Computer Applications in Respiratory Care
Computer applications are universal in respiratory care, and their impact continues to advance exponentially. Respiratory therapists (RTs) and other members of the health care team rely on computer applications in clinical care, diagnostics, management, education, and research. Emerging computer technology, or eHealth, applications aim to improve the processes of care and the performance of health care providers, engage patients, facilitate care from a distance, and manage information, improving health outcomes. Abundant, accessible, and up-to-date information from the government, universities, publishers, professional organizations, and industry is available to health care providers and patients on the World Wide Web. As established by a task force of the American Association for Respiratory Care (AARC) to chart a vision for the future, RTs will benefit from knowing how to retrieve information efficiently from the best available evidence-based resources.1 RTs have compelling reasons to learn about computer applications.
Applications in Clinical Care
Mechanical Ventilators
Conventional mechanical ventilators use microprocessors to control flow and pressure for triggering, limiting, and cycling breaths. Some modes of ventilation are closed-loop or adaptive, with predetermined algorithms that take actions automatically within preset limits. Breath-by-breath, microprocessors equilibrate measured values with target values. Based on the lung compliance measured during the previous breath, some modes adjust inspiratory pressure to attain a target tidal volume set by the clinician. New advanced adaptive systems, such as proportional assist ventilation and neurally adjusted ventilatory assist, aim to enhance the patient-ventilator synchrony via automation that is highly responsive to the patient.2
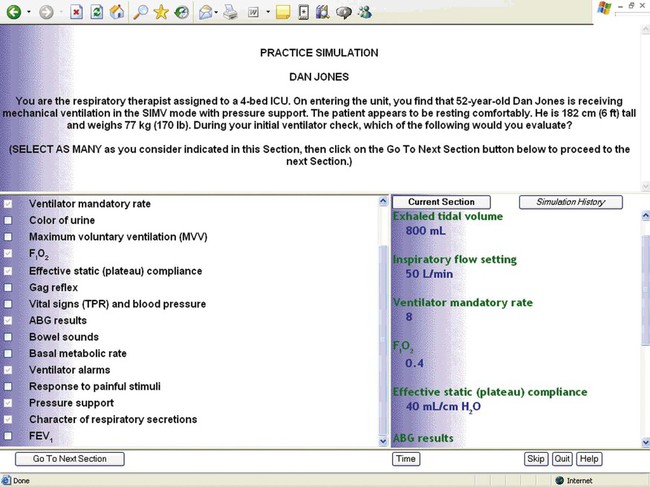
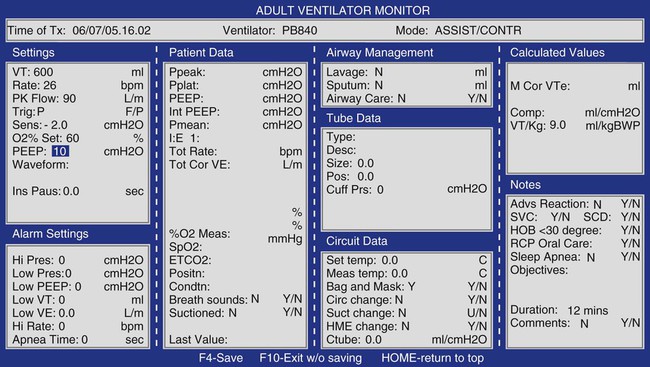
Protocols for ventilator weaning and management of acute respiratory distress syndrome can improve patients’ outcomes; complete, accurate, and consistent documentation of ventilator settings is key. However, manual ventilator charting is frequently incomplete, inaccurate, and inconsistent.3 Computerized ventilator charting applications have the potential to improve the quality and consistency of ventilator charting. Automated ventilator charting, verified by RTs, takes ventilator charting a step further, with the potential to improve completeness, accuracy, consistency, and efficiency.4 Figure 7-1 is an example of a computer screen for automated charting.
