CHAPTER 27 Complications of excimer surgery
Preoperative assessment
To protect the integrity of the corneal epithelium and postoperative wound healing, dry eye syndrome or uncontrolled blepharitis should be preoperatively treated. In patients with background of herpes keratitis, LASIK should only be performed after 1 year of inactivity without treatment and in absence of stromal disease. Consider oral antiviral prophylaxis1. Moreover, LASIK is contraindicated in anterior basement membrane dystrophy (ABMD), but photorefractive–phototherapeutic keratectomy (PRK-PTK) is an excellent option in myopic patients presenting recurrent epithelial erosions.
In-depth evaluation of corneal topography is a ‘must’ prior to refractive surgery to identify patients with risk of postoperative corneal ectasia. Corneal topographic warning signs include curvature abnormalities, thin central pachymetry, and/or asymmetry in peripheral pachymetry. Ablational corneal refractive procedures are contraindicated in such cases, except in particular situations. Due to the increased risk of visual disturbances and decreased quality of vision, the cornea should not be flattened to less than 36 D or steepened to more than 48 D2.
Intraoperative complications
The most frequent intraoperative complications are related to the creation of the lamellar corneal flap with the microkeratome. The incidence of intraoperative flap complications ranges from 0.3% to 5.7%, being most frequent at the beginning of the learning curve. Poor quality flaps include incomplete flaps, buttonholes, thin or irregular flaps, and free caps3.
Test all equipment before surgery to avoid complications. Flap diameter may be adjusted in relation to preoperative keratometric power. Flatter corneas have an increased risk of free caps or incomplete flaps, whereas steeper corneas are more prone to epithelial abrasions, buttonholes, and thin or irregular flaps4.
Postoperative complications
Flap distortions: microstriae, macrostriae, and flap dislocation
Only if detected and treated within the first 24 h of occurrence, it is possible to solve them. Lift the flap, clean the epithelium the gutter, float the flap with balanced salt solution (BSS), and smooth it back into position. If undetected or left untreated for 1 or more days, the folds become fixed due to epithelial remodeling over the folds and stromal collagen fibers contraction. De-epithelialization and swelling of the flap with sterile distilled water is essential to release fixed folds. Place a bandage contact lens (BCL) to stabilize the flap and reduce the risk of epithelial ingrowth. Prescribe topical antibiotics and steroids. If macrostriae persist despite hydration, traction and suturing of the flap are required. However, suturing itself may create new striae or induce regular or irregular astigmatism. In severe cases, amputating the flap or PTK may be effective5.
Epithelial ingrowth
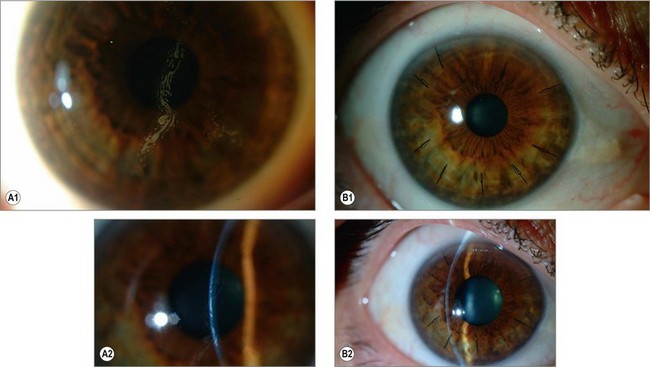
The benign form of presentation (grayish, small spots or lines at the peripheral edge of the flap) usually remains stable and is asymptomatic. On the other hand, a more diffuse form (cysts or sheaths of epithelium) may progress towards the center of the pupil and lead to irregular astigmatism (especially hyperopic astigmatism) and decreased visual acuity (Fig. 27.1).
Close follow-up is advised to rule out progression. Surgical intervention is indicated when the epithelial ingrowth progresses towards the visual axis or causes irregular astigmatism, or in presence of flap melting. Once the flap is lifted with a thin spatula, clean the epithelium from the stroma, the undersurface of the flap, and the edges of the wound. Then, carefully reposition and suture the flap. Place a BCL until the epithelium closes the wound5.
