Chapter 51 Complications of Managing the Airway
I Complications in Managing Patients with Difficult Airways
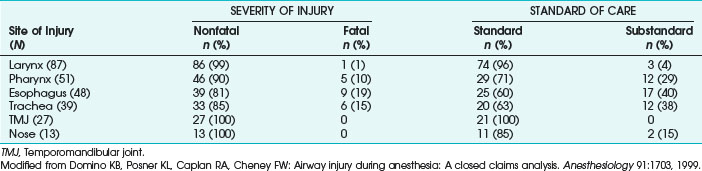
Difficulty in managing the airway is the most important cause of anesthesia-related morbidity and mortality. In the American Society of Anesthesiologists (ASA) Closed Claims Project, 6% of all claims concerned airway injury.1 Difficult intubation was a factor in only 39% of airway injury claims. Eighty-seven percent of the airway injuries were temporary, and 8% resulted in death. In 21%, the standard of care was inappropriate (Table 51-1). Female patients, elective surgery, and outpatient procedures had higher rates of injury. There was no difference in ASA physical status classification and obesity among those with airway injuries during general anesthesia.
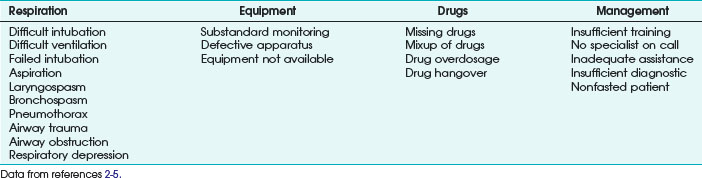
International studies exploring the incidence of complications during general anesthesia have been published in the United Kingdom,2,3 Australia,4 and France.5 The procedural problems and airway complications found in these studies are summarized in Table 51-2.
A History of the Patient and Examination
All tests should be performed in a standardized manner for every patient to prevent errors in the results. Practitioners should understand the functions and limits of each test. Combinations of simple tests or the application of more complex tests may increase the predictive value of the preanesthesia examination findings.6,7 In uncertain cases, the preoperative evaluation of the airway can use fiberoptic devices under local anesthesia. Test and physical examination results must be documented, especially when the examiner is not the person administering anesthesia during the procedure.
II Complications with Supralaryngeal Airway Devices
A Mask Ventilation
The difficult mask ventilation is an underestimated aspect of managing a difficult airway. Ventilation using a bag-mask breathing system is an essential task of the trained anesthesiologist, and it may be life-saving for the patient. The “cannot intubate, cannot ventilate” (CICV) scenario represents the most extreme type of airway problem.8 Mask ventilation is used at the beginning of most cases of general anesthesia. Although the mask and the technique may seem benign, each can cause problems.
1 The Sterilization Process
Many of the devices used to ventilate the patient and secure the airway are disposable, but some equipment is reusable. All devices should be checked before use, and reusable items should be free of residual cleaning agents. Masks may have pinhole defects in their air-filled bladders, allowing air leaks or extravasation of cleaning fluid. In one case report, the fluid caused severe burning and irritation to the patient’s eyes,9 and another patient contracted chemical conjunctivitis from residual glutaraldehyde on an anesthesia mask.10 If ethylene oxide, a common cleaning solution, adheres to reusable surfaces, it can cause serious mucosal injury. Water added to ethylene oxide forms ethylene glycol, a known irritant. Residual glutaraldehyde on an improperly rinsed laryngoscope blade caused massive tongue swelling and life-threatening allergic glossitis.11 Care must be taken to thoroughly rinse the suction channel of a fiberoptic bronchoscope (FOB) after cleaning. Residual agents may drip out of the FOB port into the larynx or trachea, causing severe chemical burns.
2 Mechanical Difficulties
A mask is typically applied to a patient’s face before induction of general anesthesia. Preoxygenation of the patient is the first step in securing the airway. The mask should be applied during spontaneous breathing, before drugs are given. During placement, direct contact of the rigid parts of the mask with the bridge of the nose or mandible should be avoided because they are at particular risk for compromised blood flow.11 Bruising and soft tissue damage may occur in these regions with excessive pressure, and pressure damage to the mental nerves as they exit from the foramina has been implicated in lower lip numbness in two patients.12 Care must be taken to avoid contact with the eyes to prevent corneal abrasions, retinal artery occlusions, and blindness. As induction proceeds, firmer mask pressure and stronger lifting pressure on the angle of the mandible become necessary to maintain a tight mask fit and secure the airway. Pressure on the soft tissue of the submandibular region may obstruct the airway, especially in small children, or it can damage the mandibular branch of the facial nerve, resulting in transient facial nerve paralysis.13
Positive airway pressure can force air into the stomach instead of the trachea, producing gastric distention, difficult ventilation, and increased likelihood of regurgitation. Cricoid pressure can help to reduce the amount of air being forced into the stomach. The ability to achieve adequate mask ventilation should be assessed preoperatively. Independent risk factors for difficult mask ventilation are the presence of a beard, increased body mass index, lack of teeth, age older than 55 years, history of snoring or sleep apnea, limited mandibular protrusion test, male gender, Mallampati class III or IV (used to predict ease of intubation), and airway masses or tumors.14
Laryngoceles may manifest as or cause upper airway obstruction during induction of anesthesia. Congenital factors contribute to development of laryngoceles, and persons who play wind instruments also may be at risk because high intrapharyngeal pressures can weaken soft tissue and cause laryngoceles in the lateral pharynx.15,16
3 Prolonged Mask Ventilation
Because mask ventilation offers no protection against silent regurgitation, the anesthesiologist should be vigilant for questionable airway noise, coughing, or bucking. Transparent masks allow visualization of the mouth and early identification of vomitus. Extra care should be taken to avoid undue pressure on vulnerable parts of the face. When continuous positive airway pressure (CPAP) is applied to patients with basilar skull fractures, pneumocephalus may occur.17,18 At least one case report identified positive airway pressure as the cause of bilateral otorrhagia.19
Mask ventilation is relatively contraindicated in nonfasting patients, intestinal obstruction, head-low position, extreme obesity, tracheoesophageal fistula, and massive naso-oropharyngeal bleeding, although it may be life-saving when other airway devices fail. Especially in pediatric cases, it may be necessary to avoid hypoxia.20
B Laryngeal Mask Airway
The laryngeal mask airway (LMA), a device designed for upper airway management, is a cross between a face mask and an ETT. The LMA has been used in millions of patients and has been accepted as a safe technique in many types of surgical procedures. With use of the LMA, muscle relaxation is unnecessary, laryngoscopy is avoided, and hemodynamic changes are minimized during insertion. The LMA has a clear advantage when laryngeal trauma must be minimized (e.g., in operatic singers), when a standard mask fit is impossible, and when light planes of anesthesia are desired.21 It has proved valuable in situations in which mask ventilation is unexpectedly difficult and direct laryngoscopy impossible, and it may be used as a conduit for a fiberoptic intubation with a standard ETT.22 Use of the device is an integral part of the ASA difficult airway algorithm.23
Placing the LMA correctly can be difficult in some patients. The mask may fold on itself, and pressure on the epiglottis can push the device down into the glottic opening, or the epiglottis may become entrapped in the laryngeal inlet of the mask. The tip of the epiglottis may fold into the vocal cords, increasing the work of breathing and producing coughing, laryngospasm, or complete airway obstruction. Excess lubricant can leak into the trachea, promoting coughing or laryngospasm.24 Regardless of the problems encountered in placing the LMA, airway patency is usually maintained. An inadequate mouth opening (<1.5 cm), inadequate anesthesia depth, insertion with a not fully deflated cuff, inadequate size of LMA, inadequate force during insertion, and inadequate volumes for cuff inflation can cause malpositioning of the LMA.
Numerous complications are associated with the LMA. Perhaps the greatest limitation is the inability of the LMA to protect against pulmonary aspiration and regurgitation of gastric contents. Because the LMA does not isolate the trachea from the esophagus, its use is risky when the patient has a full stomach or when high airway pressures are necessary for positive-pressure ventilation. The overall risk of aspiration and regurgitation using the LMA seems to be in the same low range as endotracheal intubation when the indications and contraindications for the LMA are respected.25 The risk of aspiration, which is a consequence of the device’s design, should be weighed against the advantages of the LMA in cases of difficult intubation and ventilation. Other complications have been reported with the use of the LMA. Their incidence and severity depend on the user’s skills and experience, depth of anesthesia, and anatomic or pathologic factors.26
The incidence of sore throat with this device is between 17% and 26%.27 The incidence of failed placement is 1% to 5%, although this rate tends to decrease with increasing operator experience.28 The LMA cuff is permeable to nitrous oxide and carbon dioxide, which results in substantial increases in cuff pressure and volume during prolonged procedures.29,30
Several case reports mention edema of the epiglottis, uvula, posterior pharyngeal wall, and vocal cords; in the worst cases, these conditions have led to airway obstruction.31–33 Nerve paralysis (i.e., lingual, recurrent, hypoglossal, and glossopharyngeal), postobstructive pulmonary edema, tongue cyanosis, and transient dysarthria have been reported. Cuff-pressure control can reduce at least some of these complications.27,34–37 Other problems with the LMA include dislodgment, kinking, and foreign bodies in the tube, leading to airway obstruction.38
Newer designs of the LMA were developed to increase comfort, handling, or safety in various situations. To minimize the risk of aspiration and regurgitation, the ProSeal laryngeal mask airway (PLMA), which has an esophageal vent, was released in 2000.39 It isolates the glottis from the upper esophagus when correctly positioned, which further protects the airway.40,41 Some cases with gastric insufflation with a malpositioned PLMA were reported.42,43
The intubating laryngeal mask airway (ILMA) was designed to overcome unexpected difficult laryngoscopic intubation. Use of the ILMA has been successful in patients with difficult airways.44,45 Tracheal intubation through the ILMA using special ETTs is easier than with the standard LMA, and the success rate for blind insertion of a tube through the ILMA is more than 90%.46,47 Branthwaite reported a case of larynx perforation leading to mediastinitis and the patient’s death.48 Fiberoptically guided insertion of an ETT through an LMA has had the highest success rate for intubation and the lowest rate for damage of laryngeal structures.
Modifications of extraglottic airways combine features of various LMAs. For example, the LMA Supreme combines the Fastrach intubating laryngeal mask airway (ILMA-Fastrach) shape with the PLMA gastric port, resulting in a higher rate of success on first attempt at insertion and lower leak pressures, and the LMA I-Gel supraglottic airway is a single-use device without an inflatable cuff.49,50 Other devices, such as the LMA C-Trach, use integrated fiberoptic channels to visualize the glottic region.51 Overall rates of complications are similar to those described earlier.
Classic contraindications to using an LMA include nonfasted patients, extreme obesity, necessity of high breathing pressures (20 to 25 cm H2O) in the presence of low pulmonary compliance or chronic obstructive pulmonary disease (COPD), acute abdomen, hiatal hernia, Zenker’s diverticulum, trauma, intoxication, airway problems at the glottic or infraglottic level, and thoracic trauma. Nevertheless, the LMA’s successors, particularly those with a channel for the insertion of a gastric tube, have led to more liberal use of LMA devices.52–54
C Esophageal-Tracheal Combitube
The esophageal-tracheal Combitube is an esophagotracheal, double-lumen airway designed for emergency use when standard airway management measures have failed.55,56 Use in elective surgery has been reported.57–60
The device is inserted blindly into the mouth and advanced to preset markings. The distal tube is usually positioned within the esophagus at this point. A distal cuff is inflated within the esophagus, and a large-volume proximal cuff is inflated inside the pharynx. Ventilation is then attempted through the esophageal tube because esophageal intubation occurs in approximately 96% of insertions. If ventilation through this lumen fails, ventilation is attempted through the tracheal lumen. The device is designed for single use, but a study of multiple uses of the Combitube found no problems with the reprocessing.61 Another study warned against reuse because insufficient cleaning may lead to transmission of iatrogenic infections.62
The 37-F (small adult) Combitube is not recommended for patients shorter than 120 cm, and the 41-F Combitube is not recommended for patients shorter than 150 cm. Disregarding those recommendations may induce serious esophageal injury. Further contraindications to using a Combitube are intact gag reflexes, ingestion of caustic substances, known esophageal disease, airway problems at the glottic or infraglottic level, and latex allergy.56
Complications have been reported with use of the Combitube. In two patients, the device was inserted too far, causing the large pharyngeal cuff to lie directly over the glottis and obstruct the upper airway.63 This was easily resolved by partially withdrawing the Combitube until breath sounds were auscultated. Tongue discoloration has been reported while the pharyngeal cuff was inflated, but it usually resolves immediately without further adverse sequelae after the cuff is deflated. The Combitube has been linked to glossopharyngeal and hypoglossal nerve dysfunction, esophageal rupture, subcutaneous emphysema, pneumomediastinum, pneumoperitoneum, and tracheal and esophageal injury and bleeding.64–66 Esophageal lacerations were most likely caused by incorrect use; in both cases, the distal cuff was overblocked, and the larger Combitube (41 F) was used in a small patient. Despite their disadvantages, the Combitube and the EasyTube are widely accepted as devices for managing the difficult airway.
D Other Supraglottic Airway Devices
Many devices are available for managing the airway at the supraglottic level: cuffed oropharyngeal airway (COPA), laryngeal tube (LT), LaryVent, glottic aperture seal airway (GO2 airway), Cobra perilaryngeal airway (CobraPLA), and King Laryngeal Tube Suction (LTS).67–69 Overall, they seem to cause complications and physiologic alterations similar to those found with the LMA.70,71 The devices were designed for separating the airway from the esophageus but do not efficiently protect the airway from regurgitation and aspiration. They share several advantages and disadvantages. Contraindications include nonfasted patients, gastroesophageal reflux, hiatal hernia, pregnancy, obesity, reduced pulmonary compliance, glottic and infraglottic stenosis, and a mechanical obstruction of the oropharynx. Most complications arise from dislodgment, overblocking the cuff, and insufficient depth of anesthesia. Most of the devices were developed in the past few years, and acceptance in routine practice has varied.
III Complications with Intubation
A Endotracheal Intubation
1 Anatomic Requirements
Successful oral intubation requires four anatomic traits: adequate mouth opening, sufficient pharyngeal space (determined by visualization of the hypopharynx), compliant submandibular tissue (determined by measuring the thyromental distance), and adequate atlanto-occipital extension.72 If the patient’s anatomy is compromised in any of these factors, intubation will be difficult. For optimal conditions, a free view to the vocal cords is necessary, and introduction of the ETT should be easily performed.
The pharyngeal space may be limited by tumors, abscesses, edema, and surgical or traumatic disruption. If the anatomy is distorted, the anesthesiologist must optimize the view of the vocal cords. Awake intubation may be necessary, and it should be considered whenever the pharyngeal space is limited. If direct laryngoscopy is performed, the patient should be placed in the sniffing position, and a styletted ETT should be considered. Every effort—backward-upward-rightward pressure (BURP) or optimal external laryngeal manipulation (OELM)—should be made to optimize visualization and identification of the laryngeal and pharyngeal structures.73,74
2 Laryngoscope Modifications and Rigid Optical Instruments
Obtaining a view of the vocal cords with a conventional laryngoscope requires optimal positioning of the patient. With a flexible fiberscope, positioning is not an issue, and damage to the teeth is less likely. Similarly, with innovations such as the Glidescope video laryngoscope, Airtraq laryngoscope, McGrath video laryngoscope, Pentax Airway Scope (Pentax AWS), and Truview video laryngoscope, a video image of the oropharynx and the laryngeal inlet is transmitted from the camera in the tip of the blade and allows laryngoscopy and intubation in positions other than the sniffing position. The advantages of these instruments help to reduce the number of difficult or failed intubations and the incidence of dental damage. In studies on mannequins or patients with normal airways, these devices have been evaluated as better than or equal to the Macintosh laryngoscope, and data demonstrate successful intubation of patients with known or suspected difficult airways.75,76 Although visualization of the vocal cords has become easier, insertion of the intubation tube can be tricky. The monitor view reveals only the laryngeal inlet, and advancing the tube into the larynx may requires an introducer or a built-in guiding channel, which can make the instrument bulky and the technique more complicated than with a conventional laryngoscope. Several cases of pharyngeal injuries have been reported with the rigid stylet of the Glidescope .77 Increased awareness of potential complications, better training and supervision, and appropriate equipment and patient selection can reduce the incidence of complications.
Laryngoscopy requires deep anesthesia because it causes strong stimulation of physiologic reflexes, and respiratory, cardiovascular, and neurologic adverse effects are possible.78 Hypertensive patients, pregnant patients with hypertension, and patients with ischemic heart disease are particularly at risk. Deep anesthesia, application of topical anesthetics, prevention of the sympathoadrenal response with drugs such as atropine or intravenous lidocaine, and minimizing mechanical stimulation can attenuate the adverse effects.
