by myomas can be associated with significant social, emotional, financial, and medical difficulties; women’s concerns should be addressed. Some women experience dysmenorrhea.2 Metrorrhagia, may occur, but should be evaluated with an endometrial biopsy to rule out other endometrial disease.4 About 2% to 10% of women experience infertility as a result of fibroids, ostensibly due to abnormal uterine of tubal motility, interference with sperm movements, or abnormal uterine blood flow.3,11 Fibroid degeneration, torsion, or compression of a nerve against the pelvis caused by encroachment by a fibroid can lead to significant pain.4,11
DIAGNOSIS
Diagnosis can be determined by:
CONVENTIONAL TREATMENT
Unless fibroids are symptomatic, observation is the most prudent form of treatment and no other intervention is necessary.1,4 GnRH agonists (e.g., Leuprolide) have been used effectively to control symptoms and reduce myoma size through suppression of estrogen and progesterone production.3,12 Mean uterine size decreases 30% to 64% after 3 to 6 months of treatment, and symptoms associated with fibroids are alleviated as a result. Possible side effects include hot flashes, headache, vaginal dryness and vaginitis, decreased libido, joint and muscle stiffness, and depression, and 30% of patients continue to have light, irregular vaginal bleeding.3,12 Local allergic reaction occurs in about 10% of patients.3 Bone loss occurs but is reversible, and a small number of women (2%) experience major vaginal hemorrhage 5 to 10 weeks after treatment commences. Steroid add-back therapy has been investigated to prevent bone loss in women requiring long-term GnRH therapy; however, because of the risk of osteoporosis, long-term therapy is inadvisable.3,12
Surgery should be reserved for women who are past childbearing, who are heavily symptomatic and not responsive to drug therapy, or who have suspected malignancies. Women wanting to preserve childbearing ability should be given the option of conservative therapy. GnRH therapy may be prescribed as pretreatment for surgical procedures to reduce fibroid size and bleeding. Myomectomy may be performed vaginally, hysteroscopically, or laparoscopically, and when performed skillfully, improves symptoms in 80% to 90% of patients. Between 15% and 30% experience fibroid regrowth after 5 years. Uterine scarring may occur from the procedure and affect fertility.12 Endometrial ablation and uterine artery embolization (UAE) are additional options.13,14 UAE is increasingly popular, and appears generally safe, but it is uncertain how long the treatment lasts and whether future fertility may be affected. The procedure involves injection of polyvinyl or gelatin particles into the uterine arteries to cut off blood supply to the fibroids, which leads to shrinkage over the next 3 to 12 months. Approximately 85% of patients gain relief from the procedure, which has been performed since 1995. However, it is not risk free. Adverse outcomes include infection, bleeding, and formation of emboli, as well as future fertility problems. For women intending to become pregnant in the future, myomectomy may still be the most certain conventional surgical intervention.14 Hysterectomy is generally recommended when women are past childbearing age, are symptomatic, malignancy is suspected, or if other therapies are ineffective.1,3,12
BOTANICAL TREATMENT
Among Western herbalists specializing in gynecologic complaints, there is a common perception that although symptoms of uterine fibroids are not difficult to control with botanical medicines, and their growth can be arrested, they are difficult to eliminate entirely unless the fibroid is small at the onset of treatment (smaller than 12-week size). Many women are content to have symptom control over pharmaceutical or surgical intervention, as long as the fibroids present no mechanical problems.15 Traditional Chinese medicine (TCM) has clearly defined diagnostic constructs, many herbal formulae, and well-developed adjunctive treatment protocols (e.g., acupuncture, moxibustion) for treating uterine fibroids and has claimed success in entirely eliminating uterine fibroids.
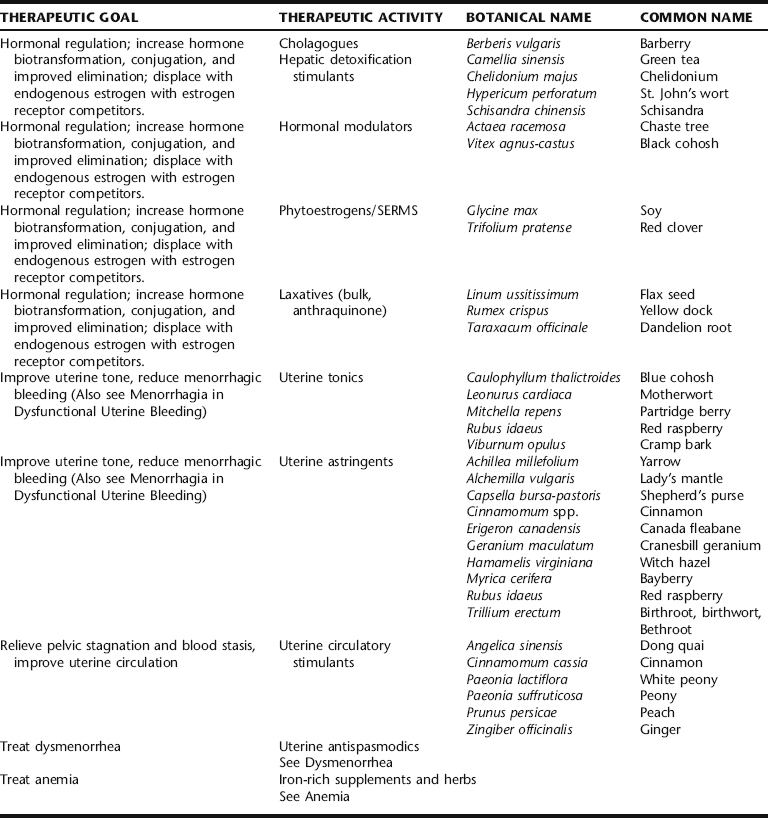
Western herbal treatment protocols include a variety of strategies (Table 7-1). These include weight reduction, promoting hormonal balance, specifically through the elimination of estrogens by enhancing liver detoxification mechanisms, promoting pelvic circulation while simultaneously controlling bleeding if necessary, and general improvement of uterine tone. These are integrated with the general recommendation to avoid excess exposure to xenoestrogens (environmental estrogens) and reduce overall estrogen levels, exposure to both being a risk factor for the development of uterine fibroids. Women with fibroids report greater frequency of red meat and pork intake, and less frequent green vegetable, fruit, and fish consumption.4 Although there is little correlation between the development of uterine fibroids and cancer, numerous studies have demonstrated a connection between diet, estrogen levels, and hormone-dependent cancers, as well as a protective effect of fruit and vegetables against cancer.4 No studies have evaluated the effects of US dairy consumption and the development of uterine fibroids. However, an association between dairy intake and increased risk of ovarian cancer has been reported.16,17 Herbalists recommend that patients avoid foods that increase risk, and emphasize intake of those shown to facilitate estrogen biotransformation, for example, by increasing dietary fiber, and regular intake of complex carbohydrates as found in vegetables and grains.11,18,19 Botanical strategies are aimed at reducing the estrogen burden through liver detoxification and improved elimination, promoting gynecologic health in general by improving pelvic circulation, reducing symptoms, and controlling fibroid size.