In severe forms or recurrences, several additive techniques have been used to eliminate potential residual cells in the stroma, and reduce the incidence of recurrences. These include the application of ethanol 20%–50% with a microsponge after cleaning the epithelium, PTK in the undersurface of the flap and the stromal bed, cryotherapy, or mitomycin C. However, we prefer not to use of any of them. In most series, reLASIK with a manual dissection technique (relift) is associated with a higher incidence (2–20%). On the other hand, its incidence seems to be lower after FS laser assisted LASIK both in primary and secondary cases. This is why we have explored the concept of FS laser assisted enhancements after a primary mechanical case6.
Visual-related complications
Quality of vision may be seriously affected if the ablation is not conveniently centered at the visual axis. Decentered ablations, central islands, small optical zones, or too flattened or too steepened corneas, will lead to both visual disturbances and decreased BSCVA due to increased higher order aberrations (irregular astigmatism). Always check the proper centration of the ablation and use an active eye tracker. If ablation problems were to occur, further topography-guided or wavefront-guided ablations may compensate for irregular astigmatism and topographic abnormalities7. However, severe cases require the use of rigid gas-permeable contact lenses (RGPCL) or anterior lamellar keratoplasty. Our favorite method to evaluate pre and postoperatively quality of vision is based on the double-pass technique (OQAS, Visiometrics SL)8,9.
Inflammation and/or infections
Diffuse lamellar keratitis, toxic syndrome, and GAPP syndrome
Diffuse lamellar keratitis (DLK) is a whitish, granular, culture negative, inflammatory response of the corneal lamellae that occurs in the early postoperative period in 0.67% of cases. Although still unclear, contaminants introduced in the lamellar interface during surgery, epithelial defects, and femtosecond laser may trigger the inflammatory cascade. Late-onset DLK has also been reported associated with epithelial defects, reactivation of herpetic keratitis, or viral keratoconjunctivitis10 DLK may cause scarring and visual loss11.
Prompt diagnosis and treatment are essential to avoid visual sequelae. The cellular reaction in the interface is usually apparent in the first 24 hours, and starts at the periphery of the lamellar flap5,11. It is important to differentiate DLK from punctate epithelial keratopathy (stains with fluorescein), or the presence of meibomian gland or tear film debris that become trapped under the flap (yellowish appearance).
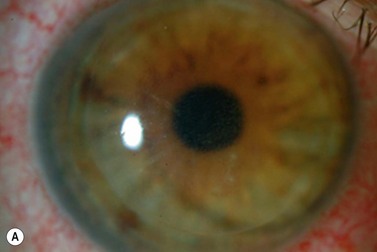
Stages 1 (white granular cells in the periphery of the flap, with sparing of the visual axis) and 2 (involving the visual axis in ‘sands of the Sahara’ appearance) require hourly topical steroids (prednisone) and daily monitoring. Most cases resolve in 7–10 days (Fig. 27.2A). Steroid-induced glaucoma may occur. If a pocket of fluid develops in the lamellar interface due to the increased IOP, the measurement of IOP by central Goldmann applanation tonometry appears falsely low, and IOP should be confirmed in the periphery of the cornea11.
Sonmez and Maloney described a new syndrome of unknown cause associated with excimer laser ablations (PRK and LASIK), the ‘toxic syndrome’: a non-inflammatory central corneal opacification with a significant hyperopic shift. The opacification gradually clears over a period of 2–18 months, leaving the eye hyperopic (more than +2D). Enhancement is indicated to treat residual hyperopia and remove residual striae. Corticosteroid treatment is not indicated12.