Laryngoscopes have been modified to optimize visualization of the vocal cords. The Corazelli-London and McCoy-Mirakuhr flexible-tip blades may achieve a better view of the glottis by drawing the epiglottis up.79
Rigid optical instruments such as the Bonfils retromolar intubation fiberscope and its modifications,80 the Bullard laryngoscope, and the intubation tracheoscope81 are not commonly used in anesthesiology. They require skilled handling, and experience should be gained in routine cases to apply to difficult airway situations. The rigid intubation tracheoscope, a familiar device in ear, nose, and throat surgery, has special indications and may be useful in the hands of anesthesiologists. Available in two sizes (child and adult), it consists of a battery-filled handle and a straight, rigid tube with a connection to a breathing bag or circuit. The rigid tracheoscope is useful for tumors, scars, and abscesses in the oropharynx, base of the tongue, and larynx and for aspirated foreign bodies.
The disadvantages of these instruments are a relatively closed view through the tube, a high risk of damage to the teeth and laryngeal structures, possible perforation of the hypopharynx, and risk of aspiration. High-flow oxygen insufflation through a port induced subcutaneous cervical and facial emphysema in one patient.82
3 Difficult Intubation
Despite optimal positioning of the head and neck, the glottis is sometimes impossible to visualize, even in patients without obvious predisposing features.83–85 Risk factors for difficult tracheal intubation include male sex, age between 40 and 59 years, and obesity.72 Anesthesiologists should be aware of the potential for a difficult intubation in the following circumstances:
• Posterior depth of the mandible greater than 2.7 cm (which limits submandibular displacement of the soft tissues)
• Anterior depth of the mandible greater than 4.8 cm
• Correlation between effective length of the mandible and a posterior depth less than 3.6
• Distance between the occiput and spinous process of C1 of about 2.6 mm
• Distance between the spinous processes of C1 and C2 of about 2.6 mm (which narrows the limits of head extension)
• Longer maxilla with protruding teeth
• Caudally positioned hyoid bone (increasing the mandible-hyoid distance)
• More rostrally positioned angle of the mandible (a phenotypical receding mandible)83,86–89
A chin-to-thyroid cartilage distance of less than three finger breadths (about 7 cm) hampers visualization of the glottis.90 A combination of tests may increase the predictive value of the preanesthesia examination results.6,7 Causes for difficulty in securing the airway are shown in Box 51-1.25,91 Computerized analysis of facial structure provides an accurate approach to predicting difficult intubation.92 Patients who proved difficult to intubate should be told about it and given written documentation so that they can notify future anesthesiologists. Patients should be registered with the MedicAlert Foundation.
Box 51-1
Miscellaneous Causes of Difficult Securing of the Airway
Diseases
Limited temporomandibular joint mobility
Limited atlanto-occipital and atlantoaxial joint mobility
Postoperative or post-traumatic rigidity of the soft tissue of mouth and neck
Congenital, postoperative, post-traumatic anomalies of face and neck
Abscesses and tumors in face and neck
Modified from Krier C, Georgi R: Airway management: Is there more than one “gold standard”? Anasthesiol Intensivmed Notfallmed Schmerzther 36:193–194, 2001.
4 Nasotracheal Passage
a Cranial Intubation
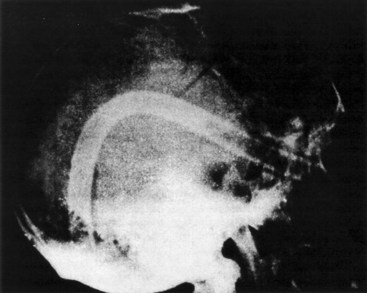
Nasotracheal intubations are potentially hazardous. In patients with basilar skull fractures or certain facial fractures (e.g., LeFort II or III fractures), the ETT may be inadvertently introduced into the cranial vault (Fig. 51-1).93 Fractures of the frontal part of the skull base with cerebrospinal rhinorrhea, intranasal abscesses or abscesses with intranasal expansion, choanal atresia, hyperplastic tonsils, tendency to uncontrollable nasal bleeding, and coagulopathies are considered contraindications to nasotracheal intubation. In a case of nasotracheal intubation, asystole occurred after the tube was introduced into the orbit.94 However, if care is taken, the complication rates of oral and nasal intubation are not different.95 Nasal intubation in a patient with a known or suspected skull fracture should be performed only by using fiberoptic bronchoscopy and with extreme caution in the inferior nasal meatus. For midfacial fractures with intact dura mater, it is possible to open the dura by manipulation during nasotracheal intubation.
b Nasal Injury
Nasotracheal intubation may be problematic in the presence of hypertrophic turbinates, extreme deviation of the nasal septum, prominences on the nasal septum, chronic infections in the nasal cavity, and nasal polyposis. Minor bruising occurs in 54% of nasal intubations and most commonly involves the mucosa overlying the inferior turbinate and the adjacent septum.96 If epistaxis occurs, the ETT cuff should be inflated and remain in the nostril to tamponade the bleeding.
The nasal mucosa must be vasoconstricted before instrumentation.97 Some agents used for this purpose are 0.5% phenylephrine in 4% lidocaine or 0.1% xylometazoline. A 4% solution of cocaine may be associated with severe adverse effects and is no longer recommended for vasoconstriction. The risk of nasal injury can be minimized with the use of a small, well-lubricated ETT with a flexible tip that has been soaked in warm water.98
Possible complications of nasotracheal intubation are dislodgment of nasal polyps,88 dislodgment of nasal turbinates,99,100 adenoidectomy, injury of the nasal septum, perforation of the piriform sinus, and the epiglottic vallecula. In case of injury to the piriform sinus, the internal branch of the superior laryngeal nerve, soft tissue of the pharynx, the larynx, and the superior laryngeal vessels may be damaged. Tears in the pharyngeal mucosa can mature into retropharyngeal abscesses.101 Nasotracheal tubes may dissect and run behind the posterior pharyngeal wall. Patients with an obstructed nasal passage due to convoluted turbinates are at increased risk for this complication. One case of external compression of the nasotracheal tube due to the displaced bony fragments of multiple Le Fort fractures was reported.102
Even without gross trauma, mechanical damage to the superficial epithelial layers caused by nasal intubation results in mucociliary slowing in 65% of patients and bacteremia in another 5.5%.103,104 The most common organisms introduced into the blood are nasopharyngeal commensal organisms (e.g., Streptococcus viridans), which can cause endocarditis and systemic infection. Even short-term intubation has caused nasal septal and retropharyngeal abscesses. Acute otitis media has occurred in 13% of nasally intubated neonates.105 Paranasal sinusitis has been reported, most commonly occurring with nasal intubation for more than 5 days.106,107 Infection may be related to sustained edema and occlusion of the sinus drainage pathways. Prompt diagnosis is critical, and paranasal sinusitis should be suspected in any patient with facial tenderness, pain, or purulent nasal discharge or in any nasally intubated patient who develops sepsis with no other obvious source. A careful examination of the patient is necessary, but the success of a previous cosmetic operation should not be endangered. The nasal structures must be checked again postoperatively.
c Foreign Bodies
The nostrils are common sites for entry of foreign bodies. Small children, known for placing small objects into their orifices, find the nostrils one of the most accessible sites. More than 80% of patients who aspirated a foreign body are children, and most were between 1 and 3 years old.108–110 Foreign body aspiration is the cause of death of 7% of children younger than 4 years.
Smith and colleagues reported a rhinolith that was dislodged during nasotracheal intubation.111 The mass had formed around the rubber tire of a toy car that the patient had placed in his nose 30 years earlier. Nasotracheal intubation can dislodge similar foreign bodies that may obstruct the ETT, pharynx, or trachea. If a nasal foreign body is known or suspected, it should be gently dislodged, advanced into the oral pharynx, and retrieved before intubation. Mask ventilation may also dislodge foreign bodies to the lower parts of the airway.
5 Traumatic Intubation
b Dental Trauma
The incidence of dental injuries associated with anesthesia is greater than 1 case in 4500 procedures.112 Maxillary central incisors are most at risk; 50% of these injuries happen during laryngoscopy, 23% after extubation, 8% during extubation, and 5% in the context of regional anesthesia. Dental injuries are also associated with the use of LMAs and oropharyngeal airways. With insufficient anesthesia, depth biting against the tube is possible. Dental injuries are most common in small children, patients with periodontal disease (in which structural support is poor) or fixed dental work (e.g., bridges, capped teeth), protrusion of the upper incisors (i.e., overbite), carious teeth, and cases of difficult intubation. Preexisting dental pathology should be explored, and all loose, diseased, chipped, or capped teeth must be documented in the chart before anesthesia induction and intubation.113 The patient must be advised of the risk of dental damage. Tooth guards may be used, but they can be awkward and obstruct vision,114 although the time for intubation is not significantly longer.115
Fragments of chipped or partially broken teeth and completely avulsed teeth should be located and retrieved. Care should be taken to ensure that no foreign bodies slip into the pharynx to later become lodged in the esophagus or the larynx. Avulsed teeth should be saved in a moist gauze or in normal saline without cleaning them. Tooth aspiration may cause serious complications requiring rigid or flexible bronchoscopy for removal. With a rapid response from an oral surgeon or a dentist, an intact tooth often can be reimplanted and saved. The optimal time is within the first hour; thereafter, reimplantation success diminishes with increasing time.116
c Tongue Injury
Massive tongue swelling, or macroglossia, has been reported in adult and pediatric patients.117,118 Some cases occurred while a bite block was in place, some happened with an oral airway and soft tissue compression of the chin, and some occurred with no protective device. The common denominator was that they all occurred when there was substantial neck flexion during endotracheal intubation and surgery was prolonged. Macroglossia results from obstructed venous and lymphatic drainage of the tongue, and it has been associated with angiotensin-converting enzyme inhibitors.119 In each case, the ETT might have severely compromised the circulation on the affected side of the tongue. One report described the sudden onset of tongue swelling after prolonged surgery to repair a cleft palate,120 during which the tongue was retracted extensively. Obstruction of the submandibular duct by an ETT may lead to massive tongue swelling.121 Reduced sense of taste, cyanosis, or loss of tongue sensation is possible after compression of the lingual nerve or by lingual artery compression during forced intubation or associated with an oversized, malpositioned, or overinflated LMA.
d Damage to the Uvula
Uvula trauma is usually associated with the use of ETTs, oropharyngeal and nasopharyngeal airways, LMAs,122 or Combitubes and with overzealous blind use of a suction catheter.123 The results of damaging the uvula are edema and necrosis.124 Sore throat, odynophagia, painful swallowing, coughing, foreign body sensation, and serious life-threatening airway obstruction are reported.125
e Pharyngeal Mucosal Damage
A postoperative sore throat (POST) likely represents a broad constellation of signs and symptoms. The incidence of POST after intubation is higher than POST after LMA use and after face mask ventilation.126,127 The incidence of sore throat associated with the use of the Combitube was 48%.128 Aggressive suctioning is probably a mitigating factor. The incidence is substantially higher in women and in patients undergoing thyroid surgery. No correlation was seen with factors such as age, use of muscle relaxants, type of narcotic used, number of intubation attempts, or duration of intubation. Small tube and cuff size and topical treatment and inhalation of steroids have a positive impact on POST.129 However, pain on swallowing usually lasts no more than 24 to 48 hours and can be relieved in part by having the patient breathe humidified air.
f Laryngeal Trauma and Damage to the Vocal Cords
Trauma to the larynx may occur after endotracheal intubation. It depends on the intubator’s skill and the degree of difficulty. In one large study, 6.2% of patients sustained severe lesions, 4.5% had hematoma of the vocal cords, 1% had hematoma of the supraglottic region, and 1% sustained lacerations and scars of the vocal cord mucosa.130 Recovery typically is prompt with conservative therapy.131 Hoarseness may appear 2 weeks postoperatively.132
Granulations usually occur as a complication of long-term intubation. However, a small but significant number of patients sustain laryngeal injuries during short-term intubation.133 Intubation can cause various degrees of laryngeal trauma, including thickening, edema, erythema, hematoma, and granuloma of the vocal folds.134,135 Injuries of the laryngeal muscles and suspensory ligaments are possible. The larynx should be inspected for injury before insertion of the ETT to document and treat preexistent lesions. Anesthesiologists should be vigilant in all cases of hoarseness, and patients should be examined by an otorhinolaryngologist preoperatively.
Arytenoid dislocation and subluxation have been reported as a rare complication of intubation.136 Mitigating factors include traumatic and difficult intubations, repeated attempts at intubation, and attempted intubation using blind techniques such as light-guided intubation,137 retrograde intubation, and use of the McCoy laryngoscope.138 Early diagnosis and conservative or operative treatment are necessary,139 because fibrosis with subsequent malpositioning and ankylosis may occur after 48 hours.
The vocal process of the arytenoid is the most common site of injury by the ETT because it is positioned between the vocal cords. Granuloma formation most commonly occurs at this site. The degree of injury worsens with increasing tube size and duration of intubation.140
Many investigators have reported unilateral or bilateral vocal cord paralysis after intubation, which is usually temporary.141–144 One report associated vocal cord paralysis with use of ethylene oxide to sterilize ETTs.145 Hoarseness occurs with unilateral paralysis, whereas respiratory obstruction occurs with bilateral problems. The most likely source of injury is an ETT cuff malpositioned in the subglottic larynx with pressure on the recurrent laryngeal nerve.142,143 Permanent voice change after intubation because of external laryngeal nerve trauma has been reported in up to 3% of patients undergoing surgery at sites other than the head or neck. The incidence may be decreased by avoiding overinflation of the ETT cuff and by placing the ETT at least 15 mm below the vocal cords.142 Eroded vocal cords may adhere to one another, eventually forming synechiae. This is a potential problem when airflow between the vocal cords has been compromised as a result of tracheostomy.146 Surgical correction is usually necessary.
g Tracheobronchial Trauma
Tracheal trauma has many causes.147 Injury may result from an overinflated ETT cuff, inadequate tube size, or malpositioned tube tip, laryngoscope, stylet, tube exchanger, or related equipment. Predisposing factors include anatomic difficulties; blind or hurried intubation; inadequate positioning; poor visualization; and most commonly, inexperience of the intubator. The presence of an ETT may lead to edema, desquamation, inflammation, and ulceration of the airway.148 The severity of the injury may be related to the duration of intubation, although this relationship is not well established.149 Any irritating stimulus, such as pressure from an oversized ETT, dry inhaled gases, allergic reactions to inhaled sprays, or chemical irritation from residual cleaning solutions, can initiate an inflammatory response and cause mucosal edema in the larynx or trachea. Edema after extubation limits the lumen diameter and increases airway resistance. Small children are most susceptible to this problem, in which a sudden increase in airway resistance results from laryngotracheobronchitis or croup. Almost 4% of children 1 to 3 years old develop croup after tracheal intubation.150,151 Mechanical trauma may result from sharp objects within the trachea, such as a stylet tip that extends beyond the length of the ETT. Tracheal ruptures, especially after emergency intubation, were reported.152 One case of a bronchial rupture caused by an ETT exchanger was reported.153
ETT cuffs inflated to a pressure greater than that of the capillary perfusion may devitalize the tracheal mucosa, leading to ulceration, necrosis, and loss of structural integrity.154 Ulceration can occur at even lower pressures in hypotensive patients. The need for increasing cuff volumes to maintain a seal is an ominous sign that heralds tracheomalacia.155 Massive gastric distention in an intubated patient may signal the presence of a tracheoesophageal fistula as the cuff progressively erodes into the esophagus.156 Any patient with more than 10 mL of blood in the ETT without a known cause should be assessed for a tracheocarotid fistula.157 The various nerves in this region of the neck are also at risk. Erosion of the ETT into the paratracheal nerves may result in dysphonia, hoarseness, and laryngeal incompetence. Tracheomalacia results from erosion confined to the tracheal cartilages. The anesthesiologist must inflate the ETT cuff only as much as necessary to ensure an adequate airway seal. When nitrous oxide is used during a lengthy surgical procedure, the pressure in the cuff should be checked by a cuff pressure control device. In the presence of 70% nitrous oxide, intracuff pressures take an average of 12 minutes to increase to levels that are potentially high enough to cause tracheal ischemia.154 The cuff pressure should not exceed 25 cm H2O. Increasing cuff pressure caused by surgical manipulations can be observed and prevented by using a cuff pressure control device.
Tracheal intubation may erode the tracheal mucosa, leading to scar tissue, which ultimately retracts and leads to stenoses of the trachea, larynx, or nares. The reported incidence of granulomas is 1 case in every 800 to 20,000 intubations.158,159 They are more common in women than in men and occur rarely in children. The most common site of erosion is along the posterior laryngeal wall, where granulation tissue easily overgrows. Side effects of granulomas include cough, hoarseness, and throat pain. The growths may be prevented by minimizing the trauma associated with laryngoscopy and intubation. When granulomas occur, surgical excision is usually required.