TCM treatment for fibroids has been evaluated through several preliminary studies, which are presented in the following section. Western botanical protocol for the treatment of uterine fibroids has not been subjected to controlled trials.4 The Western botanical information presented in this chapter reflects the opinions of herbalists practicing in the United States, United Kingdom, Canada, Australia, and New Zealand, regarding the efficacy and safety of the primary herbs used to treat myomas. Given the general safety of the botanicals being discussed, and the lack of noninvasive long-term effective medical treatments for fibroids, it seems that investigation of the primary Western herbal protocols cited in Table 7-1 is warranted. Nervines, laxatives, adaptogens, and other herbs included in fibroid protocol are discussed elsewhere throughout this text. Stress reduction should not be overlooked as part of the treatment protocol for women with symptomatic fibroids, as chronic uterine bleeding can cause emotional, social, financial, and medical consequences.2
Traditional Chinese Medicine Treatment
Cinnamon and Peony
Traditional Chinese medicine has numerous well-developed treatment protocols and formulations, some of which have been used for several centuries for promoting gynecologic health in general and for treating uterine fibroids specifically. For a more comprehensive review of the Chinese treatments for gynecologic problems, readers are referred to the primary TCM literature. Generally speaking, TCM views uterine myomas as a result of poor circulation of chi (energy) and blood through the pelvic region. Many formulas are designed to dispel pelvic stagnation and increase the flow of blood to uterine and ovarian tissues and facilitate the smooth flow of blood via menses. A classic TCM formula used for relieving blood stagnation is Cinnamon Twig and Poria Pill (gui zhi fu ling wan) consisting of: Cinnamomum aromaticum twigs, Poria cocos, Paeonia lactiflora root, Paeonia suffruticosa root, and Prunus persica seed. It should also be noted that in TCM, each herbal formula has specific diagnostic criteria for which it is used as well as clear contraindications and cautions. For maximum efficacy in using TCM protocols, a qualified herbal TCM practitioner should be consulted. In addition to herbal protocol for promoting gynecologic health and specifically treating uterine fibroids, TCM also employs numerous other modalities, which may include walking to promote circulation in general and abdominal circulation specifically, moxibustion, acupuncture, external application of compresses, and other such adjunctive therapies. Specific lifestyle recommendations also can be given such as the avoidance of cold foods and drink (in TCM coldness is said to cause congealment and stagnation) and constrictive clothing.20
Several studies have looked at the efficacy of the Cinnamon Twig and Poria Pill formula noted in the preceding section for the treatment of uterine fibroids. Specifically, the studies investigated the effectiveness of the Japanese version of this formula (Keishi-bukuryo-gan, KBG) in an open study on 110 premenopausal women with symptomatic uterine fibroids measuring less than 10 cm in diameter. They were treated with 22.5 g/day of a freeze-dried decoction of the herbs for 12 weeks. Twenty-one women were considered “normal” and 47 women much improved by the end of the trial. This herbal formula is frequently used to treat a range of gynecologic disorders including dysmenorrhea, cervical erosion, ovarian cysts, chronic salpingitis, and endometriosis, to name a few conditions.15 There is research to suggest that the Paeonia species in this formula may act as an LH-releasing hormone (LH-RH) antagonist with weakly antiestrogenic effects in the presence of estrogen.21 In another study, the authors applied individualized TCM formulations and treatments to treat 223 cases of uterine fibroids with a reported 72% reduction of menorrhagia in 160 women complaining of this symptom, 58% improvement in backache, and an overall effectiveness rate of 92.4%. Myomas were eliminated in 29 of 223 patients and markedly diminished in 42 patients. In 32 patients, no changes were seen and there were no positive results in 12.5% of patients.15 If the TCM treatments were tailored to the individual patients, then this can be kept with the addition I made. If the treatment was specific, a similar level of detail as the previously reported study should be given for consistency of presentation.