Patient-Driven Protocols
Evidence-based, patient-driven protocols can improve health outcomes.5,6 Under medical direction and based on patient assessment, RTs use protocols to allocate and titrate respiratory care. Consistency and timeliness of implementation are keys to the effectiveness of protocols. Automation of protocols at the point of care can help RTs address these concerns. An automated protocol for discontinuation of the mechanical ventilation program on hand-held computers can decrease the time to the first spontaneous breathing trial and the length of stay in the intensive care unit (ICU) compared with a protocol without automation.7 At least once a shift, RTs enter information about each mechanically ventilated patient via a hand-held computer. When patients meet preset criteria, the computer program prompts the RTs to conduct a spontaneous breathing trial to help determine the patients’ readiness for ventilator discontinuation.
Clinical Decision Support
Clinical decision support systems are associated with improved clinician performance, decreased unnecessary care, and adherence to evidence-based clinical practice guidelines.8,9 These systems are particularly useful in preventive care. Computerized reminders increased the proportion of indicated influenza vaccinations, rates of screening, counseling, and adherence to medications. They have also resulted in decreased unnecessary hospital admissions for inappropriately diagnosed cardiac ischemia, appropriately decreased tidal volume and more consistent monitoring of plateau pressure in patients with acute respiratory distress syndrome, and decreased exacerbations in asthma patients.8 Clinical decision support is instrumental in improving clinical outcomes of patients by determining optimal drug dosages. Beneficial outcomes include the following:
Telemedicine
Telemedicine is the use of telecommunication and computer technology to promote access to diagnosis, monitoring, clinical decision support, and treatment for patients at medically underserved sites that are distant from health care providers. Telemedicine has been effectively implemented in various clinical settings, including home care, emergency departments, and ICUs, and is well accepted by patients.11 Clinical outcomes have generally been similar to traditional health care delivery models; however, in the ICU setting, supplemental telemedicine has been associated with improved clinical outcomes, particularly among the most critically ill patients.12,13 From a distance, on computers either within the hospital or at home, intensive care physicians can see the vital signs, ventilator data, medical record, and diagnostic images of the remote patients. Supplemental telemedicine helps to provide additional support that can potentially result in more rapid recognition of problems and timely, appropriate interventions.14
Treatment of Tobacco Use and Dependence
In the United States, tobacco use and dependence is the leading preventable cause of death and chronic diseases.15 Health care costs attributable to tobacco use are unsustainable. Effective evidence-based treatments are available, but their implementation by health care providers is lagging.16 RTs can play a vital role in the treatment of tobacco-related diseases and should aid in the pursuit of cost-effective ways to help tobacco users.
Emerging applications of computer technology, or eHealth applications, are exciting new components of treatment for tobacco use and dependence. With the extensive reach of the Internet and the demonstrated efficacy of some applications, the potential impact on health outcomes is immense. More than 10 million Internet users have searched for online information about how to quit smoking.17
Internet-based treatment programs can recruit tobacco users via search engines, or they can be an adjunct to telephone quitline counseling. Figure 7-2 is a screen shot from the smokefree.gov tobacco treatment website. When eHealth applications are tailored to individual tobacco users, with frequent automated contacts via e-mail or text messages, rates of long-term abstinence from tobacco use are similar to other evidenced-based interventions.18–22
Consistent with the U.S. Public Health Service clinical practice guideline recommendation for a high-intensity, multicomponent approach, an Internet-based application has the capacity to provide both counseling that promotes tailored quit strategies and tobacco cessation medications that have been approved by the U.S. Food and Drug Administration (FDA).16 Internet-based applications can provide unlimited, sustained access to virtually limitless numbers of participants. These applications can be highly cost-effective. Table 7-1 lists some websites related to the treatment of tobacco use and dependence.