Several months after prolonged tracheal intubation, tracheal stenosis and fibrosis may occur. This usually represents the end stage of a progression from tracheal wall erosion to cartilaginous weakening to healing with fibrosis.147 Stenoses typically occur at the site of an inflated cuff, although they may occur at the ETT tip. Symptoms include a nonproductive cough, dyspnea, and signs of respiratory obstruction. Dilation of the stenosis is curative in its early stages. However, surgical correction may be necessary after the tracheal lumen has been reduced to 4 to 5 mm.160,161
h Barotrauma
Barotrauma results from high-pressure distention of intrapulmonary structures. High-flow insufflation techniques in which small catheters are used distal to the larynx are most often associated with barotrauma. These problems are common in microlaryngeal surgery when jet ventilation is used.162–166 Direct impingement of the catheter tip on the tracheal mucosa may also cause barotrauma.164 Edema or hematoma may occur if the jet of air strikes the mucosa of the larynx or the vocal cords, leading to laryngospasm. When air leaks into the peribronchial tissues, it can traverse into the subcutaneous space, the lung interstitium, or the pleural and pericardial cavities. Pneumomediastinum or tension pneumothorax and possibly tamponade are the results, and chest tubes may be necessary. Progressive accumulation of air may cause loss of pulmonary compliance, loss of ventilatory volume, or if the accumulation is large enough, overdistension of lung tissue with cardiopulmonary compromise and, finally, impossible ventilation. Safety mechanisms should be in place to prevent high-pressure airflow in the event that intrapulmonary pressures become excessive. For diseased pulmonary tissue, the least possible airway pressure should be used to prevent parenchymal blowout. This advice also applies to patients with blunt thoracic trauma who have subcutaneous emphysema. They should be presumed to have a bronchial leak unless proved otherwise. Barotrauma may also result from upper airway obstruction during jet ventilation.167
i Nerve Injuries
Laryngoscopy and cuffed supraglottic airway devices may cause periodic or permanent nerve injury. Lingual, recurrent, hypoglossal, and glossopharyngeal nerve paralysis have been described for LMA devices, and neuropraxia with weakness, numbness, or paralysis of the tongue can occur after laryngoscopy.34 After damage to the internal branch of the superior laryngeal nerve during a difficult intubation, two patients had signs of aspiration.168
Malposition of the cuff or tube may be one reason for this rare damage. Ahmad and Yentis postulated that lingual nerve injury may occur where the nerve distal to its gingival branch is compressed by the LMA tubing against the side of the tongue.169 In addition to the cases previously described, we observed one case of permanent anosmia after nasotracheal intubation with no pathologic findings.
j Spinal Cord and Vertebral Column Injury
Airway managing techniques such as chin lift, jaw thrust, and direct laryngoscopy transmit movement to the cervical spine. When a patient’s neck is fused, adequate neck extension may be impossible to obtain. Attempting to hyperextend the necks of these patients may result in cervical fractures and quadriplegia.170 A head that is fixated in a cervical collar or halo does not allow neck extension and limits the successful use of direct laryngoscopy. Using a fiberoptic device to assist intubation should be considered in these cases. If immediate intubation is necessary, patients with an acute fracture of the back and neck may be supported by in-line cervical stabilization during careful intubation while protecting the head against excessive movement and fixing it in a safe position by a second person.171 C1 and C2 fractures seem to be particularly vulnerable because any degree of extension may compromise spinal cord function. Between 10% and 25% of spinal cord injuries occur because of improper immobilization of the vertebral column after trauma, and neurologic deterioration was associated with direct laryngoscopy in a patient with a cervical spine injury.172–175
Several conditions, such as Down syndrome and rheumatoid arthritis, are associated with atlantoaxial instability.176,177 Excessive neck extension in a patient with an undiagnosed Arnold-Chiari malformation may cause worsening of cerebellar tonsil herniation.178 Patients with underlying diseases such as connective tissue disorders, lytic bone tumors, and osteoporosis should be intubated carefully, and extreme neck extension should be avoided in every patient because of loss of muscle tone by curarizing drugs. A range-of-motion test and an assessment of neck extension should be performed before inducing anesthesia. A case of quadriplegia after bag-ventilation, direct laryngoscopy, and cricothyrotomy in a patient with an unrecognized cervical spine injury was reported.175 Hastings found in a review of records of 150 patients with unstable cervical spine injury a 1.3% incidence of neurologic deterioration after elective surgery with tracheal intubation. Inadequate airway management may result in disaster of permanent spinal cord injury. Awake fiberoptic intubation should be considered when neck extension cannot be achieved without the risk of damage and time is not crucial. It is considered the safest method for airway management in patients with cervical spine injury, followed by LMA and the Combitube.171
k Eye Injuries
The ASA Closed Claims Project reported that the eye injuries were responsible for 3% of all claims; of these, 35% were related to corneal injuries, with corneal abrasions being the most common eye complication.179 They are primarily caused by a face mask being placed on an open eye or by the eyelids not being completely closed during anesthesia.180,181 Jewelry, identification cards, and loose-fitting watch bands have been implicated in scratching the eyeball.182 A stethoscope hanging from the neck of a clinician can fall forward and strike the patient’s eyes or forehead. Prevention consists of vigilance on the part of the anesthesiologist and application of adhesive tape over the closed eyelids. Especially during head and neck surgery, the eyelids should be taped closed, and the eyes should be covered carefully with soft eyepads.183 Some clinicians routinely apply lubricating ointment to the inside of the eyelids, although this has not been proved to increase efficacy.
l Temporomandibular Joint Injuries
TMJ anatomy is special in that one side cannot be moved without the other side. Both joints represent a functional unit, and injuries to one TMJ affect the other side. Opening the mouth is a combination of rotary and translational movement in the joint. The rotary movement allows only a mouth opening of about 25 mm; the maximal opening is achieved by the translational movement. Pathologic changes such as bone cysts, rheumatid arthritis, and atrophy of the mandible due to age can reduce the joint mobility and may lead to fractures. Rupture of the lateral ligament is possible. TMJ injuries are caused by increasing forces during laryngoscopy to optimize the view of the vocal cords. Limited mouth opening, pain in the joint, lateral deviation of the mandible (e.g., unilateral luxation), protrusion of the mandible (e.g., bilateral luxation), and lockjaw (e.g., fixation after joint luxation) may occur. Most reported cases of TMJ injury were not associated with difficult airway.184
m Damage to the Nose
Some injuries to the nose and endonasal structures were described previously. Using anatomically preformed tubes for head and neck surgery or compression of the nasal wing may lead to necrosis in the worse cases (Fig. 51-2). Wrapping the tube with foam material at the nasal wing level and careful nursing in cases of long-term intubation may reduce or avoid this complication.
6 Esophageal Intubation
a Endotracheal Tube Placement
When visualization of the glottis is difficult, the ETT may inadvertently be introduced into the esophagus. Esophageal intubation is more common among inexperienced practitioners, but it may also occur in the hands of experienced stuff members. Intubating the esophagus is not disastrous, but failing to detect and correct the condition is. Recognition of this error must be rapid to avoid the adverse effects of prolonged hypoxia. A closed claims analysis of adverse anesthesia events reported that 18% of respiratory-related claims involved esophageal intubation.185 Preoxygenation can help alleviate this problem by allowing a longer apneic period for tracheal intubation and by delaying the onset of hypoxemia. End-tidal CO2 capnography is essential in confirming endotracheal placement of the tube. Capnography should be available wherever intubation is performed. In out-of-hospital practice and emergency medicine, where capnography may not be available, calorimetric single-use CO2 detectors or an esophageal detector device can help to identify failed intubation in 94.6%.186 Esophageal intubation can briefly produce an end-tidal CO2 capnogram (e.g., in presence of CO2-containing drinks in the stomach), but the waveform diminishes rapidly after three to five breaths.187,188 Fiberoptic control is another safe way to confirm the correct position of the tube. Other signs, such as equal bilateral breath sounds, symmetrical bilateral chest wall movement, epigastric auscultation and observation, and tube condensation, are potentially misleading.189 A misplaced tube should remain in place while the trachea is correctly intubated. This helps to identify the correct orifice for intubation and protects the trachea from invasion by regurgitated stomach contents. Once proper endotracheal intubation is achieved after an esophageal intubation, the stomach should be suctioned to minimize vomiting, gastric perforation, or compromise of ventilation.
b Esophageal Perforation and Retropharyngeal Abscess
Perforation of the esophagus has been reported on several occasions.190–198 It seems most likely to occur when inexperienced clinicians handle emergency situations, when intubation is difficult, or in presence of esophageal pathology. Perforation occurs most commonly over the cricopharyngeus muscle on the posterior esophageal wall, where the esophagus is narrow and thin. Subcutaneous emphysema, pneumothorax, fever, cellulitis, cyanosis, throat pain, mediastinitis, empyema, pericarditis, and death can occur. Early detection and treatment of the condition are critical because the mortality rate of mediastinitis is more than 50%. An esophageal perforation should be suspected in any patient with a fever, sore throat, and subcutaneous emphysema after a difficult intubation.
A case report identified a traumatic tracheal perforation through the esophagus in a patient with a difficult intubation.199 Cases of esophageal perforation have been associated with the use of an esophageal-tracheal Combitube.65,66
7 Bronchial Intubation
a Use of an Endotracheal Tube
Bronchial intubation is common and sometimes difficult to identify. Asymmetrical chest expansion, unilateral absence of breath sounds (especially on the left side), and eventual arterial blood gas abnormalities are diagnostic features. Bronchial intubation (preferentially right-sided) is more common in newborns and children, because of the small distance between the carina and the glottis. The position of the tip of the tube should be carefully monitored in children. If bronchial intubation goes undetected, it may lead to atelectasis, hypoxia, and pulmonary edema.200 Transillumination of the neck with a lightwand can assist in tube location,201 although not in cases of obesity and large goiter. Fiberoptic control is the best tool to detect proper position of the tube. The ETT may be deliberately advanced into a main stem bronchus and withdrawn until bilateral breath sounds are auscultated.
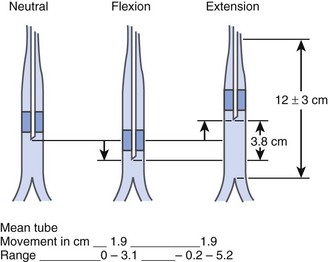
The tip of the ETT may move between 3.8 and 6.4 cm during flexion or extension of the patient’s head as the patient is positioned for surgery (Fig. 51-3).202 It is easy to remember that the tip of the ETT moves in the same direction as the patient’s nose. If the patient’s neck is flexed, the nose is pointed downward, and the ETT advances farther into the trachea. The tube moves away from the carina an average of 0.7 cm during lateral rotation of the head. Care should be taken in case of cleft palate surgery or tonsillectomy. Special blades used by the surgeon to achieve a direct view may move the ETT forward during positioning the blade. A stethoscope placed on the left chest helps to identify an endobronchial tube that is being displaced.
When inadvertent bronchial intubation is discovered, the tube should be withdrawn several centimeters and the lungs inflated sufficiently to expand any atelectatic areas. In cases of chronic atelectasis, bronchoscopy may be required to remove mucous plugs. This problem can be avoided by measuring the length of the ETT alongside the patient before intubation. The tip of the tube should ideally be at least 2 cm above the carina, which may be approximated at the sternal angle (of Louis) adjacent to the junction of the sternum with the second rib. Appropriate orotracheal tube depths are 21 cm from the teeth in adult women and 23 cm in adult men, and nasotracheal tube depths are 25 cm in women and 27 cm in men from the nares.203
b Use of A Double-Lumen Tube
Safe limits for the placement of double-lumen tubes have been outlined by Benumof and colleagues.204 Modern FOBs have removed the guesswork surrounding endotracheal-bronchial tube tip location. The double-lumen tube may be inserted blindly into the appropriate bronchus, followed by bronchoscopic confirmation of its position, or the bronchoscope may be inserted initially and used as a stylet over which the double-lumen tube is advanced. Fiberoptic bronchoscopy significantly reduces malposition of the double-lumen tube, and its routine use is recommended after intubation, changing patient’s position, increasing ventilation pressure, and irregular auscultation sounds. However, even in the best of hands, tracheobronchial injuries occur.205 Bronchial rupture is a serious complication that requires immediate attention. Using double-lumen tubes that are too large may be the cause of bronchial trauma.206 The 37- to 39-F double-lumen tubes are recommended for women, and the 39- to 41-F tubes are recommended for men.
B Maintenance of the Endotracheal Tube
1 Airway Obstruction
A patent airway is an absolute requirement for safe anesthesia. Airway obstruction can occur at any time during administration of general anesthesia, particularly in prolonged operations or in patients with predisposing anatomic abnormalities. Airway obstruction should be considered when an intubated patient has diminished breath sounds associated with increasing peak inspiratory pressures. Obstruction can result from diverse factors,207 including a sharp bend or kink in the ETT, a tube that has been bitten closed, or a tube that is obstructed with mucus, blood, foreign bodies, or lubricant.208,209 The ETT may become warm with continued use during prolonged procedures; under these circumstances, the tube may kink and become obstructed. Many clinicians mistakenly treat the patient for bronchospasm when the turbulent air movement comes from the ETT, not from the patient. At least two cases have been reported in which the plastic coating on a stylet sheared off and occluded the lumen of an ETT.210,211 In another case, a tube was obstructed by the prominent knuckle of an aortic arch.212 Nitrous oxide can cause expansion of gas bubbles trapped in the walls of an ETT, leading to airway obstruction.213
The cuff of an ETT can cause airway obstruction. An overinflated cuff may compress the bevel of the ETT against the tracheal wall, occluding its tip.214 The cuff may also herniate over the tip of the tube and cause an obstruction.215 When faced with any of these problems, the best solution is to pass a suction catheter or an FOB down the lumen of the ETT and attempt to clear it. If the tube is totally obstructed, passage of a stylet may be tried. Total obstruction that cannot be remedied quickly requires removal of the tube, and the patient should be reintubated as rapidly as possible. The ETT and connecting hoses should be supported and, if necessary, taped to prevent kinking caused by their own weight. Inspiratory gases should be humidified during long anesthesia to prevent tube obstruction from dried secretions.
Unusual causes of airway obstruction have been reported. In two patients, complete airway obstruction occurred secondary to achalasia and esophageal dilation.216,217 Two cases of tension hydrothorax that caused airway obstruction during laparoscopic surgery have been reported. The first patient had malignant ascites that, when combined with a pneumoperitoneum, led to a rapid accumulation of pleural fluid with respiratory and cardiovascular compromise.218 The second case occurred during operative hysteroscopy when a large volume of glycine was absorbed through opened myometrial vessels under high intraabdominal pressure.219 In each case, more than 1.5 L of clear fluid was drained once chest tubes were placed.
2 Disconnection and Dislodgment
A common and serious complication of tracheal intubation is disconnection of the ETT from the remainder of the anesthesia circuit. This was identified as the most common critical incident in a study of anesthesia-related human errors and equipment failures.220 A trained anesthesiologist usually identifies this problem immediately. The low-pressure alarm sounds first, and the patient’s breath sounds become absent. However, if the ventilator continues to function normally, the physician may be unaware of the nature of the problem. Disconnections are most likely to occur if the connections are made of dissimilar materials, if the patient’s head is turned away from the anesthesiologist, or if the airway connections are hidden beneath the surgical drapes. Alarms to signal airway disconnection are included on all modern anesthesia machines, and their signals should be taken seriously.
Connections between the ETT and the breathing circuit should be checked and reinforced at the outset, before the anesthesiologist loses visual control of the airway. There should be no tension on the connections from the weight of the corrugated tubing or the drapes on the tubing. Members of the surgical team should be discouraged from inadvertently leaning on any portion of the breathing circuit. The exact site of disconnection should be ascertained rapidly by checking each connection, beginning at the patient’s airway and moving proximally back to the machine.221 Nonetheless, the anesthesiologist must have a prearranged plan in mind in the event that an airway is inadvertently disconnected or dislodged during surgery.
3 Circuit Leaks
Mnemonics such as COVER ABCD–A SWIFT CHECK may help to diagnose and treat the conditions222:
C Circulation, capnograph, and color (saturation)
O Oxygen supply and oxygen analyzer
V Ventilation of intubated patient and vaporizers (include analyzers)
E Endotracheal tube (position, orientation, and patency) and eliminate machine problems
R Review monitors and equipment
A Airway (with face or laryngeal mask)
B Breathing (with spontaneous ventilation)
D Drugs (consider all given or not given)
4 Laser Fires
Lasers are frequently used in the operating room to ablate benign and neoplastic tissues in the airway. The use of special laser-guarded or metal tubes is recommended, and all inflammatory materials such as prosthetic teeth and nasogastric tubes should be removed. One of the most catastrophic events associated with their use is an airway fire, which occurs when the laser ignites the ETT.223–225 The risk that a laser beam will contact the wall of an ETT is 1 : 2.226 Perforation of the tube may occur and produce a blowtorch-like flame. Oxygen-rich inspired gas concentrations fuel brisk ignition of the plastic in the ETT and can fuel a fire in both directions. The ETT acts as a blowtorch; the fire is fed by the combustible walls of the tube and is intensified by the high rate of oxygen flow. The heat and fumes of the burning plastic may cause severe damage to the airway. Treatment consists of immediately disconnecting the circuit from the ETT and removing the burning tube from the airway. If the tube is not burning or if complete loss of the airway may occur with removal of the tube, leaving the tube in situ should be considered. The fire should be extinguished with saline, and the patient should be supported by face mask ventilation. The airway should be evaluated for damage with bronchoscopy, and the appropriate supportive respiratory care should be given.