In an interesting study by Mehl-Madrona et al., an integrated TCM-Western medicine pilot study was conducted to compare the cost and efficacy of a set of therapies typically used by CAM practitioners and conventional medicine on ability to reduce uterine fibroid size. All patients were premenopausal and age 24 to 45 years, educated, employed, and from a socioeconomic bracket that allowed them to pay cash for all treatments. None were on pharmaceutical treatment or hormonal contraceptives at the time of the study and all received a pelvic ultrasound before and again 6 months after treatment. Sonograms were obtained on patients who dropped out of the study as well, so sonograms were available on all patients. Uterine fibroids measured at least 6- to 8-week pregnancy size, with palpable fibroids 2 to 3 cm in diameter. Inclusion in the study required hemoglobin greater than 8 g/dL, with fibroid growth of less than 6 cm/year. CAM treatment included a combination of nutritional, herbal, acupuncture, bodywork, and psychological interventions. Acupuncture and herbal protocols were selected individually for the patient, using formulae and points traditionally indicated for the patient’s patterns: symptoms, constitution (based on TCM pulse and tongue diagnosis), and condition. The comparison group used progestational agents, oral contraceptives, and NSAIDs. The results of this study demonstrated no statistically significant difference in change of symptoms between the two groups when measured after 6 months of treatment. Both experienced improvement in symptoms and fibroid size. Patients in the treatment group considered the pilot study a success because they were able to achieve results equivalent to pharmaceutical interventions using nonconventional methods.15
Hormonal Modulators
Chaste Berry
Chaste berry is the primary herb employed by herbalists and integrative medicine practitioners for hormonal modulation in the botanical treatment of fibroids.4,22 It acts as a dopamine agonist, resulting in a reduction in prolactin release.23 Prolactin may play a role in fibroid growth. No scientific evidence in the literature has been found for the use of chaste berry specifically in the treatment of fibroids, and although its use may result in reduction of apparent estrogen excess due to relative progesterone deficiency, increased progesterone levels have been shown to result in increased mitotic division in fibroid tissue. Wuttke et al. studied the putative estrogenic effects of a chaste berry extract and found it contained substances that replaced radiolabeled estradiol from a cytosolic estrogen receptor preparation, and appeared to be agonistic to ERβ. However, because the uterus expresses ERα, no effects on the uterine expression of estrogen were expected or have been experimentally observed.23
Phytoestrogens and Selective Estrogen Receptor Modules
Phytoestrogens are plant compounds with a similar molecular shape and structure to endogenous estrogen molecules, and which can bind competitively to estrogen receptors, preventing the binding of more potent estrogen and estrogen metabolites (see Part IV).24 They appear to behave similarly to selective estrogen receptor modulators (SERMs). Low Dog explains their potential clinical application in conditions of estrogen excess, in relationship to the role of phytoestrogens in breast cancer treatment:
By binding to estrogen receptors in the premenopausal woman, phytoestrogens “turn down” estrogen production through negative feedback at the level of the hypothalamus and pituitary gland…when endogenous estrogen levels are high, phytoestrogens may have an antiestrogenic activity by preventing estrogen from binding to the estrogen receptor through competitive inhibition.25
Legumes, including soybeans and red clover, are rich in phytoestrogens.26 In a study by Liu et al. methanol extracts of red clover (Trifolium pratense), chaste berry, and hops (Humulus lupulus) showed significant competitive binging to both ERα and ERβ. In the same study, dong quai (Angelica sinensis) and licorice (Glycyrrhiza uralensis) showed weak ER binding, whereas black cohosh did not exhibit any competitive binding. Controversy abounds as to the mechanisms of action of black cohosh, which do not appear to be directly phytoestrogenic.27 Current research is suggesting a dopaminergic or serotonergic effect for this botanical.25,27 The application of phytoestrogens may be a promising area for further investigation for the botanical treatment of fibroids, and should be considered in the development of botanical protocols.