TABLE 7-1
Websites Related to the Treatment of Tobacco Use and Dependence
| Website | Organization |
| SmokeFree.gov | U.S. Department of Health and Human Services |
| QuitNet.com | QuitNet |
| WHO.int/tobacco | World Health Organization, Tobacco Free Initiative |
| ITCProject.org | International Tobacco Control Policy Evaluation Project |
| ATTUD.org | Association for the Treatment of Tobacco Use and Dependence |
| TreaTobacco.net | Society for Research on Nicotine and Tobacco |
| TobaccoFreeKids.org | Tobacco Free Kids |
Management of Chronic Respiratory Diseases
Management of chronic diseases presents a grave challenge to the U.S. health care system. In the United States, 7 out of 10 deaths are due to chronic disease.23 Chronic disease is present in 8 out of 10 Americans on Medicare, and chronic diseases account for three out of every four dollars of health care expenditures in the United States.24,25 As baby boomers age in the coming decades, the proportion of the U.S. population 65 years old and older is expected to double. There is much interest in addressing the historically disjointed, misallocated processes of chronic disease management through advances in eHealth technologies, to improve health outcomes in a cost-effective manner. In the United States, 60% of households have access to computers, and the availability of broadband access to the Internet is expanding.17 In the United States, which has a population of 311 million people, there are more than 307 million wireless mobile phone connections.26,27
Asthma
eHealth applications for asthma include interactive Internet applications, such as games for children, Internet applications linked to cell phones for personalized or automated voice or text messaging, and other telemonitoring devices. Many of these applications use monitored patient data to tailor the adjustment of the plan of care. Some provide for personalized goals, calendars, and reminders. Educational tools include audiovisuals and quizzes. In patients with persistent asthma, evidence from research studies shows that these eHealth applications can result in an improvement in asthma knowledge, self-management skills, peak flow rates, and adherence to inhaled corticosteroid controller medications and fewer symptoms, missed school days, nighttime awakenings, activity limitations, emergency department visits, and hospitalizations.28–33 These applications are well received by patients.30
A cornerstone of asthma disease management is assessing patients’ level of control of the disease over time. One validated measure of impairment, recommended by the National Asthma Education and Prevention Program, is the Asthma Control Test.34 This free questionnaire is available in an online format (see www.asthmacontrol.com), which patients can complete and take to a health care provider.
Chronic Obstructive Pulmonary Disease
Increasingly, chronic obstructive pulmonary disease (COPD) is being managed in the home. Internet-based telemonitoring systems, smartphones, and mobile phones with computer applications extend the reach of health care providers into the home. eHealth applications for patients with COPD facilitates education, self-management, and timely feedback from health care providers (Figure 7-3). Patients generally have a positive attitude about the role of this technology, and the quality of the transmitted data is good.35 Improved outcomes include earlier identification of deteriorating symptoms, better response to exacerbations, increased rate of sustained exercise after pulmonary rehabilitation, and decreased emergency department visits and hospitalizations.35–37 Additionally, eHealth applications can help detect comorbidities, such as sleep apnea.35
Applications in Diagnostics
Hemodynamic Monitoring
Pulmonary Function Laboratories
Interpretation of Pulmonary Function Tests
The American Thoracic Society recommended pulmonary function reference standards based on the National Health and Nutrition Examination Survey (NHANES). These standards for prediction of normal PFT values may differ from other reference values. This difference can confound the interpretation of successive PFTs in an individual patient when clinicians focus on the computer-assisted interpretation of percent-of-predicted values, rather than the actual observed values.38 Clinicians should have a clear understanding of which reference values were used for each test and interpret PFT results accordingly.
Information Retrieval
Although assessment skills of RTs generally sharpen with experience, their knowledge of the most up-to-date therapies may diminish over time.39 However, the best available medical evidence is dynamic rather than static, and the amount of available information is staggering. A search with the Google search engine using the search word “smoking” yielded more than 169 million results in a fraction of a second. RTs need to be knowledgeable about efficient ways to access, filter, and retrieve information effectively. They must also be prepared to guide increasingly sophisticated patients, many of whom actively seek medical information on the Internet, in retrieving reliable information.
World Wide Web
The World Wide Web is a far-reaching, rich source of information. RTs can “bookmark” helpful websites for clinical practice guidelines, evidence-based systematic reviews of clinical questions, accrediting agencies, or other relevant sites for rapid retrieval of important information (Table 7-2). For example, the Cochrane Collaboration (see www.cochrane.org), well respected for rigorously conducted systematic evidence-based reviews, provides free access to abstracts and summaries pertaining to relevant clinical questions, including questions related to “airways.”
