Complications of transurethral resection of the prostate
In a traditional TURP, resection of the prostate is performed during cystoscopy using a resectoscope with an electrocautery loop. The morbidity rate of 7% to 20% is associated with longer resection times (>90 min), larger gland size (>45 g), acute urinary retention, and age greater than 80 years. One of the most serious complications associated with TURP, TURP syndrome (Box 166-1) occurs in 2% to 15% of patients treated with this approach. Postoperative bleeding with the need for blood transfusion occurs in about 2% to 4.8% of patients who develop TURP syndrome.
Specific complications
Turp syndrome
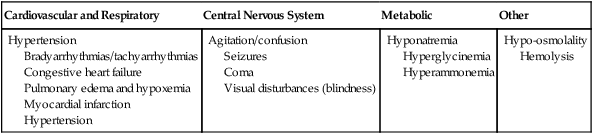
TURP syndrome, a constellation of symptoms and signs caused by excessive absorption of the irrigating fluid, may occur at any time perioperatively. Patients who undergo a TURP with a neuraxial anesthetic and who remain awake will often complain of nausea, headache, and dizziness as the first manifestations of TURP syndrome, which progresses to dyspnea and confusion. Agitation often ensues, associated with elevated blood pressure and bradycardia; if no treatment is implemented, seizures and cardiac arrest may follow (see Box 166-1). Diagnosing TURP syndrome in patients who undergo TURP with general anesthesia may be difficult because the first signs are hypertension and severe refractory bradycardia, followed in short order by seizure and cardiac arrest. These signs develop most often in patients with preexisting compromised myocardial function whose compromise leaves them unable to handle the increased intravascular absorption of the irrigating solution.
< ?xml:namespace prefix = "mml" />