Many precautions can reduce the risk for an airway fire. If possible, placement of an ETT may be avoided altogether if air can be delivered through a ventilating laryngoscope, a jet ventilation system, or by intermittent apneic ventilation.227 If a tracheostomy tube is in place, ventilation may occur distal to the site of laser surgery. The choice of laser tubes should be consistent with the type of laser used. Blocking cuffs are particularly vulnerable to the laser beam. Covering the tube with saline-soaked gauze or noncombustible tape, using a positive end-expiratory pressure (PEEP) of 5 to 10 cm H2O to prevent aspiration of material in case of cuff puncture, and filling the cuff with saline to act as extinguisher in the event of puncture are measures that can protect the patient’s airway.228,229 Placing a dye, such as methylene blue, in the saline can further alert the anesthesiologist, because in the event of a fire, a stream that is the color of the dye will be emitted.
Nitrous oxide should be avoided because it supports combustion. Oxygen concentrations should never exceed 40% for the same reason.230,231
C Special Techniques
1 Fiberoptic Intubation
Intubation with an FOB should not be attempted when the pharynx is filled with blood or saliva, when inadequate space exists within the oral cavity to identify pharyngeal structures, or when time is critical and creating a surgical airway is the priority. Relative contraindications include marked tissue edema, distortion of the oropharyngeal anatomy, narrowed nasal passages, soft tissue traction, and a severe cervical flexion deformity. Operator experience with the technique and proper preparation are essential. Connecting the device to a video system can help with guidance by a more experienced bystander particularly in training situations.232
Potential complications associated with the FOB include bleeding, epistaxis (especially if a nasal airway is attempted), laryngotracheal trauma, laryngospasm, bronchospasm, and aspiration of blood, saliva, or gastric contents. Another possible hazard is associated with the practice of insufflating oxygen through the suction channel. Although this technique can help to keep the tip of the bronchoscope clean and provide for a high volume of forced inspiratory oxygen, it can also cause high-pressure submucosal injection of oxygen if the tip cuts into the pharyngeal mucosa. If this sequence occurs, the result may be pronounced subcutaneous emphysema of the pharynx, face, and periorbital regions.233
2 Lighted Stylets
The lighted stylet may be used to facilitate intubation under local and general anesthesia. A light at the tip of a flexible stylet is used to transilluminate the soft tissues of the pharynx. The device can be used blindly or as an aid when direct laryngoscopy is difficult. It may also confirm that the tip of an ETT is still within the cervical trachea and establish that the tube has not been advanced too far.234
Several real and potential complications have been reported with the use of this device. Sore throat, hoarseness, mucosal damage, and arytenoid subluxation are possible. Several cases have been reported in which the light fell off of the end of the stylet. In another instance, the protective tubing was not removed from the stylet and had the potential to become dislodged within the trachea. Heat damage to the tracheal mucosa in prolonged intubation is a potential risk with inappropriate handling. To avoid heat damage, the Trachlight’s bulb flashes on and off after 30 seconds.235
3 Submandibular and Submental Approach for Tracheal Intubation
The oral route for tracheal intubation can interfere with some maxillofacial surgical procedures, and the nasal route can be contraindicated or impossible. Nasotracheal intubation is contraindicated in patients with fractures in the cribriform plate of the ethmoid, which frequently accompany Le Fort II and III maxillary fractures, because of the potential complications of infection and the possibility of cranial intubation. Tracheostomy is the usual solution in these circumstances, but it also carries complications. An alternative method is to introduce the tracheal tube through a submental or a submandibular incision, bypassing the surgical area and avoiding the complications of tracheostomy. Damage to adjacent structures with bleeding, tube displacement, aspiration, and hypoxia when passing the tube through a submental excision and infections have been reported.236,237
Iv Complications with Infraglottic Procedures
A Translaryngeal Airway
1 Retrograde Wire Intubation
Retrograde wire intubation is an excellent technique for securing a difficult airway. It can be used when anatomic limitations obscure the glottic opening. Because the technique is blind, it is important to exercise caution and not worsen any preexisting conditions. The technique has variations, such as using the FOB by passing the wire through the suction channel or through a tube exchanger.238
Although simple in concept, the basic technique has numerous problems and potential complications. The procedure takes some time to perform and should not be considered under emergency circumstances unless the practitioner is very experienced. The tip of the ETT has been known to get caught on the glottic structures. The problem may be alleviated somewhat by using a tapered dilator inside the ETT or by using an epidural catheter as the wire to assist with passing the ETT through the glottis. Bleeding may occur at the site of the tracheal puncture in quantities sufficient to cause a tracheal clot or airway obstruction. Cases of severe hemoptysis with resultant hypoxia, cardiopulmonary arrest, arrhythmias, and death after retrograde wire intubation have been reported.239–242 Subcutaneous emphysema localized to the area of the transtracheal needle puncture is common but usually self-limited. In severe cases, the air may track back through the fascial planes of the neck, leading to tracheal compression with resultant airway compromise, pneumomediastinum, and pneumothorax.243,244 Laryngospasm may result from irritation by the retrograde wire unless the vocal cords are anesthetized or relaxed. Other, less common complications include esophageal perforations, tracheal hematoma, laryngeal edema, infections, tracheitis, tracheal fistulas, trigeminal nerve injury, and vocal cord damage.245,246 The complications reported with retrograde wire intubation were most often associated with multiple attempts, large-gauge needles, and untrained staff members in emergency settings.247
2 Cricothyrotomy
Two methods are described: the surgical cricothyrotomy (using a scalpel) and the needle cricothyrotomy (using a needle set). In both procedures, the cricothyroid membrane must be perforated. Acute complications include bleeding (especially during surgical cricothyrotomy), misplacement of the tube (especially after needle cricothyrotomy), failure of airway access, wound infection, displaced cartilage fractures, and laryngotracheal separation.248 Other complications include breaking and bending of the needle, subcutaneous emphysema, pneumothorax, pneumomediastinum, and pneumopericardium. When cricothyrotomy is performed in the case of total upper airway obstruction, barotrauma may occur because of expiratory blockade.
B Transtracheal Airway
1 Transtracheal Jet Ventilation
To accomplish TTJV, a long, large-bore catheter is advanced through the cricothyroid membrane into the trachea. If this catheter is displaced from the trachea, subcutaneous emphysema, hypoventilation, pneumomediastinum, pneumothorax, severe abdominal distention, or death may result.164 On the basis of normal skin compliance, a 4-inch catheter may be pulled into the subcutaneous space by applying traction to its proximal end. The hub of the TTJV catheter must be continuously pressed firmly against the skin.
Barotrauma is a potential complication of TTJV.249,250 Oxygen delivered through a transtracheal catheter must be able to escape the lungs freely, or overdistention and pulmonary rupture may occur.251,252 Any changes in breath sounds, chest wall expansion, or hemodynamics should be considered to result from pneumothorax. In cases of total airway obstruction, the risk for pneumothorax is greatly increased because gas cannot escape from the lungs in a normal manner. Strong consideration should be given to placing a second transtracheal egress catheter in these circumstances. Laryngospasm can impede the outward flow of oxygen from the trachea. It should be prevented by providing adequate local anesthesia to the neighboring structures or by relaxing the patient.250 If the larynx is obstructed by a foreign body, only low-flow oxygen should be delivered until safe egress of gas is established. Inadvertent placement of a gas delivery line into the gastrointestinal tract may result in complications and may cause gastric rupture, esophageal perforation, bleeding, hematoma, and hemoptysis.253,254
Damage to the tracheal mucosa may occur in patients who are managed with long-term TTJV, especially if the gas is not humidified.255 The possibility of tracheal mucosal ulceration should be considered in any patient if nonhumidified TTJV is attempted through single-orifice catheters for a prolonged period.
2 Percutaneous Dilatational Tracheostomy
Percutaneous dilatational tracheostomy is not primarily recommended for emergency use. With further development, these insertion techniques became faster and appeared to be suitable for emergency situations in skilled hands.256–260 Different sets are available.
Bleeding, subcutaneous and mediastinal emphysema, pneumothorax, airway obstruction, aspiration, infection, and death are early complications. Accidental extubation is a serious complication, because replacement of the cannula may be impossible. In this situation, orotracheal intubation or a translaryngeal oxygenation is required.261 Bacteremia also has been reported.262
3 Formal Tracheostomy
Bleeding is a complication of all surgical procedures, including airway access procedures. Minitracheostomy occasionally results in excessive bleeding into the airway, necessitating progression to full surgical tracheostomy.263 The inflated cuff used in formal tracheostomy prevents pulmonary aspiration of blood. In rare cases, the innominate artery can rupture into the trachea because of excessive pressure from the tracheostomy tube, with resultant massive hemorrhage into the airway. Air embolism during operative procedure is possible.
V Physiologic Responses
A Hemodynamic Changes
Direct laryngoscopy and tracheal intubation are potent stimuli that may instigate an intense autonomic response.264,265 Tachycardia, hypertension, arrhythmias, bronchospasm, and bronchorrhea are common; hypotension and bradycardia occur less often. Patients with preexisting hypertension are even more at risk when they are under stress.
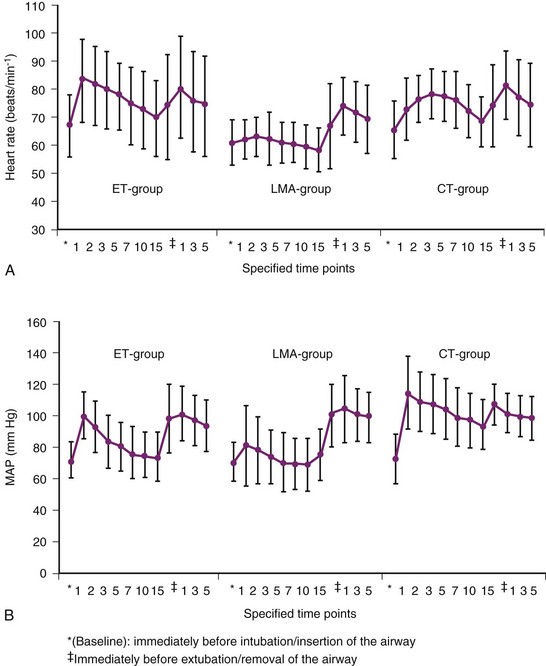
Oczenski and colleagues showed that the insertion of a Combitube was associated with a significantly higher and longer-lasting increase in systolic, diastolic, and mean arterial pressure; heart rate; and plasma catecholamine concentration compared with insertion of a LMA and laryngoscopic endotracheal intubation (Fig. 51-4).266 Hemodynamic and catecholamine responses to insertion of an LMA are minimal.267,268 The apparently sympathetically mediated responses to mechanical stimulation of larynx, trachea-carina, and bronchi may be completely or partially blocked by topical or intravenous lidocaine.269 The magnitude of stimuli to the upper airway depends on the number of attempts and the duration of intubation. In cases of difficult airway situations a higher increase of hemodynamic responses is anticipated. The hemodynamic response may also be blunted by giving opioids or short-acting selective β1-blockers before laryngoscopy and intubation.270 Because many patients have coexisting cardiovascular disease and cannot meet increased myocardial oxygen demands, large hemodynamic responses must be prevented. More than 11% of patients with myocardial disease develop some degree of myocardial ischemia during intubation.271 The key is to provide an adequate depth of anesthesia with intravenous or inhalational agents before instrumentation of the airway.
Fiberoptic intubation performed under sufficient local anesthesia and conscious sedation is an appropriate technique to prevent major hemodynamic changes during intubation. Minor hemodynamic changes and minor increases of plasma catecholamine concentration are nevertheless apparent in this technique. Fiberoptic intubation using a special mask adapter shows fewer hemodynamic changes than those caused by laryngoscopy after induction of anesthesia. The lowest cardiovascular responses were documented in patients after insertion of an LMA.272
B Laryngospasm
Laryngospasm is a protective reflex mediated by the vagus nerve. This reflex is an attempt to prevent aspiration of foreign bodies into the trachea. It may be provoked by movement of the cervical spine, pain, vocal cord irritation by secretions, or sudden stimulation while the patient is still in a light plane of anesthesia.273
In some cases of laryngospasm, the patient makes respiratory efforts but cannot move air in or out of the lungs. If direct laryngoscopy was performed, the vocal cords would be completely adducted. However, laryngospasm involves more than spastic closure of the vocal cords. An infolding of the arytenoids and the aryepiglottic folds occurs; these structures are subsequently covered by the epiglottis.274 Malpositioning, incorrect insertion of an LMA, secretions or blood in the airway, and inadequate depth of anesthesia during intubation or extubation of the LMA or tracheal tube may induce laryngospasm. It may also occur during fiberoptic intubation performed in unanesthetized or subanesthetized laryngeal structures. A firm jaw thrust can sometimes break the spasm—the hyoid is elevated, thereby stretching the epiglottis and aryepiglottic folds to open the forced closure.
The stimulus should be removed, a change of airway should be considered, and secretions should be suctioned away. Positive mask pressure with 100% oxygen may help by distending the pharynx or vocal cords, but this technique is not always adequate. Gentle chest compression in children may also help.275 Deepening the anesthesia with small doses of propofol (0.25 to 0.8 mg/kg given intravenously can treat laryngospasm in 76.9%) or treatment with a short-acting muscle relaxant (0.1 to 3 mg/kg of succinylcholine) are the most promising ways to break the spasm.276
C Bronchospasm
Tracheal irritation from the ETT can cause bronchospasm that is sufficiently severe to prevent air movement throughout the lungs.277 Approximately 80% of the measurable resistance to airflow occurs in the large central airways; the remaining 20% occurs in the smaller peripheral bronchioles.278 The incidence of intraoperative bronchospasm is almost 9% with endotracheal intubation, 0,13% with an LMA, but almost 0% with mask ventilation.279,280 Poor correlation is seen with age, sex, duration or severity of reactive airway disease, duration of anesthesia, or the forced expiratory volume in 1 second.279 Other factors that may contribute to bronchospasm include inhaled stimulants, release of allergic mediators, viral infections, exercise, or pharmacologic factors (including beta-blockers, prostaglandin inhibitors, and anticholinesterases). Bronchospasm may occur during fiberoptic intubation if parts of subglottic airway are insufficiently anesthetized. The spasm can be treated with inhalation of epinephrine or isoproterenol or a β2-agonist (e.g., albuterol, metaproterenol, or terbutaline) or by deepening the level of a volatile anesthetic.
D Coughing and Bucking
Two additional adverse responses to intubation are coughing and bucking on the ETT.281 These responses are potentially hazardous in cases of increased intracranial pressure,282 intracranial vascular anomalies, open-globe injuries, or ophthalmologic surgery or in cases in which increased intra-abdominal pressure may rupture an abdominal incision.283 Intubating a patient only when an adequate depth of anesthesia has been achieved helps to prevent this reflex.
E Vomiting, Regurgitation, and Aspiration
The overall incidence of aspiration during general anesthesia has been reported as 1 in 2131 procedures (in Sweden) to 1 in 14,150 procedures (in France). The incidence in the United States was 1 in 3216 procedures. The associated mortality rate was 1 in 71,829 cases in the United States.284 A meta-analysis of 547 publications concerning use of the LMA suggested that the overall incidence of pulmonary aspiration was about 2 in 10,000 cases.285
In any patient considered to have a full stomach, the likelihood of vomiting in response to irritation of the airway is increased, and aspiration of stomach contents is a constant concern. Aspiration leads to coughing, laryngospasm, and bronchospasm, assuming that protective reflexes are intact. Hypertonia, bradycardia, asystole, and hypoxia may occur. The magnitude of pulmonary reactions depends on the type and quantity of the aspirated material.286
It is possible to completely obstruct the airway with CP. CP has resulted in airway obstruction in patients with lingual tonsils, lingual thyroid glands,287 and undiagnosed laryngeal trauma.288 If any doubt exists about the success of an oral intubation, awake techniques should be considered under these circumstances.289
F Intraocular Pressure Changes
Intraocular pressure increases during direct laryngoscopy and extubation, but not during LMA insertion.290,291 Decreased intraocular pressure was observed under tracheal intubation during general anesthesia with propofol and with sevoflurane, both combined with remifentanil.292
Sufentanil is effective in preventing intraocular pressure increases caused by rapid-sequence induction with succinylcholine; alternatively rocuronium can be used.293 Increased intraocular pressure should be strictly avoided in patients with penetrating eye injuries.
G Intracranial Pressure Changes
Intracranial pressure markedly and transiently rises during laryngoscopy and endotracheal intubation. Patients with head injury are at risk from this increase because it reduces cerebral perfusion and may increase the likelihood of secondary brain damage.294 Fiberoptic bronchoscopy produces a substantial but transient increase of intracranial pressure.295 Deep anesthesia during induction can prevent these adverse effects.