TABLE 7-2
Helpful Websites for Respiratory Therapists
| Organization | Website |
| American Academy of Allergy, Asthma, and Immunology | www.aaaai.org |
| American Academy of Pediatrics | www.aap.org |
| American Academy for Sleep Medicine | www.aasmnet.org |
| American College of Allergy, Asthma, and Immunology | www.acaai.org |
| American Association for Respiratory Care | www.aarc.org |
| American Cancer Society | www.cancer.org |
| American College of Chest Physicians | www.chestnet.org |
| American Heart Association | www.heart.org/heartorg |
| American Lung Association | www.lungusa.org |
| American Thoracic Society | www.thoracic.org |
| ARDS Network | www.ardsnet.org |
| Centers for Disease Control and Prevention | www.cdc.gov |
| Cochrane Collaboration | www.cochrane.org |
| Committee on Accreditation for Respiratory Care | www.coarc.com |
| Cystic Fibrosis Foundation | www.cff.org |
| Global Initiative for COPD | www.goldcopd.com |
| National Board for Respiratory Care | www.nbrc.org |
| National Heart, Lung and Blood Institute | www.nhlbi.nih.gov/health/indexpro.htm |
| Society for Critical Care Medicine | www.sccm.org |
| U.S. Surgeon General | www.surgeongeneral.gov |
Google Scholar
Google Scholar (see scholar.google.com) is a search engine for scholarly publications in a wide range of fields. It includes peer-reviewed manuscripts, abstracts, theses, and books from academic publishers, professional societies, and university libraries. Google Scholar uses a special algorithm to rank and determine the order of the search results. Variables in the algorithm include analyses of citations, authors, publications, and full texts.
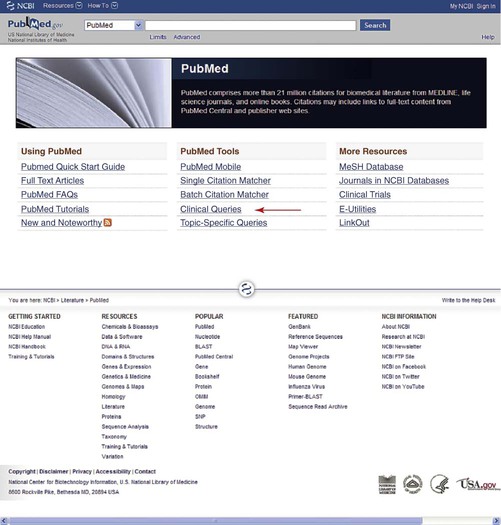
PubMed and MEDLINE
PubMed (see www.pubmed.com) is the free search engine of the National Library of Medicine for health information. It searches several databases, including MEDLINE, the database of the National Library of Medicine of millions of references from thousands of journals related to medicine, nursing, the health care system, and science. The National Library of Science updates MEDLINE references in PubMed almost daily. Each MEDLINE citation in PubMed generally has the following information: title, authors, an abstract, journal, language, type of publication, and Medical Subject Headings (MeSH).
A unique feature of PubMed is that it maps users’ search terms to MeSH. PubMed uses Boolean logic, in which users can combine search words or phrases with connectors such as AND or OR to narrow or broaden searches. Box 7-1 provides examples to illustrate the use of Boolean connector terms.