Hormone Excretion and Biotransformation
Greater than 50% of all estrogen metabolism and conjugation occurs in the liver, suggesting a basis for the belief among herbalists that herbs that improve liver function may increase estrogen excretion and either treat or lower the risk for uterine fibroids.4,22 Herbalists commonly include liver-specific herbs in formulae for treating fibroids. Several herbs actively effect phase 1 and phase 2 liver detoxification systems and CYP450, an enzyme system partially involved in the metabolism of estrogen. These effects and their relationship to uterine fibroid treatment, if any, have not been formally investigated but are often applied by modern herbal practitioners in putatively reducing estrogen burdens. Cholagogues, herbs which stimulate the release of bile from the gallbladder, also may be useful for clearing estrogen through increased bowel clearance resulting from their indirect laxative action. Examples of cholagogues include bayberry and chelidonium.22
Uterine Tonics, Astringents, and Hemostatics
Because bleeding is a common symptom of uterine fibroids, numerous antihemorrhagic herbs are used in botanical medicine protocols (see Menorrhagia in Dysfunctional Uterine Bleeding).22 Yarrow dried plant infusion is perhaps one of the most widely used uterine antihemorrhagics, reliably reducing acute uterine bleeding, but conversely promoting menstrual flow when suppressed. It has been used since ancient times as a styptic.25 Either dry or fresh plant can be used as a tea or tincture. Many herbalists believe that yarrow herb taken as tea is more quickly effective for stopping acute uterine bleeding than other preparations. Other traditionally used uterine antihemorrhagic herbs include lady’s mantle, shepherd’s purse (fresh only), cranesbill geranium, witch hazel, bayberry, red raspberry, and bethroot. These are all generally
| Yarrow | (Achillea millefolium) | 40 mL |
| Lady’s mantle | (Alchemilla vulgaris) | 20 mL |
| Bayberry bark | (Myrica cerifera) | 15 mL |
| Shepherd’s purse | (Capsella bursa-pastoris) | 15 mL |
| Cinnamon | (Cinnamomum cassia) | 10 mL |
| Total: 100 mL | ||
taken in tincture form in 2- to 4-mL doses repeated every 15 minutes as needed until bleeding subsides, or combined into larger formulae for the treatment or prevention of chronic menorrhagia. Shepherd’s purse in particular has been used traditionally as a uterine antihemorrhagic. The 1986 Commission E monograph recommends daily oral doses of 10 to 15 g of crude herb (or equivalent in extract) for mild gynecologic bleeding.28 Extracts of the drug contain a hemostyptic action, likely owing to the presence of a peptide that has demonstrated oxytocin-like activity in vitro.28,29 Many modern Western herbalists believe that it is imperative to prepare Shepherd’s purse from fresh, not dry, plant material. Lady’s mantle’s mechanism of action lies in its high tannin content, indicating it for bleeding, diarrhea, and wound healing, a likely mechanism for many of the other herbs used as uterine antihemorrhagics.29 The combination of Cinnamomum and Erigeron was relied upon by the Eclectics for uterine hemorrhage, and is still employed by midwives today for the treatment of nonemergency postpartum bleeding, and by herbalists for the treatment of menorrhagia.30,31 Red raspberry leaf is typically used more as a long-term uterine tonic than to arrest acute bleeding. Blue cohosh has been used historically for its utero-tonic actions. It is listed in the 1918 US Dispensatory for the treatment of menorrhagia and dysmenorrhea, and is still widely used by herbalists for these conditions.32
Relieving Uterine Stasis: Circulatory Stimulants
Improving pelvic circulation and relieving stasis is a common approach to fibroid treatment in both Western and traditional Chinese herbal medicine, based on the belief that relieving stagnation and congestion in the pelvis will facilitate the removal of “blockages” and growths (e.g., fibroid tissues), remove wastes, and promote greater health and nourishment of the pelvic organs in general.11,18,20 Decreasing pelvic stagnation is also thought to help reduce uterine hemorrhage. Ginger and cinnamon are both traditionally used to increase circulation to the reproductive organs. Further, cinnamon has been used historically to reduce uterine bleeding, making it specific for the treatment of uterine fibroids with menorrhagia or metrorrhagia.30,31 White peony, an ingredient in Keishi-bukuryo-gan, discussed in the preceding, is a common herb used in TCM for the treatment of women’s disorders, including menstrual dysfunction and uterine bleeding.33 Red peony is often combined with white peony and peach seed to dispel blood stasis, and conditions associated with it, including excessive uterine bleeding, particularly with the presence of thick, purple clots.33
Treatment Protocol
| Lady’s mantle | (Alchemilla vulgaris) | 25 mL |
| Raspberry | (Rubus idaeus) | 30 mL |
| Nettles | (Urtica dioica) | 20 mL |
| White peony | (Paeonia lactiflora) | 15 mL |
| Ginger | (Zingiber officinalis) | 10 mL |
| Total: 100 mL |
After 3 months the above protocol was modified to:
| Red raspberry leaf | (Rubus idaeus) | 40 mL |
| White peony | (Paeonia lactiflora) | 40 mL |
| False unicorn | (Chamaelirium luteum) | 15 mL |
| Ginger | (Zingiber officinalis) | 5 mL |
| Total: 100 mL |
| Ashwagandha | (Withania somnifera) | 40 mL |
| Lemon Balm | (Melissa officinalis) | 30 mL |
| Hops | (Humulus lupulus) | 15 mL |
| Valerian | (Valeriana officinalis) | 15 mL |
| Total: 100 mL |
NUTRITIONAL CONSIDERATIONS
Xenoestrogens/Endocrine Disruptors
Avoid xenoestrogen ingestion from pesticide and herbicide residue by eating organically cultivated foods and avoiding foods in plastic containers. Xenoestrogens are found most concentrated in the fat of meat, farmed fish, and nonorganic dairy products.12 Eating primarily organic meat, dairy, and produce, washing fruits and vegetables thoroughly before eating, and minimizing the use of soft plastics, such as for food storage, can help reduce xenoestrogen intake.
Estrogen Biotransformation and Diet
Metabolism and detoxification of estrogen in the body ultimately determines its biological effects. Estrogen biotransformation occurs mainly in the liver through phase I hydroxylation and phase II methylation and glucuronidation, allowing estrogen to become a water-soluble, excretable compound.11 This is predominantly excreted by the liver in bile (see Dietary Fiber). Phase I detoxification yields three estrogen metabolites with highly variable biological activity: 2-hydroxyestrone (2-HE), 16-alpha-hydroxyestrone (16α-HE), and 4-hydroxyestrone (4-HE). 2-HE is a beneficial estrogen metabolite in that among its effects, it competitively binds estrogen sites, blocking more potent estrogens. Conversely, 4-HE and 16α-HE are potent estrogens that may promote the growth of estrogen-sensitive tissue.11 Dietary consumption of cruciferous vegetables, such as broccoli and cabbage, as well as green tea, garlic, and rosemary can increase the amount of 2-HE by modifying P450 activity in phase I, and have antioxidant effects as well.11,34
Dietary Fiber
Once estrogen metabolites are excreted by the liver in bile, the metabolites are soaked up by fiber in the small intestines and excreted via defecation. If the diet lacks fiber, bile, along with the estrogen metabolites are reabsorbed, adding an unnecessary estrogen burden to the body. Soluble fiber such as the lignins found in flax seeds also increases sex hormone binding globulin (SHBG), decreasing the amount of available active estrogen, as estrogen bound to SHBG is rendered inactive.11 Brassicae vegetables such as cabbage and broccoli contain indole glucosinolates, which when chewed, are degraded by a plant enzyme into a variety of indole structures. When degraded in the body, these structures induce cytochrome P450 expression (CY1A1) in hepatic and extrahepatic tissue, leading to greater conversion of 2-hydroxyestrone (2-HE), and decreasing the availability of E1 for conversion to 16-HE, thereby reducing the estrogen burden overall.25 This is partly associated with the anticancer effects associated with these foods.