H Apnea
Apnea may be a reflex response to tracheal irritation from the ETT or other airway techniques. Extraneous reasons for the apnea—for example, if the patient is a premature or term neonate,296 has had induction drugs or excessive narcotics, or has a reflux response to light levels of anesthesia—should be ruled out initially. If no clear reason exists for the patient’s lack of respiratory effort, mechanical ventilation can be initiated, and spontaneous ventilation can be attempted later.
I Latex Allergy
Of anaphylaxis episodes occurring during surgical procedures, 16.6% are related to latex allergies.297 To prevent anaphylaxis during anesthesia and surgery, the patient’s history should be evaluated preoperatively. There is no therapy for latex allergy, and avoidance of latex-containing products is mandatory for predisposed individuals.298 Latex allergy affects 8% of the U.S. general population and has a prevalence of 30% among health care workers.299,300 There has been an increase in the incidence of type I and IV latex sensitivity in the general population, from 1% in 1980 to 8% in 1996.301 The prevalence of latex sensitivity among anesthesiologists is about 12.5%, and the prevalence of allergy is 2.4%.302
Patients with spina bifida, rubber industry workers, atopic patients, and patients with a history of many operations are most at risk.303 Patients with certain exotic food allergies may also have a coexisting latex allergy304; in one study, the rate was 86%.305
VI Complications with Extubation
Primary and secondary responses to extubation are possible. The primary effects are local and systemic responses (Box 51-2). The same responses after intubation may be observed at extubation. During intubation, the patient is more protected by anesthesia induction than during extubation, and the cardiovascular responses may be even more exaggerated. The most serious complication after extubation is acute airway obstruction. Decreased consciousness with central respiratory depression, decreased muscle tone, and tongue retraction to the postpharyngeal wall may lead to inspiratory or expiratory stridor, dyspnea, cyanosis, tachycardia, hypertension, agitation, and sweating. Laryngospasm is also possible, and urgent treatment is necessary to prevent hypoxia, brain damage, and death. Other complications after extubation are not caused by the removal of the tube itself; they are consequences of the previous intubation and the duration of tube placement, such as laryngitis, edema, ulcerations, granuloma, or synechia of the vocal cords. The quality of tracheal intubation contributes to laryngeal morbidity, and excellent conditions are less frequently associated with postoperative hoarseness and vocal cord sequelae.
Box 51-2
Pathophysiologic Effects of Tracheal Extubation
Modified from Hartley M: Difficulties in tracheal extubation. In Latto IP, Vaughan RS, editors: Difficulties in tracheal intubation, London, 1997, Saunders.
A Hemodynamic Changes
Hemodynamic changes, including a 20% increase in heart rate and blood pressure, occur in most patients at the time of extubation,306,307 and symptoms that are associated with sympathoadrenal activity should be expected. These changes are usually transient and rarely require treatment. Although most patients tolerate these hemodynamic responses well, patients with cardiac disease,271 pregnancy-induced hypertension,308 and increased intracranial pressure may be at particular risk for life-threatening ischemic myocardial episodes.309 Patients with cardiac disease have had decreased ejection fractions at the time of extubation.310 Management consists of extubation under deep anesthesia or pharmacologic therapy. Deep extubation is inappropriate for patients with a difficult airway, those at high risk for aspiration, and those with compromised airway access. Pharmacologic strategies emphasize the importance of decreasing the heart rate, such as with short-acting beta-blockers.311 Cerebral hemorrhage is possible. Using an LMA may significantly reduce local and cardiovascular responses at removal if the cuff pressure is minimized to avoid overstimulation of the patient.26
B Laryngospasm
In a computer-aided study of 136,929 patients, the incidence of laryngospasm was 50 cases per 1000 children with bronchial asthma or airway infection and 25 cases per 1000 in children 1 to 3 months old after tracheal intubation had been performed.312
The optimal course for treating laryngospasm is to avoid it in the first place. Treatment was described earlier. When laryngospasm is anticipated, the patient may undergo a deep extubation. A patient undergoing deep extubation should be placed in the lateral position with the head down to keep the vocal cords clear of secretions during emergence. It is best to extubate patients during a positive-pressure breath to remove residual secretions. Extubation during positive-pressure breath is the procedure of choice in children. A study showed that children could be safely extubated in deep anesthesia from a 1.5 minimum effective alveolar anesthetic concentration of sevoflurane or desflurane.313 The study of Koga and colleagues showed that the rate of airway obstruction in patients extubated during deep anesthesia (17 of 20) was not higher than in patients extubated after regained consciousness (18 of 20).314
C Laryngeal Edema
Laryngeal edema is an important cause of post-extubation obstruction, especially in neonates and infants. This condition has various causes and is classified as supraglottic, retroarytenoidal, or subglottic.315 Supraglottic edema most commonly results from surgical manipulation, positioning, hematoma formation, overaggressive fluid management, impaired venous drainage, or coexisting conditions (e.g., preeclampsia, angioneurotic edema). Retroarytenoidal edema typically results from local trauma or irritation. Subglottic edema occurs most often in children, particularly neonates and infants. Factors associated with development of subglottic edema include traumatic intubation, intubation lasting longer than 1 hour, bucking on the ETT, changes in head position, or tight-fitting tubes. Laryngeal edema usually manifests as stridor within 30 to 60 minutes after extubation, although it may start as late as 6 hours after extubation. Regardless of the cause of laryngeal edema, management depends on the severity of the condition. Therapy consists of humidified oxygen, nebulized epinephrine, head-up positioning, and occasionally reintubation with a smaller ETT. The practice of administering parenteral steroids with the goal of preventing or reducing edema after long-term (>36 hours) ventilation may prove beneficial for adult patients, but routine administration for anesthesia is controversial.316
D Laryngotracheal Trauma
Unlike trauma during intubation, airway trauma at the time of extubation is not well described. Arytenoid cartilage dislocation has been reported after difficult and routine intubations.122,317 Symptoms become apparent soon after extubation and may be mild (e.g., difficulty swallowing, voice changes) or major (e.g., complete airway obstruction). Management depends on the severity of the condition. Options include reintubation, arytenoid reduction, and tracheostomy. If laryngotracheal trauma is suspected, an otolaryngology consultation is warranted.
F Negative-Pressure Pulmonary Edema
When airway obstruction occurs after extubation in the case of laryngospasm, negative-pressure pulmonary edema may occur in a spontaneously breathing patient. As a result of inspiratory effort against the closed glottis, these patients generate negative intrapleural pressure of more than 100 cm H2O. Rib retraction with poor air movement, laryngospasm, and stridor may lead to the rare diagnosis. Increased left ventricular preload and afterload, altered pulmonary vascular resistance, increased adrenergic state, right ventricle dilation, intraventricular septum shift to the left, left ventricular diastolic dysfunction, increased left heart loading conditions, enhanced microvascular intramural hydrostatic pressure, negative pleural pressure, and transmission to the lung interstitium may result in a marked increase in transmural pressure, fluid filtration into the lung, and development of pulmonary edema.318
G Aspiration
Pulmonary aspiration of gastric contents is a constant threat for any patient who has a full stomach or is at risk for postoperative vomiting. Laryngeal function is altered for at least 4 hours after tracheal extubation.319 Coughing is a physiologic response to protect the airway from aspiration. Depression of reflexes, along with the presence of residual anesthetic agents, places most recently extubated patients at risk. Aspiration is probably more prevalent than is currently thought. Most cases are so minor that they do not affect the patient’s postoperative course. Reducing gastric contents by suctioning through a gastric tube and extubation with the patient placed in the lateral position with a head-down tilt is the safest protection against aspiration. Perioperative problems, if they do occur, are usually attributed to factors such as atelectasis. Management consists of supportive measures. Depending on the extent of aspiration, measures include supportive care, ranging from administration of oxygen through a nasal cannula to reintubation with mechanical ventilation, and PEEP.
H Airway Compression
External compression of the airway after extubation may lead to obstruction. An excessively tight postoperative neck dressing is a cause of external compression that is easily resolved. A more ominous situation is a rapidly expanding hematoma close to the airway. This may occur after certain operations, such as carotid endarterectomy, and must be quickly diagnosed and treated before total airway obstruction occurs.320 Immediate surgical re-exploration is indicated, although the airway concerns for these patients should be approached with extreme caution. To minimize airway distortion, general anesthesia should be avoided until the wound is evacuated under local anesthesia. However, even after surgical drainage, airway obstruction may occur as the result of venous or lymphatic congestion. Any use of muscle relaxants during anesthesia induction in these patients may result in catastrophe, regardless of whether the wound was previously drained. Conservative options for managing the airway in this situation include awake fiberoptic intubation, surgical airways, or inhalation induction. Muscle relaxants should be avoided until the airway is secured.
External compression of the neck, such as chronic compression of a goiter, may also result from tracheomalacia.321 This condition is usually seen after the goiter has been removed, although cases were reported in which the airway collapsed with induction or after extubation.322,323 Airway obstruction in these patients becomes apparent soon after extubation. Management includes reintubation, surgical tracheal support (i.e., stenting), or tracheostomy below the level of obstruction.
I Difficult Extubation
Occasionally, ETTs are difficult to remove. Possible causes are failure to deflate the cuff, use of an oversized tube,324 adhesion of the tube to the tracheal wall,325 or transfixation of the tube by an inadvertent suture to a nearby organ, a wire, a screw placed in an oromaxillofacial operation, or a broken drill.326–329340 Possible sequelae of these complications include airway leak, aspiration, tube obstruction, and trauma from attempts at forceful extubation. One case was reported in which a nasogastric tube made a loop around the ETT.330 In most cases, the problem arises from an inability to deflate the cuff, commonly as a result of failure in the cuff-deflating mechanism. If this problem occurs, the cuff should be punctured with a transtracheal needle. If tube fixation is suspected, the passage of the tube should be checked with a suction catheter or a fiberscope. Forceful removal of an ETT with the cuff inflated may result in damage to the vocal cords and arytenoid dislocation.
J Accidental Extubation
Accidental extubation during anesthesia has been reported with disposable tonsillectomy instruments,331 change of the patient’s head position, and in neurosurgery with the patient in the knee-elbow position.332 Most accidental extubations were reported from intensive care unit patients, for whom self-extubation was the most common incident (77% to 85%).333–335 The rate of reintubation was 37% to 57%.333–335 The requirement for reintubation is higher for patients with full ventilatory support than those during the weaning phase.
Patients at risk for accidental extubation are characterized by the absence of physical restraints, a high nurse-to-patient ratio, trips out of the intensive care unit (59%), light sedation (43%), use of bedside portable radiography, accidental removal of the nasogastric tube or tugging on the ETT, oral intubation, and insufficient sedation.336 Complications after accidental extubation may be hypoxia, hypercarbic respiratory failure, aspiration, retention of pulmonary secretion, arrhythmia, and tachycardia. To avoid unplanned extubation, tubes can be secured with special tube holders,337 with waterproof tape, and with fixation using a knot or a bow.338,339
Reintubation may be very difficult, especially after a difficult intubation. The use of a Combitube or an LMA is required in some cases of inadequate access to the patient’s head in the intensive care setting.340
VIII Clinical Pearls
• The final goal of airway management is oxygenation of the patient, not placement of an endotracheal tube (ETT).
• Serious complications of airway management result from not recognizing the level of airway difficulties.
• To minimize injury to the patient, the anesthesiologist should examine the patient’s airway carefully, identify potential problems, devise a plan that involves the least risk for injury, and have a backup plan immediately available. Common sense should prevail at all times.
• In daily anesthesia practice, errors of omission are more common than errors of commission. Errors of omission include failure to recognize the magnitude of a problem, failure to make appropriate observations, and failure to act in a timely manner. Errors of commission include actions such as trauma to the lips, nose, or laryngotracheal mucosa; forcing sharp instruments into areas in which they do not belong; or introducing air or secretions into regions of the body in which further complications will ensue.
• Many complications in airway management result from insufficient communication between the members of the medical team and improper coordination of the patients in the daily operating room schedule. A patient with known difficult airway problems should be scheduled at a time when the most experienced anesthesiologists and surgeons are available.
• Delayed recognition of complications leads to delayed therapy. Inadequate monitoring, nonfunctional equipment, and an untrained staff can contribute to airway catastrophes.
• The overall risk of aspiration and regurgitation using the laryngeal mask airway (LMA) is about that for endotracheal intubation when the indications and contraindications for the LMA are respected. The risk of aspiration, which is a consequence of the airway device’s design, should be weighed against the advantages of the LMA in cases of difficult intubation and ventilation.
• Because of the increased risk associated with multiple attempts of any airway technique, a maximum of three attempts is recommended to minimize trauma to the airway.
• Any airway device technique may cause movement and subsequent injury to the patient with an injured cervical spine.
• A patent airway is an absolute requirement for safe anesthesia. Airway obstruction can occur at any time during administration of general anesthesia, particularly in prolonged operations or in patients with predisposing anatomic abnormalities. The most serious complication after extubation is the occurrence of acute airway obstruction.
All references can be found online at expertconsult.com.
14 El-Orbany M, Woehlck HJ. Difficult mask ventilation. Anesth Analg. 2009;109:1870.
27 Seet E, Yousaf F, Gupta S, et al. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: A prospective, randomized trial. Anesthesiology. 2010;112:652.
34 Brimacombe J, Clarke G, Keller C. Lingual nerve injury associated with the ProSeal laryngeal mask airway: A case report and review of the literature. Br J Anaesth. 2005;95:420.
46 Benumof JL. Laryngeal mask airway and the ASA difficult airway algorithm. Anesthesiology. 1996;84:686.
54 López AM, Valero R, Brimacombe J. Insertion and use of the LMA Supreme in the prone position. Anaesthesia. 2010;65:154.
74 Benumof JL, Cooper SD. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J Clin Anesth. 1996;8:136.
76 Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia. 2008;63:745.
171 Ghafoor AU, Martin TW, Gopalakrishnan S, Viswamitra S. Caring for the patients with cervical spine injuries: What have we learned? J Clin Anesth. 2005;17:640.
183 Martin DP, Weingarten TN, Gunn PW, et al. Performance improvement system and postoperative corneal injuries: Incidence and risk factors. Anesthesiology. 2009;111:320.
275 Al-Metwalli RR, Mowafi HA, Ismail SA. Gentle chest compression relieves extubation laryngospasm in children. J Anesth. 2010;24:854.
276 Al-alami AA, Zestos MM, Baraka AS. Pediatric laryngospasm: Prevention and treatment. Curr Opin Anaesthesiol. 2009;22:388.
289 El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg. 2010;110:1318.
335 Tanios MA, Epstein SK, Livelo J, Teres D. Can we identify patients at high risk for unplanned extubation? A large-scale multidisciplinary survey. Respir Care. 2010;55:561.
1 Domino KB, Posner KL, Caplan RA, et al. Airway injury during anesthesia: A closed claims analysis. Anesthesiology. 1999;91:1703.
2 Cook TM, Scott S, Mihai R. Litigation related to airway and respiratory complications of anaesthesia: An analysis of claims against the NHS in England 1995-2007. Anaesthesia. 2010;65:556.
3 Confidential enquiries into maternal and child health: Why mothers die 2000-2002. The Sixth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. London: RCOG Press, 2004.
4 Aders A, Aders H. Anaesthetic adverse incident reports: An Australian study of 1,231 outcomes. Anaesth Intensive Care. 2005;33:336.
5 Auroy Y, Benhamou D, Péquignot F, et al. Mortality related to anaesthesia in France: Analysis of deaths related to airway complications. Anaesthesia. 2009;64:366.
6 Khan ZH, Mohammadi M, Rasouli MR, et al. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: A prospective study. Anesth Analg. 2009;109:822.
7 L’Hermite J, Nouvellon E, Cuvillon P, et al. The Simplified Predictive Intubation Difficulty Score: A new weighted score for difficult airway assessment. Eur J Anaesthesiol. 2009;26:1003.
8 Adnet F. Difficult mask ventilation. Anesthesiology. 2000;92:1217.
9 Durkan W, Fleming N. Potential eye damage from reusable masks [letter]. Anesthesiology. 1987;67:444.
10 Murray WJ, Ruddy MP. Toxic eye injury during induction of anesthesia. South Med J. 1985;78:1012.
11 Smurthwaite GJ, Ford P. Skin necrosis following continuous positive airway pressure with a face mask. Anaesthesia. 1993;48:147.
12 Azar I, Lear E. Lower lip numbness following general anesthesia [letter]. Anesthesiology. 1986;65:450.
13 Glauber DT. Facial paralysis after general anesthesia. Anesthesiology. 1986;65:516.
14 El-Orbany M, Woehlck HJ. Difficult mask ventilation. Anesth Analg. 2009;109:1870.
15 Fredrickson KL, D’Angelo AJ, Jr. Internal laryngopyocele presenting as acute airway obstruction. Ear Nose Throat J. 2007;86:104.