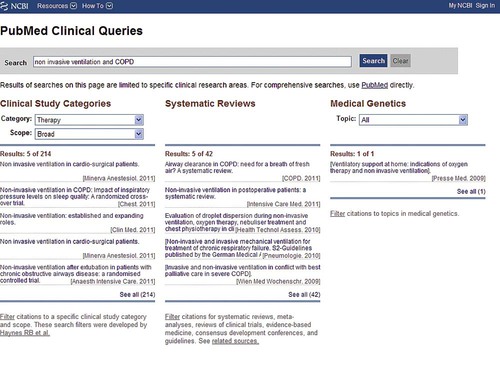
PubMed Clinical Queries Filter
The Clinical Queries search filter in PubMed is easy to use and very effective in retrieving valid research studies. To access it, on the PubMed home page, in the center column, under “PubMed Tools,” click “Clinical Queries” (Figure 7-4). On the Clinical Queries page, select one of the “Clinical Studies Categories,” such as “Therapy” or “Diagnosis.” Then select the scope of the search, as either “Broad” or “Narrow.” A “Broad” search is more sensitive, providing more search results; a “Narrow” search is more specific, providing fewer search results. Selection of “Broad” versus “Narrow” depends on the reason for the search. Search results include clinical research studies in the left column and systematic reviews in the center column, or the user can elect to include only systematic reviews in the search results (Figure 7-5). When the user selects “Therapy” from the “Clinical Study Categories” with a “Narrow” scope, the Clinical Queries filter automatically searches for randomized controlled trials and systematic reviews.
The Clinical Queries search filter is very sensitive (true positives/true positives + false negatives) and specific (true positives/true positives + false positives) in the retrieval of the best available scientific evidence. A validation study of this search filter yielded 93% sensitivity and 97% specificity.40 The Clinical Queries search filter effectively retrieves valid research studies, while eliminating nonrelevant information and poorly designed studies. Compared with Google Scholar, which lacks any way to filter a large volume of information, PubMed Clinical Queries filter is equally sensitive but considerably more specific, reducing the time it takes to find the best available evidence.41
Information Retrieval by Patients
With the advent of extensive available information on the Web, patients increasingly seek knowledge about diseases and treatments on their own. Eight in 10 Internet users have searched the Web for health information.17 However, many Web users neglect to scrutinize the quality or source of the information, which is largely unregulated.42 RTs should be able to offer guidance to patients about appropriate information sources. Table 7-3 presents the Health on the Net criteria for evaluating the quality of medical and health websites. Selected resources for patients include the AARC site for patients (see www.yourlunghealth.org), the website of the National Lung Health Program (see www.nlhep.org) dedicated to COPD patients, and MedlinePlus.gov of the National Library of Medicine. MedlinePlus features online interactive tutorials, practical instructional handouts for patients, a medical encyclopedia, and videos of surgical procedures.
TABLE 7-3
Health on the Net Code of Conduct for Medical and Health Websites
| Principle | Code |
| Authority | Any medical or health advice provided and hosted on this site will be given only by medically trained and qualified professionals unless a clear statement is made that a piece of advice offered is from a non–medically qualified individual or organization. |
| Complementarity | Information provided on this site is designed to support, not replace, the relationship that exists between a patient/site visitor and existing physician. |