ADDITIONAL THERAPIES
Treatment Summary: Uterine Fibroids
What to expect with treatment
Eclectic Specific Condition Review: Uterine Fibroids—a Historical Perspective
stress. Herbalists often recommend specific yoga postures or Kegel exercises to assist in improving pelvic circulation particularly.35 Vigorous walking, hip circling, pelvic thrusts, and belly dancing can all be useful to improve pelvic circulation.
FIBROCYSTIC BREASTS AND BREAST PAIN
Benign breast conditions are a common finding in clinical practice, with fibrocystic breast changes and fibroadenomas occurring in 60% to 90% of all women.36 The hallmark of fibrocystic breast changes is that the cysts fluctuate in size and shape, may entirely disappear and reappear cyclically, and are associated with hormonal changes in the menstrual cycle. Women with this condition describe their breasts as feeling lumpy, “ropey,” and tender. The changes occur bilaterally. Fibroadenomas are mobile, solid, firm, rubbery masses that typically occur singly, and are not usually painful (Fig. 7-2). They are second only to fibrocystic changes as the most common of the benign breast conditions, and are commonly found in women in their 20s. Breast tenderness that accompanies the menstrual cycle is known as cystic mastalgia.38,39 Cyclic mastalgia may be associated with other premenstrual complaints. The terms benign breast disorder and benign breast disease are unfortunate misnomers, as they are neither a disorder nor disease. In only a small percentage of cases are the atypical ductal and lobular hyperplasias associated with increased risk of breast carcinoma. Practitioners consulting with women for fibrocystic breast changes and other findings must be sensitive to a patient’s increased anxiety about finding a breast lump, and provide clear information and calming reassurance both during the exam and while the patient awaits tests results if any were deemed necessary.
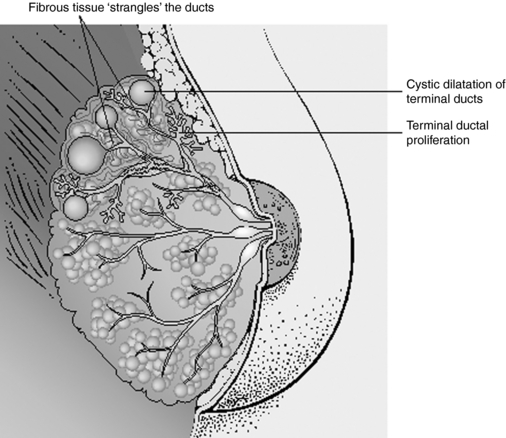
Figure 7-2 Comparison of normal and fibrocystic breast tissue.
Salvo S: Mosby’s Pathology for Massage Therapists, St. Louis, 2004, Mosby.
PATHOPHYSIOLOGY
Fibrocystic breast changes are an exaggerated response to cyclic ovarian hormones.39 The etiology of fibroadenomas and cyclic mastalgia may also be hormonal, though in some cases, the cause of a fibroadenoma may be unclear. When this occurs in women over 30, removal of the mass is generally recommended.
DIAGNOSIS AND DIFFERENTIAL DIAGNOSIS
There are two primary aims when arriving at a diagnosis of fibrocystic breasts. The first is to rule out breast cancer, and the second is to determine if benign breast symptoms warrant treatment. A careful history, physical exam, and cancer risk assessment are indicated (Box 7-1 and Table 7-2).36 A thorough breast exam is best performed after the menses, as examination prior to menses (when the pain is actually likely to be most acute) can obscure problematic lumps caused by normal breast tissue proliferation and nodularity from normal hormonal changes. If a suspicion of breast cancer remains after the history and physical, further diagnostic tests should be performed as appropriate.36 Diagnosis of fibrocystic breasts can be made on the basis of cancer exclusion. For women experiencing symptoms including pain, tenderness, swelling, inflammation, or nipple discharge, the comprehensive history and physical can be used to determine if the problem is cyclic or noncyclic in nature and whether it is associated with other signs and symptoms, including fever or premenstrual mood swings. It is also important to gently move aside the breast tissue and examine the chest wall and muscle to determine whether breast pain or muscle pain is the proper diagnosis.40 Depending on the associated signs and symptoms, a diagnosis, including breast infection, muscle sprain/strain, premenstrual syndrome, or noncyclic mastalgia can be determined.