16 Töro K, Kardos M, Dunay G. Fatal asphyxia due to laryngomucocele. Forensic Sci Int. 2009;190:e1. 10
17 Jarjour NN, Wilson P. Pneumocephalus associated with nasal continuous positive airway pressure in a patient with sleep apnea syndrome. Chest. 1989;96:1425.
18 Klopfenstein CE, Forster A, Suter PM. Pneumocephalus: A complication of continuous positive airway pressure after trauma. Chest. 1980;78:656.
19 Weaver LK, Fairfax WR, Greenway L. Bilateral otorrhagia associated with continuous positive airway pressure. Chest. 1988;93:878.
20 Weiss M, Gerber AC. [Induction of anaesthesia and intubation in children with a full stomach: Time to rethink!]. Anaesthesist. 2007;56:1210.
21 Wilkins CJ, Cramp PG, Staples J, et al. Comparison of the anesthetic requirement for tolerance of laryngeal mask airway and endotracheal tube. Anesth Analg. 1992;75:794.
22 Pennant JH, White PF. The laryngeal mask airway: Its use in anesthesiology. Anesthesiology. 1993;79:144.
23 American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269.
24 Brain AIJ. The Intravent laryngeal mask instruction manual, ed 2. Berkshire, UK: Brain Medical; 1992.
25 Krier C, Georgi R. Airway management. Stuttgart: Thieme; 2001.
26 Brimacombe JR, Brain AIJ. The laryngeal mask airway. Philadelphia: Saunders; 1997.
27 Seet E, Yousaf F, Gupta S, et al. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: A prospective, randomized trial. Anesthesiology. 2010;112:652.
28 Verghese C, Smith TG, Young E. Prospective survey of the use of the laryngeal mask in 2359 patients. Anaesthesia. 1993;48:58.
29 Brimacombe J, Holyoake L, Kellar C, et al. Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology. 2000;93:26.
30 Marjot R. Pressure exerted by the laryngeal mask airway cuff upon the pharyngeal mucosa. Br J Anaesth. 1993;70:25.
31 Miller AC, Bickler P. The laryngeal mask airway: An unusual complication. Anaesthesia. 1991;46:659.
32 Lee JJ. Laryngeal mask and trauma to uvula [letter]. Anaesthesia. 1989;44:1014.
33 Marjot R. Trauma to the posterior pharyngeal wall caused by a laryngeal mask airway [letter]. Anaesthesia. 1991;46:589.
34 Brimacombe J, Clarke G, Keller C. Lingual nerve injury associated with the ProSeal laryngeal mask airway: A case report and review of the literature. Br J Anaesth. 2005;95:420.
35 Ezri T, Priscu V, Szmuk P. Laryngeal mask and pulmonary edema [letter]. Anesthesiology. 1993;78:219.
36 Wynn JM, Jones KL. Tongue cyanosis after laryngeal mask airway insertion. Anesthesiology. 1994;80:1403.
37 Lloyd JFR, Hegab A. Recurrent laryngeal nerve palsy after laryngeal mask airway insertion. Anaesthesia. 1996;51:171.
38 Conacher ID. Foreign body in a laryngeal mask airway [letter]. Anaesthesia. 1991;46:164.
39 Brain AIJ, Verghese C, Strube PJ. The LMA “ProSeal”: A laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650.
40 Brimacombe J, Keller C. The ProSeal laryngeal mask airway. Anesthesiology. 2000;93:104.
41 Keller C, Brimacombe J, Kleinsasser A, et al. Does the ProSeal laryngeal mask airway prevent aspiration of regurgitated fluid? Anesth Analg. 2000;91:1017.
42 Brimacombe J, Keller C, Berry A. Gastric insufflation with the ProSeal laryngeal mask. Anesth Analg. 2001;92:1614.
43 Stix MS, Borromeo CJ, O’Connor CJ, Jr. Esophageal insufflation with normal fiberoptic positioning of the ProSeal laryngeal mask airway. Anesth Analg. 2002;94:1036.
44 Ferson DZ, Rosenblatt WH, Johansen MJ, et al. Use of the intubating LMA-Fastrach in 254 patients with difficult-to-manage airways. Anesthesiology. 2001;95:1175.
45 Joo HS, Kapoor S, Rose DK, et al. The intubating laryngeal mask after induction of general anesthesia versus awake fiberoptic intubation in patients with difficult airway. Anesth Analg. 2001;92:1342.
46 Benumof JL. Laryngeal mask airway and the ASA difficult airway algorithm. Anesthesiology. 1996;84:686.
47 Lu PP, Yang CH, Ho AC, et al. The intubating LMA: A comparison of insertion techniques with conventional tracheal tubes. Can J Anaesth. 2000;478:837.
48 Branthwaite MA. An unexpected complication of the intubating laryngeal mask. Anaesthesia. 1999;54:166.
49 Eschertzhuber S, Brimacombe J, Hohlrieder M, et al. The laryngeal mask airway Supreme—A single use laryngeal mask airway with an oesophageal vent: A randomised, cross-over study with the laryngeal mask airway ProSeal in paralysed, anaesthetised patients. Anaesthesia. 2009;64:79.
50 Shin WJ, Cheong YS, Yang HS, Nishiyama T. The supraglottic airway I-gel in comparison with ProSeal laryngeal mask airway and classic laryngeal mask airway in anaesthetized patients. Eur J Anaesthesiol. 2010;27:598.
51 Timmermann A, Cremer S, Eich C, et al. Prospective clinical and fiberoptic evaluation of the Supreme laryngeal mask airway. Anesthesiology. 2009;110:262.
52 Braude D, Southard A, Bajema T, et al. Rapid sequence airway using the LMA-Supreme as a primary airway for 9 h in a multi-system trauma patient. Resuscitation. 2010;81:1217.
53 Teoh WH, Lee KM, Suhitharan T, et al. Comparison of the LMA Supreme vs the i-gel in paralysed patients undergoing gynaecological laparoscopic surgery with controlled ventilation. Anaesthesia. 2010;65:1173.
54 López AM, Valero R, Brimacombe J. Insertion and use of the LMA Supreme in the prone position. Anaesthesia. 2010;65:154.
55 Frass M, Frenzer R, Zdrahal F. The esophageal tracheal Combitube: Preliminary results with a new airway for CPR. Ann Emerg Med. 1987;16:768.
56 Frass M. The Combitube: Esophageal/tracheal double-lumen airway. In: Benumof JL, ed. Airway management: Principles and practice. St Louis: Mosby; 1996:444.
57 Urtubia RM, Aguila CM, Cumsille MA. Combitube: A study for proper use. Anesth Analg. 2000;90:958.
58 Hartmann T, Hoerauf KH, Benumof JL, et al. The esophageal-tracheal Combitube small adult: An alternative airway for ventilatory support during gynaecological laparoscopy. Anaesthesia. 2000;55:670.
59 Gaitini LA, Vaida SJ, Mostafa S, et al. The Combitube in elective surgery. Anesthesiology. 2001;94:79.
60 Hoerauf KH, Hartmann T, Acimovic S. Waste gas exposure to sevoflurane and nitrous oxid during anaesthesia using the oesophageal-tracheal Combitube small adult. Br J Anaesth. 2001;86:124.
61 Lipp MDW, Jaehnichen G, Golecki N, et al. Microbiological, microstructure and material science examinations of reprocessed Combitubes after multiple reuse. Anesth Analg. 2000;91:693.
62 Miller DM, Youkhana I, Karunaratne WU, et al. Presence of proteine deposits on “cleaned” re-usable anesthetic equipment. Anaesthesia. 2001;56:1069.
63 Green KS, Beger TH. Proper use of the Combitube [letter]. Anesthesiology. 1994;81:513.
64 Zamora JE, Saha TK. Combitube rescue for Cesarean delivery followed by ninth and twelfth cranial nerve dysfunction. Can J Anaesth. 2008;55:779.
65 Bagheri SC, Stockmaster N, Delgado G, et al. Esophageal rupture with the use of the Combitube: Report of a case and review of the literature. J Oral Maxillofac Surg. 2008;66:1041.
66 Vézina MC, Trépanier CA, Nicole PC, Lessard MR. Complications associated with the Esophageal-Tracheal Combitube in the pre-hospital setting. Can J Anaesth. 2007;54:124.
67 Greenberg RS, Toung T. The cuffed oro-pharyngeal airway: A pilot study. Anesthesiology. 1992;77:558.
68 Dörges V, Ocker H, Wenzel V, et al. The laryngeal tube: A new simple airway device. Anesth Analg. 2000;90:1220.
69 Benumof JL. The glottic aperture seal airway: A new ventilatory device. Anesthesiology. 1998;88:1219.
70 Turan A, Kaya G, Koyuncu O, et al. Comparison of the laryngeal mask (LMA) and laryngeal tube (LT) with the new perilaryngeal airway (CobraPLA) in short surgical procedures. Eur J Anaesthesiol. 2006;23:234.
71 Hagberg C, Bogomolny Y, Gilmore C, et al. An evaluation of the insertion and function of a new supraglottic airway device, the King LT, during spontaneous ventilation. Anesth Analg. 2006;102:621.
72 Rose DK, Cohen MM. The airway: Problems and predictions in 18,500 patients. Can J Anaesth. 1994;41(Pt 1):372.
73 Takahata O, Kubota M, Mamiya K, et al. The efficacy of the “BURP” maneuver during a difficult laryngoscopy. Anesth Analg. 1997;84:419.
74 Benumof JL, Cooper SD. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J Clin Anesth. 1996;8:136.
75 Aziz MF, Healy D, Kheterpal S, et al. Routine clinical practice effectiveness of the Glidescope in difficult airway management: An analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34.
76 Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia. 2008;63:745.
77 Leong WL, Lim Y, Sia AT. Palatopharyngeal wall perforation during Glidescope intubation. Anaesth Intensive Care. 2008;36:870.
78 Latto IP, Vaughan RS. Difficulties in tracheal intubation. London: Saunders; 1997.
79 Nagaoka E, Takenaka I, Kadoya T. The McCoy laryngoscope expands the laryngeal aperture in patients with difficult intubation. Anesthesiology. 2000;92:1855.
80 Boedeker BH, Barak-Bernhagen MA, Miller DJ, et al. Improving rigid fiberoptic intubation: A comparison of the Bonfils Intubating Fiberscope with a novel modification. BMC Emerg Med. 2010;27:10.
81 Liem EB, Bjoraker DG, Gravenstein D. New options for airway management: Intubating fibreoptic stylets. Br J Anaesth. 2003;91:408.
82 Hemmerling TM, Bracco D. Subcutaneous cervical and facial emphysema with the use of the Bonfils fiberscope and high-flow oxygen insufflation. Anesth Analg. 2008;106:260.
83 White A, Kander PL. Anatomical factors in difficult direct laryngoscopy. Br J Anaesth. 1975;47:468.
84 Cass NM, James NR, Lines V. Intubation under direct laryngoscopy. BMJ. 1956;2:488.
85 Benumof JL. Management of the difficult adult airway: With special emphasis on awake tracheal intubation. Anesthesiology. 1991;75:1087.
86 Nichol HC, Zuck D. Difficult laryngoscopy: The “anterior” larynx and the atlanto-occipital gap. Br J Anaesth. 1983;55:141.
87 Bellhouse CP, Doré C. Criteria for estimating likelihood of difficulty of endotracheal intubation with the Macintosh laryngoscope. Anaesth Intensive Care. 1988;16:329.
88 Horton WA, Fahy L, Charters P. Disposition of cervical vertebrae, atlanto-axial joint, hyoid and mandible during x-ray laryngoscopy. Br J Anaesth. 1989;63:435.
89 Chou HC, Wu TL. Mandibulohyoid distance in difficult laryngoscopy. Br J Anaesth. 1993;71:335.
90 Frerk CM. Predicting difficult intubation. Anaesthesia. 1991;46:1005.
91 Rosenberg H, Rosenberg HK. Airway obstruction and tracheal intubation. In: Gravenstein N, Kirby RR. Complications in anesthesiology. Philadelphia: Lippincott-Raven; 1996:219.
92 Connor CW, Segal S. Accurate classification of difficult intubation by computerized facial analysis. Anesth Analg. 2011;112:84.
93 Horellou MF, Mathe D, Feiss P. A hazard of naso-tracheal intubation [letter]. Anaesthesia. 1978;33:73.
94 Green JG, Wood JM, Davis LF. Asystole after inadvertent intubation of the orbit. J Oral Maxillofac Surg. 1997;55:856.
95 Bähr W, Stoll P. Nasal intubation in the presence of frontobasal fractures: A retrospective study. J Oral Maxillofac Surg. 1992;50:445.
96 O’Connell JE, Stevenson DS, Stokes MA. Pathological changes associated with short-term nasal intubation. Anaesthesia. 1996;51:347.
97 El-Seify ZA, Khattab AM, Shaaban AA, et al. Xylometazoline pretreatment reduces nasotracheal intubation-related epistaxis in paediatric dental surgery. Br J Anaesth. 2010;105:501.
98 Sanuki T, Hirokane M, Matsuda Y, et al. The Parker Flex-Tip tube for nasotracheal intubation: The influence on nasal mucosal trauma. Anaesthesia. 2010;65:8.
99 Binning R. A hazard of blind nasal intubation [letter]. Anaesthesia. 1974;29:366.
100 Cavusoglu T, Yazici I, Demirtas Y, et al. A rare complication of nasotracheal intubation: Accidental middle turbinectomy. J Craniofac Surg. 2009;20:566.
101 Hariri MA, Duncan PW. Infective complications of brief nasotracheal intubation. J Laryngol Otol. 1989;103:1217.
102 Joo DT, Orser BA. External compression of a nasotracheal tube due to the displaced bony fragments of multiple LeFort fractures. Anesthesiology. 2000;92:1830.
103 Elwany S, Mekhamer A. Effect of nasotracheal intubation on nasal mucociliary clearance. Br J Anaesth. 1987;59:755.
104 Dinner M, Tjeuw M, Artusio JF, Jr. Bacteremia as a complication of nasotracheal intubation. Anesth Analg. 1987;66:460.
105 Halac E, Indiveri DR, Obregon RJ. Complication of nasal endotracheal intubation [letter]. J Pediatr. 1983;103:166.
106 Willatts SM, Cochrane DF. Paranasal sinusitis: A complication of nasotracheal intubation. Two case reports. Br J Anaesth. 1985;57:1026.
107 O’Reilly MJ, Reddick EJ, Black W. Sepsis from sinusitis in nasotracheally intubated patients: A diagnostic dilemma. Am J Surg. 1984;147:601.
108 Cataneo AJM, Reibscheid SM, Ruiz RL, Jr., et al. Foreign bodies in the tracheobronchial tree. Clin Pediatr. 1997;36:701.
109 Fitzpatrick PC, Guarisco JL. Pediatric airway foreign bodies. J La State Med Soc. 1998;150:138.
110 Silva AB, Muntz HR, Clary R. Utility of conventional radiography in the diagnosis and management of pediatric airway foreign bodies. Ann Otol Rhinol Laryngol. 1998;107:834.
111 Smith WD, Timms MS, Sutcliffe H. Unusual complication of nasopharyngeal intubation [letter]. Anaesthesia. 1989;44:615.
112 Warner ME, Benefeld SM, Warner MA, et al. Perianesthetic dental injuries. Anesthesiology. 1999;90:1302.
113 Chadwick RG, Lindsay SM. Dental injuries during general anaesthesia. Br Dent J. 1996;180:255.
114 Aromaa U, Pesonen P, Linko K, et al. Difficulties with tooth protectors in endotracheal intubation. Acta Anaesthesiol Scand. 1988;32:304.
115 Brosnan C, Radford P. The effect of a toothguard on the difficulty of intubation. Anaesthesia. 1999;52:1011.
116 Petrovic B, Marković D, Peric T, Blagojevic D. Factors related to treatment and outcomes of avulsed teeth. Dent Traumatol. 2010;26:52.
117 Mayhew JF, Miner M, Katz J. Macroglossia in a 16-month-old child after a craniotomy. Anesthesiology. 1985;62:683.
118 Teeple E, Maroon J, Rueger R. Hemimacroglossia and unilateral ischemic necrosis of the tongue in a long-duration neurosurgical procedure [letter]. Anesthesiology. 1986;64:845.
119 Kharasch ED. Angiotensin-converting enzyme inhibitor–induced angioedema associated with endotracheal intubation. Anesth Analg. 1992;74:602.
120 Patane PS, White SE. Macroglossia causing airway obstruction following cleft palate repair. Anesthesiology. 1989;71:995.
121 Heuhns TY, Yentis SM, Cumberworth V. Apparent massive tongue swelling. Anaesthesia. 1994;49:414.
122 Diaz JH. Is uvular edema a complication of endotracheal intubation? Anesth Analg. 1993;76:1139.
123 Bogetz MS, Tupper BJ, Vigil AC. Too much of a good thing: Uvular trauma caused by overzealous suctioning. Anesth Analg. 1991;72:125.
124 Calikapan GT, Karakus F. Uvula necrosis after endotracheal intubation for rhinoplasty. Aesthetic Plast Surg. 2008;32:710.