| Confidentiality | Confidentiality of data relating to individual patients and visitors to a medical/health website, including their identity, is respected by this website. The website owners undertake to honor or exceed the legal requirements of medical/health information privacy that apply in the country and state where the website and mirror sites are located. |
| Attribution | Where appropriate, information contained on this site will be supported by clear references to source data and, where possible, have specific HTML links to that data. The date when a clinical page was last modified will be clearly displayed. |
| Justifiability | Any claims relating to the benefits/performance of a specific treatment, commercial product, or service will be supported by appropriate, balanced evidence. |
| Transparency of authorship | The designers of this website will seek to provide information in the clearest possible manner and provide contact addresses for visitors that seek further information or support. The Webmaster will display his/her e-mail address clearly throughout the website. |
| Transparency of sponsorship | Support for this website will be clearly identified, including the identities of commercial and noncommercial organizations that have contributed funding, services, or material for the site. |
| Honesty in advertising and editorial policy | If advertising is a source of funding, it will be clearly stated. A brief description of the advertising policy adopted by the website owners will be displayed on the site. Advertising and other promotional material will be presented to viewers in a manner and context that facilitates differentiation between it and the original material created by the institution operating the site. |
Applications in Management and Administration
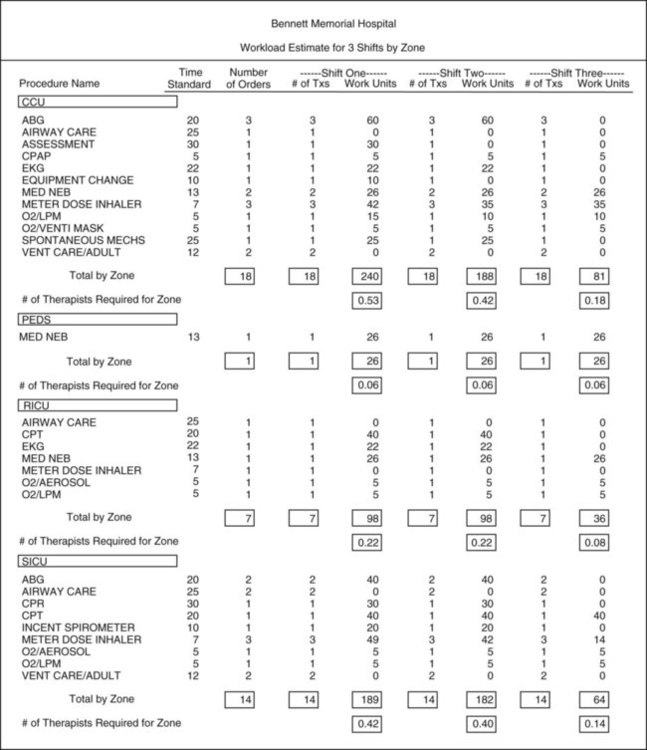
Respiratory Care Management Information Systems
Many respiratory care departments use respiratory care management information systems. In addition to charting and billing, respiratory care management information systems provide a means to organize and assign respiratory care orders, measure staff productivity, report clinical results, and execute respiratory care protocols, along with generating data to show their effectiveness via outcomes research (Figure 7-6).
Hand-held computers offer several advantages compared with paper charts. Hand-held computers facilitate the organization and assignment of workload, facilitate the fulfillment of physicians’ orders, and improve documentation.43,44 Documentation of patient assessment becomes immediately available to other members of the health care team in the HIS. Incomplete or lack of patient information, which is more likely to occur with paper charts, is associated with numerous medical errors that cause adverse events, including prolonged hospitalization and death.45
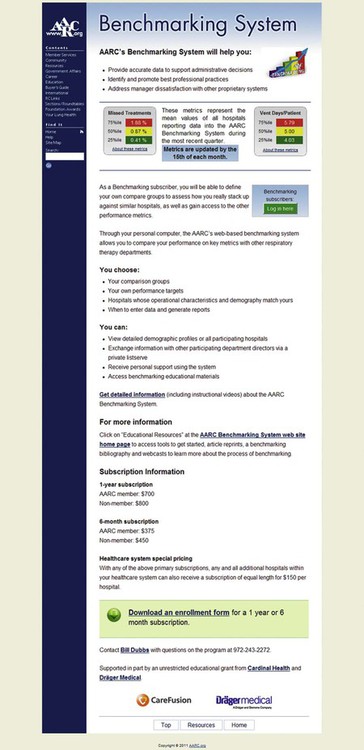
Benchmarking
Benchmarking is valuable for each of the primary functions of respiratory care managers, including planning, organizing, directing, and evaluating. The AARC provides an online benchmarking system (Figure 7-7) in which managers can compare the performance of their department with other similar departments. Managers can compare the ratio of ventilator days with the number of patients or the number of missed treatments in a given time frame. Benchmarking helps to show the productivity of the department and establish best practices.