TABLE 7-2 Risk for Development of Breast Cancer by Type of Benign Breast Disease
| HISTOLOGIC PATTERN | APPROXIMATE RELATIVE RISK OF DEVELOPING BREAST CARCINOMA | PROPORTION OF BENIGN LESIONS* |
|---|---|---|
| Nonproliferative changes | No increased risk | 70% |
| Proliferative disease without atypical hyperplasia | Twofold increased risk | 27% |
** Family history limited to mother, daughter, or sister with breast cancer
CONVENTIONAL TREATMENT
Conventional treatment for fibrocystic breasts includes encouraging women to wear loose fitting brassieres, decreased caffeine consumption, and smoking cessation, and a pharmacologic focus on hormonal modulation, including oral contraceptives (OCs), prolactin antagonists, and antiestrogen agents as well as diuretics for moderate premenstrual mastalgia; and analgesics such as ibuprofen, salicylates, and acetaminophen for pain.36,38 Hormonal therapies often carry unwanted side effects, including weight gain, lipid profile changes, depression, and abnormal bleeding.36 Although OCs reduce symptoms in up to 90% of women, symptoms return upon discontinuation.36 Danazol, which suppresses the pituitary ovarian axis by inhibiting the output of both FSH and LH from the pituitary gland, is also used for mastalgia. Its side effects include virilization, muscle cramps, CPK elevations, and liver damage. Bromocriptine is also used for breast pain and nodularity but has several common side effects, including nausea, giddiness, and postural hypotension.36 Reduction in dietary fat intake has been shown to reduce cyclic mastalgia.
BOTANICAL TREATMENT
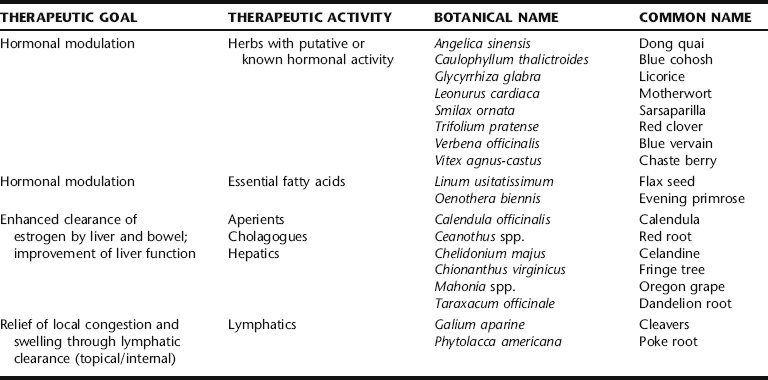
Botanical treatment for fibrocystic breasts has not been widely subject to scientific evaluation, in spite of this being a commonly treated condition in the herbal clinic. Treatment aims primarily at hormonal regulation through direct (i.e., HPA and HPO axes) and indirect (i.e., improved hormonal biotransformation and excretion) actions, and reduction of local congestion and symptomatic pain relief through topical applications (Table 7-3). The liver plays a central role in metabolizing and detoxifying sex hormones.34 Consequently, herbal practitioners typically include herbs that are known or thought to enhance hepatic detoxification functions in formulae for treatment of fibrocystic breasts.34 Such herbs, many of them considered “bitters,” include dandelion root, burdock, root, licorice root, Oregon grape root, fringe tree, motherwort, blue vervain, and celandine. These botanicals are usually included in ranges of 5% to 20% of formulae, in tincture or decoction forms. Although there has been little investigation of such herbs to establish their pharmacologic or physiologic action for such use, they are nonetheless a common part of the protocol for many gynecologic concerns, including benign breast complaints, and their role in formulae should be considered and further evaluated.
Chaste Berry
Chaste berry is extensively recommended by herbal practitioners for cyclic breast pain and fibrocystic breasts, both when it presents independently and when associated with PMS. This traditional use is supported by clinical trials. Chaste berry may be used singly or in combination with other herbs that enhance hormonal regulation and hormone metabolism (e.g., herbs that promote liver function and hormonal conjugation and elimination). There have been three placebo-controlled, double-blind, randomized clinical trials (RCT) examining the effects and safety of a proprietary chaste berry extract–containing solution (VAC) on cyclic mastalgia. VAC is sold as Mastodynon®, and manufactured by Bionorica Arzneimittel GmbH (Neumark/Opf. Germany).41 It contains 32.4 mg of chaste berry fruit extract/60 drops as well as a mixture of homeopathic ingredients, including Caulophyllum thalictroides, Cyclamen, Ignatia, Iris, and Lilium. This product is available as both a tablet (MR 1025 E1) and a liquid extract in Germany. German drug indications for the product include menstrual disorders based on a temporary or permanent corpus luteum insufficiency, infertility resulting from corpus luteum insufficiency, and menstrually related complaints, including mastodynia.42 All three of the studies used the liquid solution, which contained 53% (v/v) alcohol, although the study by Wuttke et al. also used the tablets.41,43 All three studies defined cyclic mastalgia as having at least 5 days of breast pain the previous cycle and treated women for three menstrual cycles with 30 drops two times daily of VAC (1.8 mL/equivalent to 32.4 mg extract of chaste berry drug). Researchers found that both the severity (assessed on a 1- to 100-mm visual analog scale [VAS]) and presence of breast pain (as measured by women’s diaries) were significantly improved in the women who were assigned to the chaste berry groups compared with placebo after the first month of treatment. Although pain intensity was reduced by 30% in the chaste berry group compared with 11% in placebo after one cycle, pain intensity was even more reduced at the end of the second month of treatment, with 53% of women receiving chaste berry having decreased severity of breast pain compared with 25% of the placebo group (p = 0.006).41 No further improvement was obtained with longer treatment periods. However, to reduce the number of days with severe pain women needed to receive VECS for three to four cycles before they had significantly fewer days with breast pain compared with the placebo group (p = 0.21).41,44 Two of the studies also measured serum hormone levels including estradiol, progesterone, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and basal prolactin levels at baseline and in the premenstrual weeks of cycles 1, 2, and 3.43,45 One study found a significant rise in prolactin levels and a decrease in progesterone levels,45 whereas another study found no effect on FSH, LH, and progesterone, but did see a decrease in estradiol levels and a significant decrease in basal prolactin levels (3.7 ng/mL tablets and 4.35 ng/mL liquid extracts) compared with placebo.43 Adverse events were rare and did not differ from placebo in any of the RCTs.