125 Rempf C, Pechlivanis I, Zenz M, et al. Swollen and elongated uvula after general anaesthesia [in German]. Anaesthesist. 2008;57:775.
126 Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: A systematic review. J Oral Maxillofac Surg. 2010;68:2359.
127 Brimacombe J, Holyoake L, Keller C, et al. Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology. 2000;93:26.
128 Oczenski W, Krenn H, Dahaba AA, et al. Complications following the use of the Combitube, tracheal tube and laryngeal mask airway. Anaesthesia. 1999;54:1161.
129 Scuderi PE. Postoperative sore throat: More answers than questions. Anesth Analg. 2010;111:831.
130 Kambic V, Radsel Z. Intubation lesions of the larynx. Br J Anaesth. 1978;50:587.
131 Peppard SB, Dickens JH. Laryngeal injury following short-term intubation. Ann Otol Rhinol Laryngol. 1983;92(Pt 1):327.
132 Rieger A. Intubationsschäden: Inzidenz, Komplikationen, Konsequenzen. In: Krier C, Georgi R. Airway management. Stuttgart: Thieme, 2001.
133 Drosnes DL, Zwillenberg DA. Laryngeal granulomatous polyp after short-term intubation of a child. Ann Otol Rhinol Laryngol. 1990;99(Pt 1):183.
134 Alessi DM, Hanson DG, Berci G. Bedside videolaryngoscopic assessment of intubation trauma. Ann Otol Rhinol Laryngol. 1989;98(Pt 1):586.
135 Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation. Anesthesiology. 2003;98:1049.
136 Yamanaka H, Hayashi Y, Watanabe Y, et al. Polonged hoarseness and arytenoid cartilage dislocation after tracheal intubation. Br J Anaesth. 2009;103:452.
137 Aoyanma K, Takenaka I, Nagaoka E, et al. Potential damage to the larynx associated with light-guided intubation: A case and series of fiberoptic examinations. Anesthesiology. 2001;94:165.
138 Usui T, Sato S, Goto F. Arytenoid dislocation while using a McCoy laryngoscope. Anesth Analg. 2001;92:1347.
139 Tan V, Seevanayagam S. Arytenoid subluxation after a difficult intubation treated successfully with voice therapy. Anaesth Intensive Care. 2009;37:843.
140 Bishop MJ, Weymuller EA, Jr., Fink BR. Laryngeal effects of prolonged intubation. Anesth Analg. 1984;63:335.
141 Brandwein M, Abramson AL, Shikowitz MJ. Bilateral vocal cord paralysis following endotracheal intubation. Arch Otolaryngol Head Neck Surg. 1986;112:877.
142 Cavo JW, Jr. True vocal cord paralysis following intubation. Laryngoscope. 1985;95:1352.
143 Lim EK, Chia KS, Ng BK. Recurrent laryngeal nerve palsy following endotracheal intubation. Anaesth Intensive Care. 1987;15:342.
144 Nuutinen J, Karja J. Bilateral vocal cord paralysis following general anesthesia. Laryngoscope. 1981;91:83.
145 Jones GOM, Hale DE, Wasmuth CE, et al. A survey of acute complications associated with endotracheal intubation. Cleve Clin Q. 1968;35:23.
146 Kirchner JA, Sasaki CT. Fusion of the vocal cords following intubation and tracheostomy. Trans Am Acad Ophthalmol Otolaryngol. 1973;77:ORL88.
147 van Klarenbosch J, Meyer J, de Lange JJ. Tracheal rupture after tracheal intubation. Br J Anaesth. 1994;73:550.
148 Kastanos N, Miro RE, Perez AM, et al. Laryngotracheal injury due to endotracheal intubation: Incidence, evolution, and predisposing factors. A prospective long-term study. Crit Care Med. 1983;11:362.
149 Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy: A prospective study of 150 critically ill adult patients. Am J Med. 1981;70:65.
150 Jordon WS, Graves CL, Elwyn RA. New therapy for postintubation laryngeal edema and tracheitis in children. JAMA. 1970;212:585.
151 Pender JW. Endotracheal intubation in children: Advantages and disadvantages. Anesthesiology. 1954;15:495.
152 Sippel M, Putensen C, Hirner A, Wolff M. Tracheal rupture after endotracheal intubation: Experience with management in 13 cases. Thorac Cardiovasc Surg. 2006;54:51.
153 Seitz PA, Gravenstein N. Endobronchial rupture from endotracheal reintubation with an endotracheal tube guide. J Clin Anesth. 1989;1:214.
154 O’Donnell JM. Orotracheal tube intracuff pressure initially and during anesthesia including nitrous oxide. CRNA. 1995;6:79.
155 Harris R, Joseph A. Acute tracheal rupture related to endotracheal intubation: Case report. J Emerg Med. 2000;18:35.
156 Tessler S, Kupfer Y, Lerman A, et al. Massive gastric distention in the intubated patient: A marker for a defective airway. Arch Intern Med. 1990;150:318.
157 LoCicero J, III. Tracheo-carotid artery erosion following endotracheal intubation. J Trauma. 1984;24:907.
158 Howland WS, Lewis JS. Postintubation granulomas of the larynx. Cancer. 1956;9:1244.
159 Snow JC, Harano M, Balough K. Postintubation granuloma of the larynx. Anesth Analg. 1966;45:425.
160 Geffin B, Bland J, Grillo HC. Anesthetic management of tracheal resection and reconstruction. Anesth Analg. 1969;48:884.
161 Webb WR, Ozdemir IA, Ikins PM, et al. Surgical management of tracheal stenosis. Ann Surg. 1974;179:819.
162 Badran I, Jamal M. Pneumomediastinum due to Venturi system during microlaryngoscopy. Middle East J Anesthesiol. 1988;9:561.
163 Chang JL, Bleyaert A, Bedger R. Unilateral pneumothorax following jet ventilation during general anesthesia. Anesthesiology. 1980;53:244.
164 Egol A, Culpepper JA, Snyder JV. Barotrauma and hypotension resulting from jet ventilation in critically ill patients. Chest. 1985;88:98.
165 O’Sullivan TJ, Healy GB. Complications of Venturi jet ventilation during microlaryngeal surgery. Arch Otolaryngol. 1985;111:127.
166 Wetmore SJ, Key JM, Suen JY. Complications of laser surgery for laryngeal papillomatosis. Laryngoscope. 1985;95(Pt 1):798.
167 Cook TM, Bigwood B, Cranshaw J. A complication of transtracheal jet ventilation and use of the Aintree intubation catheter during airway resuscitation. Anaesthesia. 2006;61:692.
168 Laxton CH, Kipling R. Lingual nerve paralysis following the use of the laryngeal mask airway. Anaesthesia. 1996;51:869.
169 Ahmad NS, Yentis SM. Laryngeal mask airway and lingual nerve injury. Anaesthesia. 1996;51:707.
170 Salathé M, Johr M. Unsuspected cervical fractures: A common problem in ankylosing spondylitis. Anesthesiology. 1989;70:869.
171 Ghafoor AU, Martin TW, Gopalakrishnan S, Viswamitra S. Caring for the patients with cervical spine injuries: What have we learned? J Clin Anesth. 2005;17:640.
172 Cloward RB. Acute cervical spine injuries. Clin Symp. 1980;32:3.
173 Podolsky S, Baraff LJ, Simon RR, et al. Efficacy of cervical spine immobilization methods. J Trauma. 1983;23:461.
174 Riggins RS, Kraus JF. The risk of neurologic damage with fractures of the vertebrae. J Trauma. 1977;17:126.
175 Hastings RH, Kelley SD. Neurologic deterioration associated with airway management in a cervical spine-injured patient. Anesthesiology. 1993;78:580.
176 Crosby ET, Lui A. The adult cervical spine: Implications for airway management. Can J Anaesth. 1990;37:77.
177 Williams JP, Somerville GM, Miner ME, et al. Atlanto-axial subluxation and trisomy-21: Another perioperative complication. Anesthesiology. 1987;67:253.
178 Dong ML. Arnold-Chiari malformation type I appearing after tonsillectomy. Anesthesiology. 1987;67:120.
179 Gild WM, Posner KL, Caplan RA, et al. Eye injuries associated with anesthesia: A closed claims analysis. Anesthesiology. 1992;76:204.
180 Snow JC, Kripke BJ, Norton ML, et al. Corneal injuries during general anesthesia. Anesth Analg. 1975;54:465.
181 Batra YK, Bali IM. Corneal abrasions during general anesthesia. Anesth Analg. 1977;56:363.
182 Watson WJ, Moran RL. Corneal abrasion during induction [letter]. Anesthesiology. 1987;66:440.
183 Martin DP, Weingarten TN, Gunn PW, et al. Performance improvement system and postoperative corneal injuries: Incidence and risk factors. Anesthesiology. 2009;111:320.
184 Cheney FW, Posner KL, Caplan RA. Adverse respiratory events infrequently leading to malpractice suits. Anesthesiology. 1991;75:932.
185 Caplan RA, Posner KL, Ward RJ, et al. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828.
186 Takeda T, Tanigawa K, Tanaka H, et al. The assessment of three methods to verify tracheal tube placement in the emergency setting. Resuscitation. 2003;56:153.
187 Zbinden S, Schupfer G. Detection of oesophageal intubation: The cola complication [letter]. Anaesthesia. 1989;44:81.
188 Sum-Ping ST, Mehta MP, Anderton JM. A comparative study of methods of detection of esophageal intubation. Anesth Analg. 1989;69:627.
189 Birmingham PK, Cheney FW, Ward RJ. Esophageal intubation: A review of detection techniques. Anesth Analg. 1986;65:886.
190 Eldor J, Ofek B, Abramowitz HB. Perforation of oesophagus by tracheal tube during resuscitation. Anaesthesia. 1990;45:70.
191 Johnson KG, Hood DD. Esophageal perforation associated with endotracheal intubation. Anesthesiology. 1986;64:281.
192 Kras JF, Marchmont-Robinson H. Pharyngeal perforation during intubation in a patient with Crohn’s disease. J Oral Maxillofac Surg. 1989;47:405.
193 Levine PA. Hypopharyngeal perforation: An untoward complication of endotracheal intubation. Arch Otolaryngol. 1980;106:578.
194 Majumdar B, Stevens RW, Obara LG. Retropharyngeal abscess following tracheal intubation. Anaesthesia. 1982;37:67.
195 Norman EA, Sosis M. Iatrogenic oesophageal perforation due to tracheal or nasogastric intubation. Can Anaesth Soc J. 1986;33:222.
196 à Wengen DF. Piriform fossa perforation during attempted tracheal intubation. Anaesthesia. 1987;42:519.
197 Young PN, Robinson JM. Cellulitis as a complication of difficult tracheal intubation [letter]. Anaesthesia. 1987;42:569.
198 Gamlin F, Caldicott LD, Shah MV. Mediastinitis and sepsis syndrome following intubation. Anaesthesia. 1994;49:883.
199 Reyes G, Galvis AG, Thompson JW. Esophagotracheal perforation during emergency intubation. Am J Emerg Med. 1992;10:223.
200 Kramer MR, Melzer E, Sprung CL. Unilateral pulmonary edema after intubation of the right mainstem bronchus. Crit Care Med. 1989;17:472.
201 Mehta S. Guided orotracheal intubation in the operating room using a lighted stylet [letter]. Anesthesiology. 1987;66:105.
202 Conrardy PA, Goodman LR, Lainge F, et al. Alteration of endotracheal tube position: Flexion and extension of the neck. Crit Care Med. 1976;4:7.
203 Owen RL, Cheney FW. Endobronchial intubation: A preventable complication. Anesthesiology. 1987;67:255.
204 Benumof JL, Partridge BL, Salvatierra C, et al. Margin of safety in positioning modern double-lumen endotracheal tubes. Anesthesiology. 1987;67:729.
205 Rajan GR. Tracheal perforation with modified Broncho-Cath: Is it the tube or the technique? Anesth Analg. 2005;100:291.
206 Yüceyar L, Kaynak K, Cantürk E, Aykaç B. Bronchial rupture with a left-sided polyvinylchloride double-lumen tube. Acta Anaesthesiol Scand. 2003;47:622.
207 Blanc VF, Tremblay NAG. The complications of tracheal intubation: A new classification with a review of the literature. Anesth Analg. 1974;53:202.
208 Rosenberg H, Rosenberg HK. Airway obstruction and causes of difficult intubation. In: Orkin FK, Cooperman LH. Complications in anesthesiology. Philadelphia: Lippincott; 1983:125.
209 Ehrenpreis MB, Oliverio RM, Jr. Endotracheal tube obstruction secondary to oral preoperative medication. Anesth Analg. 1984;63:867.
210 Cook WP, Schultetus RR. Obstruction of an endotracheal tube by the plastic coating sheared from a stylet. Anesthesiology. 1985;62:803.
211 Zmyslowski WP, Kam D, Simpson GT. An unusual cause of endotracheal tube obstruction [letter]. Anesthesiology. 1989;70:883.
212 Sapsford DJ, Snowdon SL. If in doubt, take it out: Obstruction of tracheal tube by prominent aortic knuckle. Anaesthesia. 1985;40:552.
213 Populaire C, Robard S, Souron R. An armoured endotracheal tube obstruction in a child. Can J Anaesth. 1989;36(Pt 1):331.
214 Wright PJ, Mundy JVB, Mansfield CJ. Obstruction of armoured tracheal tubes: Case report and discussion. Can J Anaesth. 1988;35:195.
215 Treffers R, de Lange JJ. An unusual case of cuff herniation. Acta Anaesthesiol Belg. 1989;40:87.
216 Kendall AP, Lin E. Respiratory failure as presentation of achalasia of the esophagus. Anaesthesia. 1991;46:1039.
217 Westbrook JL. Oesophageal achalasia causing respiratory obstruction. Anaesthesia. 1992;47:38.
218 McConnell MS, Finn JC, Feeley TW. Tension hydrothorax during laparoscopy in a patient with ascites. Anesthesiology. 1994;80:1390.
219 Gallagher ML, Roberts-Fox M. Respiratory and circulatory compromise associated with acute hydrothorax during operative hysteroscopy. Anesthesiology. 1993;79:1129.
220 Cooper JB, Newbower RS, Kitz RJ. An analysis of major errors and equipment failures in anesthesia management: Considerations for prevention and detection. Anesthesiology. 1984;60:34.
221 Raphael DT, Weller RS, Doran DJ. A response algorithm for the low-pressure alarm condition. Anesth Analg. 1988;67:876.
222 Paix AD, Williamson JA, Runciman WB. Crisis management during anaesthesia: Difficult intubation. Qual Saf Health Care. 14(e5), 2005.
223 Snow JC, Norton ML, Saluja TS, et al. Fire hazard during CO2 laser microsurgery on the larynx and trachea. Anesth Analg. 1976;55:146.
224 Ossoff ARG. Laser safety in otolaryngology: Head and neck surgery—Anesthetic and educational considerations for laryngeal surgery. Laryngoscope. 1989;99(Suppl 48):1.
225 Hirshman CA, Smith J. Indirect ignition of the endotracheal tube during carbon dioxide laser surgery. Arch Otolaryngol. 1980;106:639.
226 Pashayan AG, Gravenstein N. High incidence of CO2 laser beam contact with the tracheal tube during operations on the upper airway. J Clin Anesth. 1989;1:354.
227 Henn-Beilharz A, Hagen R. Besonderheiten der Atemwegssicherung in der Hals-Nasen-Ohren-Heilkunde. In: Krier C, Georgi R. Airway management. Stuttgart: Thieme, 2001.
228 Sesterhenn AM, Dünne AA, Braulke D, et al. Value of endotracheal tube safety in laryngeal laser surgery. Lasers Surg Med. 2003;32:384.
229 Pashayan AG, SanGiovanni C, Davis LE. Positive end-expiratory pressure lowers the risk of laser-induced polyvinyl chloride tracheal-tube fires. Anesthesiology. 1993;79:83.
230 Wolf GL, Simpson JI. Flammability of endotracheal tubes in oxygen and nitrous oxide enriched atmosphere. Anesthesiology. 1987;67:236.
231 Pashayan AG, Gravenstein JS, Cassisi NJ, et al. The helium protocol for laryngotracheal operations with CO2 laser: A retrospective review of 523 cases. Anesthesiology. 1988;68:801.
232 Kaplan MB, Hagberg CA, Ward DS, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357.
233 Hemmerling TM, Bracco D. Subcutaneous cervical and facial emphysema with the use of the Bonfils fiberscope and high-flow oxygen insufflation. Anesth Analg. 2008;106:260.
234 Mehta S. Transtracheal illumination for optimal tracheal tube placement: A clinical study. Anaesthesia. 1989;44:970.
235 Agrò F, Hung OR, Cataldo R, et al. Lightwand intubation using the Trachlight: A brief review of current knowledge. Can J Anaesth. 2001;48:592.
236 Anwer HM, Zeitoun IM, Shehata EA. Submandibular approach for tracheal intubation in patients with panfacial fractures. Br J Anaesth. 2007;98:835.