Electronic Health Records
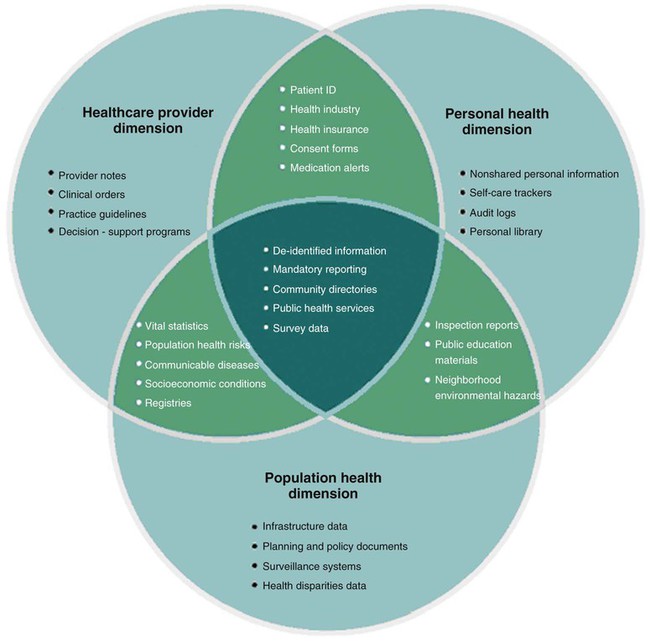
Electronic health records can improve access to patients’ updated health information for both clinicians and patients and assist clinicians with clinical decision support. Many investigators have begun to focus attention on the development of a seamless network of transferable, widely accessible, longitudinal electronic health records. A comprehensive national health information infrastructure would result in interconnectivity among health information systems in the United States.46 Core functions are shown in Box 7-2.
The electronic health record would become the central component of health care information systems, satisfying the information needs of health care providers, public health officials, and individuals, and potentially reduce medical errors and elimination of redundant diagnostic tests (Figure 7-8). It would support health systems planning and development of policies. Major barriers and challenges for the development and implementation of electronic health records are costs, the lack of uniformity of data, the inability to establish an interface among different health information systems, and accounting for the needs of various health professional disciplines.
Applications in Education
Clinical Simulation
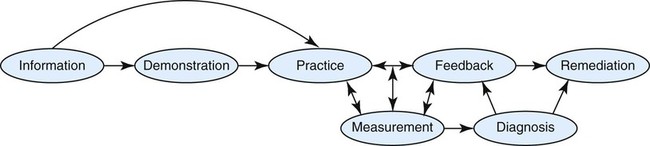
Learners are able to suspend disbelief, immersing themselves in carefully planned case scenarios and performing in a manner similar to that of real clinical situations (Figure 7-9). They develop psychomotor, critical thinking, decision-making, and team-building skills. In contrast, traditional methods of didactic education in combination with clinical apprenticeships can result in increased knowledge, but limited, inconsistent experiential learning opportunities, without the benefit of remediation and extensive practice based on feedback. Clinical simulators, to a certain extent, allow for in-depth evaluation of learners’ competencies, rather than evaluation based on the length of time for clinical rotations or the number of performed procedures. They are an excellent tool to help respiratory care departments meet The Joint Commission requirement of demonstrating the competencies of respiratory care staff in an ongoing manner.47,48 Recommended steps in clinical simulation education are diagrammed in Figure 7-10.
Clinical simulators are particularly valuable for learning how to function in rare but high-risk clinical situations. Training via simulators has resulted in improved performance of health care providers in emergency airway management, advanced life support, bronchoscopy, and surgery.49–53 Clinical simulators have the potential to reduce medical errors and improve patient safety. Simulations promote relatively comprehensive learning (Box 7-3). Performances in clinical settings become more refined and automatic.
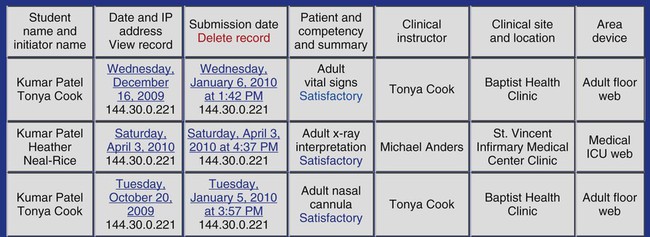
DataARC
DataARC (see www.dataarc.ws) is a secured, password-protected, Web-based database management system for documenting and reporting clinical educational activities for nursing and allied health professions, including respiratory care. The records help both students and faculty members identify underaddressed clinical activities and competencies (Figure 7-11). Functions include the following:
National Board for Respiratory Care Credentialing
The National Board for Respiratory Care (NBRC) uses computerized credentialing examinations. NBRC credentialing for the registry for advanced RTs consists of two distinct examinations—the written examination and the clinical simulation (Figure 7-12).