Dong Quai and Blue Cohosh
Along with chaste berry, dong quai and blue cohosh are commonly employed by herbal clinicians to modulate hormone levels. Blue cohosh, as part of the German herbal formulation Mastodyn® (reviewed in the preceding), may provide some of the therapeutic benefit of that formulation. However, to date, no studies have demonstrated that blue cohosh has any effect on hormonal levels. Dong quai in vitro can weakly bind to estrogenic receptors and induce progesterone receptors. However, it did not stimulate vaginal cells or increase endometrial thickness and had no estrogenic effect showing no transactivation of either alpha- or beta-estrogen receptors.27,46,47 Additionally, dong quai showed no significant effect on either hormonal levels or symptoms in an RCT in menopausal women.48,49 Consequently, dong quai appears to have a limited if any effect on hormone levels. In a recent study, dong quai was found to have significant anti-inflammatory effects because of one of its constituents, ferulic acid.50 Although this study is very preliminary, it may offer an alternative mechanism through which dong quai could be helping to decrease mastalgia in women with fibrocystic breasts. According to TCM theory, dong quai dissolves blockages and relieves blood stagnation, and is thus a common ingredient in formulae for mastalgia.
Flax Seed and Evening Primrose Oil
Flax seeds are the richest source of plant-based omega-3 fatty acids, with a-linolenic acid (ALA) being the primary fatty acid (18:3n-3).51 These fatty acids are considered strongly anti-inflammatory, being precursors for the anti-inflammatory series prostaglandins (PGE3). Flax seeds are also rich in fibers called lignins. Like isoflavones in soy and other foods, lignins and their associated phenolic compounds are classified as phytoestrogens.52,53 Flax seeds are an especially rich source of dietary lignins, with 75 to 800 times more than any other food source.51,54 Research has shown lignins to be a promising agent for binding excess sex hormones, including testosterone and estrogens. Through both its anti-inflammatory and possible anti-estrogenic effects researchers believed that flax may prove a beneficial treatment for fibrocystic breasts. One study examined the effect of eating one muffin daily supplemented with 25 g of ground flax seeds in 127 women with mastalgia.55 Women experienced a significant reduction of symptoms; however, the full results of this study were never published and thus it is unknown how long women needed to take the flax seed–enriched muffins, what symptoms were reduced, what the degree of symptom reduction was, or if there was any placebo control to assess for the considerable level of spontaneous remission (60% to 80%) of symptoms in women with breast pain over time.55 Evening primrose oil (EPO), is a rich source of omega-6 essential fatty acids (EFAs). EFAs are precursors to either series 1 or 2 prostaglandins, depending on substrate availability. The more omega-6 EFAs there are in the diet, the more likely it is for the inflammatory series prostaglandins to be made; conversely, the less omega 6 EFAs there are in the diet, the more likely it is for anti-inflammatory series 1 prostaglandins to be produced. Because of EPO’s potential anti-inflammatory properties, two randomized placebo-controlled, double-blind clinical trials and one open-labeled trial of EPO in both cyclic and noncyclic mastalgia have been conducted. One double-blind, placebo-controlled randomized study in 73 women with either cyclic or noncyclic mastalgia found that 1000 mg of EPO or placebo three times daily over 3 months significantly reduced symptoms of pain and tenderness in the women who received EPO compared with placebo.56 In a similar study, 291 women with severe persistent breast pain given either placebo or 1000 mg EPO three times daily for 3 to 6 months found that 45% of women with cyclic pain improved. Further, 27% of women with noncyclic breast pain improved compared with 9% in the placebo group.57 In a nonrandomized open-labeled study, 94 women with cyclic and 32 women with noncyclic mastalgia received 3 g of EPO for at least 4 months. Severity of pain was diminished in a “clinically useful”40 manner in 58%49 of the women with cyclic mastalgia and 38%12 of the women with noncyclic mastalgia taking EP. Unfortunately, all three of these studies are difficult to assess because of lack of reporting of how pain and symptoms were measured and how great the effect, and thus how clinically relevant the effect of EPO is in women with breast pain.40 The recommended dose of flax oil to treat and prevent mastalgia and nodularity is two to four 500-mg capsules twice daily or 1 to 2 tablespoons of the oil daily. One to three grams daily is the recommended dose of ground seeds.58 A typical dose of EPO is 1500 mg daily.