Infections
Infections after excimer laser surgery are very rare (0.02–1.5%), but may lead to moderate to severe visual loss in up to 49.4% of the eyes affected. Early-onset infections (≤7 days of surgery) occur in 49.4% of cases, and are generally caused by Gram-positive bacteria (S. aureus), whereas late-onset infections (≥10 days after surgery) represent 50.6% of cases, and are mainly caused by atypical mycobacteria (Mycobacterium chelonae) (Fig. 27.2B). Fungal infections are less frequent (up to 20% of late-onset cases), but may cause extremely severe infections that may end up in endophthalmitis and severe visual loss. Sources of infection include patients’ eyelids, surgical instruments, and postoperative inoculation by the patient.
Therapeutic penetrating or lamellar keratoplasty is rarely required. The main indications are: persistent, worsening infiltrate despite 2–12 weeks of medical therapy, progressive, uncontrolled corneal thinning or perforation, and scarring and irregular astigmatism13.
Corneal ectasia
Post-LASIK ectasia has an estimated incidence of 0.04–0.6%, and leads to irregular astigmatism and decrease of BSCVA. Risk factors include high myopia, residual stromal bed (RSB) thickness less than 250 µm, low preoperative corneal thickness, and forme frustre keratoconus. Young age and steep cornea are the main risk factors for ectasia development in patients with normal topography2.
As previously mentioned, corneal ablational procedures are absolutely contraindicated in patients with ectatic disorders (keratoconus and pellucid marginal degeneration) and abnormal topographic patterns including elevated I-S values (specially if greater than 1.4 D), asymmetric inferior corneal steepening, skewed radial axes above and below the horizontal meridian, and asymmetry of topographic patterns between eyes. Randleman et al. have developed a scoring system to preoperatively establish the risk for postoperative ectasia2.
1 de Rojas Silva V, Rodríguez-Conde R, Cobo-Soriano R, et al. Laser in situ keratomileusis in patients with a history of ocular herpes. J Cataract Refract Surg. 2007;33:1855-1859.
2 Randleman JB, Woodward M, Lynn MJ, et al. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115:37-50.
3 Lee JK, Nkyekyer EW, Chuck RS. Microkeratome complications. Curr Opin Ophthalmol. 2009;20:260-263.
4 Albelda-Valles JC, Marti-Reyes C, Ramos F, et al. Effect of preoperative keratometric power on intraoperative complications in LASIK in 34099 eyes. J Refract Surg. 2007;23:592-597.
5 Schallhorn SC, Amesbury EC, Tanzer DJ. Avoidance, recognition, and management of LASIK complications. Am J Ophthalmol. 2006;141:733-739.
6 Güell JL, Elies D, Gris O, et al. Femtosecond laser assisted enhancements after LASIK. Journal Cataract Refract Surgery. April 2011. In press
7 Reinstein DZ, Archer TJ, Gobbe M. Combined corneal topography and corneal wavefront data in the treatment of corneal irregularity and refractive error in LASIK or PRK using the Carl Zeiss Meditec MEL 80 and CRS-Master. J Refract Surg. 2009;25:503-515.
8 Güell JL, Pujol J, Arjona M, et al. OQAS: A new technique instrument for an objective clinical evaluation of the ocular optical quality. Correspondence. J Cataract Refract Surgry July. 2004;(30):1598-1600.
9 Vilaseca M, Padilla A, Ondategui J, et al. Effect of laser in situ keratomileusis on vision analyzed using preoperative Optical Quality. J Cataract Refrac Surg. 2010;36:1945-1953.
10 Gris O, Güell JL, Wolley-Dod C, et al. Diffuse lamellar keratitis and corneal edema associated with viral keratoconjunctivitis 2 years after laser in situ keratomileusis. J Cataract Refract Surg. 2004;30:1366-1370.
11 Knorz MC. Flap and interface complications in LASIK. Curr Opin Ophthalmol. 2002;13:242-245.
12 Sonmez B, Maloney RK. Central toxic keratopathy: description of a syndrome in laser refractive surgery. Am J Ophthalmol. 2007;143:420-427.
13 Chang MA, Jain S, Azar DT. Infections following laser in situ keratomileusis: an integration of the published literature. Surv Ophthalmol. 2004;49:269-280.