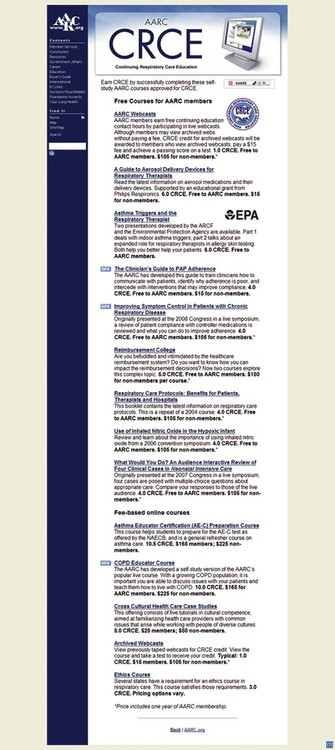
Continuing Education
American Association for Respiratory Care
The AARC provides plentiful continuing education opportunities on the Web (see www.aarc.org). Web casts and text-based courses are available in both a live and an asynchronous manner. RTs may earn continuing respiratory care education (CRCE) credit by completing these courses (Figure 7-13). The AARC also provides Web-based CRCE credits through the Respiratory Care journal. Therapists can read the journal, use a copy of the test that appears in the journal to draft answers, and then complete the Web-based test on the journal website (www.rcjournal.com/online_resources/crce). The AARC maintains a database of members’ CRCE credits, which RTs can access on the AARC website.
Pulmonary Artery Catheter Education Project
The Pulmonary Artery Catheter Education Project (see www.pacep.org) provides excellent online training in hemodynamic monitoring. It includes Web casts with audio and slides and pretesting and posttesting for each module and case studies for many of the modules.
Applications in Research
Computers are indispensable in research. Some of the more common functions are presented in Box 7-4.
Data Sources
Additionally, public data sources are available on the Web to support descriptive and analytic research. The National Center for Health Statistics (see www.cdc.gov/nchs), the principal health statistics agency in the United States, oversees birth and mortality data, the National Maternal and Infant Health Survey, the Longitudinal Studies on Aging, the National Asthma Survey, and the NHANES. The NHANES is a comprehensive survey and examination of a nationally representative sample and includes data concerning demographics, tobacco use and other behaviors, pulmonary diseases, laboratory data, physical examination, and spirometry. State public health agencies are sources of public data available to researchers from instruments such as the Youth Behavioral Risk Survey.
Data Collection
Computers facilitate data collection via either hand-held computers or Web-based survey software. Compared with traditional paper methods of data collection, hand-held computers improve adherence to instructions, are faster, are preferred by research subjects, and may improve data accuracy.54
Web-based survey software, such as Survey Monkey (see www.surveymonkey.com) and Questionmark Perception (see www.questionmark.com/us/perception/index.htm), is a cost-effective approach for data collection. These tools enable researchers to create secured, Web-based, questionnaires with the capacity for adaptive branching of questions, tracking respondents, and downloading data into spreadsheets or statistical software.
Citations and Bibliographies
Web-based software (see www.EndNote.com; www.RefWorks.com) automates the otherwise unwieldy and sometimes exhausting task of generating and formatting citations and bibliographies in research manuscripts. With relative ease, researchers can search for, import, organize, manage, and share databases of references.
Security and Confidentiality
Security
Confidentiality
Health Insurance Portability and Accountability Act of 1996 (HIPAA) regulations concerning confidentiality are pertinent to electronic medical records and research data that contain personal health information (see Chapter 5). To emphasize two important points concerning electronic personal health information, users of hospital and respiratory care information management systems and researchers must (1) refrain from sharing passwords and (2) access personal health information only on a need-to-know basis. Some respiratory care information management systems now feature thumbprint protected security.