237 Chandu A, Witherow H, Stewart A. Submental intubation in orthognathic surgery: Initial experience. Br J Oral Maxillofac Surg. 2008;46:561.
238 Dhara SS. Retrograde tracheal intubation. Anaesthesia. 2009;64:1094.
239 Kalinske RW, Parker RH, Brandt D. Diagnostic usefulness and safety of transtracheal aspiration. N Engl J Med. 1967;276:604.
240 Unger KM, Moser KM. Fatal complication of transtracheal aspiration: A report of two cases. Arch Intern Med. 1973;132:437.
241 Spencer CD, Beaty HN. Complications of transtracheal aspiration. N Engl J Med. 1972;286:304.
242 Schillaci CR, Iacovoni VF, Conte RS, et al. Transtracheal aspiration complicated by fatal endotracheal hemorrhage. N Engl J Med. 1976;295(9):48.
243 Poon YK. Case history number 89: A life-threatening complication of cricothyroid membrane puncture. Anesth Analg. 1976;55:298.
244 Massey JY. Complications of transtracheal aspiration: A case report. J Ark Med Soc. 1971;67:254.
245 Sanchez A. Retrograde intubation technique. In: Benumof JL, ed. Airway management: Principles and practice. St Louis: Mosby, 1996.
246 Faithfull NS. Injury to terminal branches of the trigeminal nerve following tracheal intubation. Br J Anaesth. 1985;57:535.
247 Parmet JL, Metz S. Anesthesiology issues in general surgery. Retrograde endotracheal intubation: an underutilized tool for management of the difficult airway. Contemp Surg. 49(5), 1996.
248 Scrase I, Woollard M. Needle vs surgical cricothyrotomy: A short cut to effective ventilation. Anaesthesia. 2006;61:962.
249 Craft TM, Chambers PH, Ward ME, et al. Two cases of barotrauma associated with transtracheal jet ventilation. Br J Anaesth. 1990;64:524.
250 Schumacher P, Stotz G, Schneider M, et al. Laryngospasm during transtracheal high frequency jet ventilation. Anaesthesia. 1992;47:855.
251 Oliverio R, Jr., Ruder CB, Fermon C, et al. Pneumothorax secondary to ball-valve obstruction during jet ventilation. Anesthesiology. 1979;51:255.
252 Smith RB, Schaer WB, Pfaeffle H. Percutaneous transtracheal ventilation for anesthesia: A review and report of complications. Can J Anaesth. 1975;22:607.
253 Braverman I, Sichel JY, Halimi P, et al. Complication of jet ventilation during microlaryngeal surgery. Ann Otol Rhinol Laryngol. 1994;103(Pt 1):624.
254 Benumof JL, Scheller MS. The importance of transtracheal jet ventilation in the management of the difficult airway. Anesthesiology. 1989;71:769.
255 Thomas T, Zornow M, Scheller MS, et al. The efficacy of three different modes of transtracheal ventilation in hypoxic hypercarbic swine. Can J Anaesth. 1988;35(Suppl):61.
256 Ciaglia P, Firsching R, Syniec C. Elective percutaneous dilatational tracheostomy: A new simple bedside procedure. Preliminary report. Chest. 1985;87:715.
257 Griggs WM, Worthley LIG, Gilligan JE, et al. A simple percutaneous tracheostomy technique. Surg Gynecol Obstet. 1990;170:543.
258 Fantoni A, Ripamonti D. A non-derivative, non-surgical tracheostomy: The translaryngeal method. Intensiv Care Med. 1997;23:386.
259 Frova G, Quintel M. A new simple method for percutaneous tracheostomy: Controlled rotating dilation. A preliminary report. Intensive Care Med. 2002;28:299.
260 Gromann TW, Birkelbach O, Hetzer R. Balloon dilatational tracheostomy: Initial experience with the Ciaglia Blue Dolphin method. Anesth Analg. 2009;108:1862.
261 Dempsey GA, Grant CA, Jones TM. Percutaneous tracheostomy: A 6 yr prospective evaluation of the single tapered dilator technique. Br J Anaesth. 2010;105:782.
262 Saayman AG, Findlay GP, Barnes RA, et al. Bacteraemia following single-stage percutaneous dilatational tracheostomy. Intensive Care Med. 2009;35:1970.
263 Wain JC, Wilson DJ, Mathieon DJ. Clinical experience with minitracheostomy. Ann Thorac Surg. 1990;49:881.
264 Bedford RF. Circulatory responses to tracheal intubation. Probl Anesth. 1998;2:201.
265 Latorre F, Hofmann M, Kleemann PP, et al. Fiberoptic intubation and stress. Anaesthetist. 1993;42:423.
266 Oczenski W, Krenn H, Dahaba AA, et al. Hemodynamic and catecholamine stress responses to insertion of the Combitube, laryngeal mask airway or tracheal intubation. Anesth Analg. 1999;88:1389.
267 Wilson IG, Fell D, Robinson SL, et al. Cardiovascular responses to insertion of the laryngeal mask. Anaesthesia. 1992;47:300.
268 Wood ML, Forrest ET. The haemodynamic response to the insertion of the laryngeal mask airway: A comparison with laryngoscopy and tracheal intubation. Acta Anaesthesiol Scand. 1994;38:510.
269 Hamaya Y, Dohi S. Differences in cardiovascular response to airway stimulation at different sites and blockade of the responses by lidocaine. Anesthesiology. 2000;93:95.
270 Horak J, Weiss S. Emergent management of the airway: New pharmacology and control of comorbidities in cardiac disease, ischemia and valvular heart disease. Crit Care Clin. 2000;16:411.
271 Edwards ND, Alford AM, Dobson PM, et al. Myocardial ischaemia during tracheal intubation and extubation. Br J Anaesth. 1994;73:537.
272 Imai M, Matsumara C, Hanoka Y, et al. Comparison of cardiovascular responses to airway management: Fiberoptic intubation using a new adapter, laryngeal mask insertion, or conventional laryngoscopic intubation. J Clin Anesth. 1995;7:14.
273 Rex MAE. A review of the structural and functional basis of laryngospasm and a discussion of the nerve pathways involved in the reflex and its clinical significance in man and animals. Br J Anaesth. 1970;42:891.
274 Fink BR. Laryngeal complications of general anesthesia. In: Orkin FK, Cooperman LH. Complications in anesthesiology. Philadelphia: Lippincott, 1983.
275 Al-Metwalli RR, Mowafi HA, Ismail SA. Gentle chest compression relieves extubation laryngospasm in children. J Anesth. 2010;24:854.
276 Al-alami AA, Zestos MM, Baraka AS. Pediatric laryngospasm: Prevention and treatment. Curr Opin Anaesthesiol. 2009;22:388.
277 Dohi S, Gold MI. Pulmonary mechanics during general anesthesia: The influence of mechanical irritation on the airway. Br J Anaesth. 1979;51:205.
278 Macklem PT, Mead J. Resistance of central and peripheral airways measured by a retrograde catheter. J Appl Physiol. 1967;22:395.
279 Kumeta Y, Hattori A, Mimura M, et al. A survey of perioperative bronchospasm in 105 patients with reactive airway disease. Masui. 1995;44:396.
280 Brimacombe JR. Analyses of 1500 laryngeal mask uses by one anaesthetist in adults undergoing routine anaesthesia. Anaesthesia. 1996;51:76.
281 Gonzalez RM, Bjerke RJ, Drobycki T, et al. Prevention of endotracheal tube-induced coughing during emergence from general anesthesia. Anesth Analg. 1994;79:792.
282 Williams B. Cerebrospinal fluid pressure changes in response to coughing. Brain. 1976;99:331.
283 Donlon JV. Anesthesia and eye, ear, nose, and throat surgery. In: Miller RD, ed. Anesthesia. ed 3. New York: Churchill Livingstone; 1990:2004.
284 Engelhardt T, Webster NR. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth. 1999;83:453.
285 Brimacombe J, Berry A. The incidence of aspiration associated with the laryngeal mask airway: A meta-analysis of published literature. J Clin Anesth. 1993;7:297.
286 Pothmann W. Der nicht nüchterne Patient. In: Krier C, Georgi R. Airway management. Stuttgart: Thieme, 2001.
287 Georgescu A, Miller JN, Lecklitner ML. The Sellick maneuver causing complete airway obstruction. Anesth Analg. 1992;74:457.
288 Shorten GD, Alfille PH, Gliklich RE. Airway obstruction following application of cricoid pressure. J Clin Anesth. 1991;3:403.
289 El-Orbany M, Connolly LA. Rapid sequence induction and intubation: Current controversy. Anesth Analg. 2010;110:1318.
290 Kilickan L, Baykara N, Gurkan Y, et al. The effect on intraocular pressure of endotracheal intubation or laryngeal mask use during TIVA without the use of muscle relaxants. Acta Anaesthesiol Scand. 1999;43:343.
291 Bharti N, Mohanty B, Bithal PK, et al. Intra-ocular pressure changes associated with intubation with the intubating laryngeal mask airway compared with conventional laryngoscopy. Anaesth Intensive Care. 2008;36:431.
292 Schafer R, Klett J, Auffarth G, et al. Intraocular pressure more reduced during anesthesia with propofol than with sevoflurane: both combined with remifentanil. Acta Anasthesiol Scand. 2002;46:703.
293 Georgiou M, Parlapani A, Argiriadou H, et al. Sufentanil or clonidine for blunting the increase in intraocular pressure during rapid-sequence induction. Eur J Anaesthesiol. 2002;19:819.
294 Robinson N, Clancy M. In patients with head injury undergoing rapid sequence intubation, does pretreatment with intravenous lignocaine/lidocaine lead to an improved neurological outcome? A review of the literature. Emerg Med J. 2001;18:453.
295 Kerwin AJ, Croce MA, Timmons SD, et al. Effects of fiberoptic bronchoscopy on intracranial pressure in patients with brain injury: A prospective clinical study. J Trauma. 2000;48:878.
296 Gerhardt T, Bancalari E. Apnea of prematurity: I. Lung function and regulation of breathing. Pediatrics. 1984;74:58.
297 Vervloet D, Magnan A, Birnbaum J, et al. Allergic emergencies seen in surgical suites. Clin Rev Allergy Immunol. 1999;17:459.
298 Hepner DL, Castells MC. Latex allergy: An update. Anesth Analg. 2003;96:1219.
299 Kurup VP, Fink JN. The spectrum of immunologic sensitisation in latex allergy. Allergy. 2001;56:2.
300 Garabrant DH, Schweitzer S. Epidemiology of latex sensitization and allergies in health care workers. J Allergy Clin Immunol. 2002;110:S82.
301 Randel GI. Latex allergy: Who is next? ASA Newsletter. 61(5), 1997.
302 Brown RH, Schauble JF, Hamilton RG. Prevalence of latex allergy among anesthesiologists: Identification of sensitized but asymptomatic individuals. Anesthesiology. 1998;89:287.
303 Kelly KJ, Kurup VP, Reijula KE, Fink JN. The diagnosis of natural rubber latex allergy. J Allergy Clin Immunol. 1994;93:813.
304 Diaz-Perales A, Collada C, Blanco C, et al. Cross-reactions in the latex-fruit syndrome: A relevant role of chitinases but not of complex asparagine-linked glycans. J Allergy Clin Immunol. 1999;104:681.
305 Garcia Ortiz JC, Moyano JC, Alvarez M, et al. Latex allergy in fruit allergic patients. Allergy. 1999;53:532.
306 Bidwai AV, Bidwai VA, Rogers CR, et al. Blood pressure and pulse-rate responses to endotracheal extubation with and without prior injection of lidocaine. Anesthesiology. 1979;51:171.
307 Wohlner EC, Usubiaga LJ, Jacoby RM, et al. Cardiovascular effects of extubation [abstract]. Anesthesiology. 1979;51:S194.
308 Cooper RM. Extubation and changing endotracheal tubes. In: Benumof JL, ed. Airway management: Principles and practice. St. Louis: Mosby; 1996:866.
309 Muzzi DA, Black S, Losasso TJ, et al. Labetalol and esmolol in the control of hypertension after intracranial surgery. Anesth Analg. 1990;70:68.
310 Coriat P, Mundler O, Bousseau D, et al. Response of left ventricular ejection fraction to recovery from general anesthesia: Measurement by gated radionuclide angiography. Anesth Analg. 1986;65:593.
311 Miyazaki M, Kadoi Y, Saito S. Effects of landiolol, a short-acting beta-1 blocker, on hemodynamic variables during emergence from anesthesia and tracheal extubation in elderly patients with and without hypertension. J Anesth. 2009;23:483.
312 Olsson GL, Hallen B. Laryngospasm during anaesthesia: A computer-aided incidence study in 136,929 patients. Acta Anaesthesiol Scand. 1984;28:567.
313 Valley RD, Freid EB, Bailey AG, et al. Tracheal extubation of deeply anesthetized pediatric patients: A comparison of desflurane and sevoflurane. Anesth Analg. 2003;96:1320.
314 Koga K, Asai T, Vaughan RS, Latto IP. Respiratory complications associated with tracheal extubation. Anaesthesia. 1998;53:540.
315 Hartley M, Vaughan RS. Problems associated with tracheal extubation. Br J Anaesth. 1993;71:561.
316 Khemani RG, Randolph A, Markovitz B. Corticosteroids for the prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev. 8, 2009. CD001000
317 Tolley NS, Cheesman TD, Morgan D, et al. Dislocated arytenoid: An intubation-induced injury. Ann R Coll Surg Engl. 1990;72:353.
318 Broccard AF, Liaudet L, Aubert JD, et al. Negative pressure post-tracheal extubation alveolar hemorrhage. Anesth Analg. 2001;92:273.
319 Burgess GE, III., Cooper JR, Jr., Marino RJ, et al. Laryngeal competence after tracheal extubation. Anesthesiology. 1976;51:73.
320 O’Sullivan JC, Wells DG, Wells GR. Difficult airway management with neck swelling after carotid endarterectomy. Anaesth Intensive Care. 1986;14:460.
321 Geelhoed GW. Tracheomalacia from compressing goiter: Management after thyroidectomy. Surgery. 1988;104:1100.
322 Wade JS. Cecil Joll lecture, 1979: Respiratory obstruction in thyroid surgery. Ann R Coll Surg Engl. 1980;62:15.
323 Batra YK, Gupta SK, Rajeev S. Tracheomalacia due to short term ventilation after total hip arthroplasty in an adult with long standing goiter. Anesth Analg. 2007;105:1867.
324 Debain JJ, Le Brigand H, Binet JP. Quelques incidents et accidents de l’intubation trachéale prolongué. Ann Otolaryngol Chir Cervicofac. 1968;85:379.
325 Dryden GE. Circulatory collapse after pneumonectomy (an unusual complication from the use of a Carlens catheter): Case report. Anesth Analg. 1977;56:451.
326 Brisson H, Welter J, Wiel E, et al. Complication inhabituelle de l’extubation. Ann Fr Anesth Reanim. 2001;20:573.
327 Lee C, Schwartz S, Mok MS. Difficult extubation due to transfixation of a nasotracheal tube by a Kirschner wire. Anesthesiology. 1977;46:427.
328 Hilley MD, Henderson RB, Giesecke AH. Difficult extubation of the trachea. Anesthesiology. 1983;59:149.
329 Lang S, Johnson DH, Lanigan DT, Ha H. Difficult tracheal extubation. Can J Anaesth. 1989;36:340.
330 Fagraeus L. Difficult extubation following nasotracheal intubation. Anesthesiology. 1978;49:43.
331 Wynne DM, Marshall JN. Risk of accidental extubation with disposable tonsillectomy instruments. Br J Anaesth. 2002;89:659.
332 Sugiyama K, Yokoyama K. Displacement of the endotracheal tube caused by change of head position in pediatric anesthesia: Evaluation by fiberoptic bronchoscopy. Anesth Analg. 1996;82:251.
333 Christie JM, Dethlefsen M, Cane RD. Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth. 1996;8:289.
334 Betbese AJ, Perez M, Bak E, et al. A prospective study of unplanned endotracheal extubation in intensive care unit patients. Crit Care Med. 1998;26:1180.
335 Tanios MA, Epstein SK, Livelo J, Teres D. Can we identify patients at high risk for unplanned extubation? A large-scale multidisciplinary survey. Respir Care. 2010;55:561.
336 Chevron V, Menard JF, Richard JC, et al. Unplanned extubation: Risk factors of development and predictive criteria for reintubation. Crit Care Med. 1998;26:1049.
337 Kaplow R, Bookbinder M. A comparison of four endotracheal tube holders. Heart Lung. 1994;23:59.
338 Tominaga GT, Rudzwick H, Scannell G, et al. Decreasing unplanned extubations in the surgical intensive care unit. Am J Surg. 1995;170:586.
339 Clarke T, Evans S, Way P, et al. A comparison of two methods of securing an endotracheal tube. Aust Crit Care. 1998;11:45.
340 Goldik Z, Mecz Y, Bornstein J, et al. LMA insertion after accidental extubation. Can J Anaesth. 1995;42:1065.