Red Clover
Red clover is rich in isoflavones, especially genistein and daidzein. Genistein and daidzein have weak estrogenic effects, which have led researchers to hypothesize that genistein may compete with stronger endogenous estrogens such as estradiol for estrogen receptors; although what effects this may have on breast tissue is unclear at this time. One unpublished study found that a red clover extract had a significant effect on improving mastalgia. No further information is available concerning this trial.59
Topical Applications
Poke Root
Poke root has traditionally been used to stimulate the immune system, relieve lymph congestion, and resolve
Botanical Protocol for the Treatment of Fibrocystic Breasts
I. Prepare the Following Tincture:
| Calendula | (Calendula officinalis) | 20 mL |
| Chaste berry | (Vitex agnus-castus) | 20 mL |
| Burdock root | (Arctium lappa) | 20 mL |
| Sarsaparilla | (Smilax ornata) | 20 mL |
| Dandelion root | (Taraxacum officinale) | 20 mL |
| Total: 100 mL | ||
lumps and cysts, and by extension, has been widely applied topically for the treatment of fibrocystic breasts. Poke root oil is applied topically by rubbing in a small amount (1 tsp) of the oil throughout the affected breast(s) for at least 5 nights per week for 1 to 2 months. The addition of 5 to 7 drops each of rose geranium and sandalwood essential oils makes the oil slightly more stimulating to the local circulation and also adds a pleasant scent to the oil. All parts of the plant are toxic and can lead to contact dermatitis or even toxicity from handling large amounts. Internal use is not recommended without the supervision of a qualified practitioner.
CASE HISTORY: CYCLIC MASTALGIA
She was prescribed the following tea for her to take after supper to help her sleep:
| Passionflower | (Passiflora incarnata) | 2 parts |
| Chamomile | (Matricaria chamomilla) | 2 parts |
| Skullcap | (Scutellaria lateriflora) | 1 part |
For her mastalgia and menstrual irregularities, she was prescribed the following tincture:
| Chaste berry | (Vitex agnus-castus) | 20 mL |
| Burdock root | (Arctium lappa) | 20 mL |
| Cleavers | (Galium aparine) | 20 mL |
| Dong quai | (Angelica sinensis) | 40 mL |
| Total: 100 mL |
NUTRITIONAL CONSIDERATIONS
Elimination of Coffee, Tea, and Other Caffeinated Products
An association between caffeine, or methylxanthines, and fibrocystic breast disease has been reported but remains controversial. In one study of a group of 102 women who had mammograms performed to measure the level of fibrocystic breast disease, a strong correlation was found with both caffeine and total methylxanthine ingestion and fibrocystic breasts as determined by a series of questionnaires.60 Similar results were found in a large case control study of 634 women.61 Other studies, however, have found only weak associations. Normal fluctuations in hormonal effects on breast tissue and difficulty in consistently measuring caffeine or methylxanthine intake make it difficult to conclusively demonstrate a causal relationship.62,63 In a review of the literature presented on AltMedex, the following studies are cited: A controlled clinical trial showed no clinically or statistically significant effects of alcohol- or methylxanthine-free diets on signs and symptoms of fibrocystic breast disease. One hundred sixty-two women with clinical and thermographic diagnoses of fibrocystic breast disease completed the study with evaluation at 6 months. It was concluded that abstinence from alcohol or methylxanthine-containing beverages is not likely to substantially reduce severity of fibrocystic breast disease within a few months.64 A case control study examined the relationship between coffee consumption and the development of benign breast disease involving the analysis of 854 cases of histologically diagnosed benign breast disease and 1748 control subjects. No association between coffee consumption and benign breast disease was found; neither was a dose–response relationship between methylxanthine consumption and benign breast disease development noted. These results suggest no association between caffeine intake and the development of benign breast disease.65 In a randomized study, 158 women with breast concerns were divided into two groups; one group abstained from consumption of methylxanthine-containing foods and beverages. The second group (controls) had no dietary restrictions. The patients were re-examined at 4 months for palpable breast findings. One hundred forty patients completed the study. There was a statistically significant decrease in clinically palpable breast findings in the abstaining group compared with controls, but the absolute change was minor and may be of little clinical significance. This study offered little support for the claim that caffeine-free diets are associated with clinically significant improvement in benign breast disease.66 In a study of 66 patients, restriction of dietary caffeine ingestion can cause improvement in fibrocystic breast disease. Graphic stress telethermometry (GST) was performed as an objective monitor for fibrocystic breast. At baseline, an average score of 83.5 on GST was observed in these women. Following dietary methylxanthine restriction, these scores were observed to be an average of 69.5 at 2 months and 55.5 at 6 months. Forty-two of the 66 patients had decreases in GST scores of more than 20 points at 6 months. Eighty-five percent of the patients showed improvement in GST patterns at 6 months, 15% of patients showed no change, and none showed worsening in GST patterns. Subjectively, at 6 months, 22 of 66 patients reported marked improvement, 30 of 66 moderate improvement, 6 of 66 mild improvement, and 8 of 66 no change in symptoms of fibrocystic breast disease. At pretreatment, 78% of patients had 2+ or 3+ nodularity on palpation. At the 6-month examination, 89% of patients had no or 1+ nodularity on palpation (91% had improvement, 9% had no change, and none had worsening). In 85 US women with clinical and mammographically confirmed fibrocystic disease, complete abstention from methylxanthine consumption resulted in complete resolution of fibrocystic breast disease in 82.5% and significant improvement in 15% of the patients studied.67
Vitamin E and B6 Supplementation
Supplementation with vitamin E (400 to 800 IU) may be beneficial for reducing mastalgia and nodularity of fibrocystic breasts and pyridoxine (vitamin B6/50 to 100 mg) to reduce breast tenderness and pain.68,69 Women are also encouraged to increase dietary fiber and complex carbohydrates, reduce dietary fat to 15% to 20% of their diet, and move toward a more plant-based diet, rich in phytoestrogens. A recent review examined various dietary therapies, and their potential effects in treating fibrocystic breasts.38 The review found that some dietary therapies, including vitamin E and B6