CHAPTER 12 Complex Therapeutic Hip Arthroscopy With the Use of a Femoral Distractor
Introduction
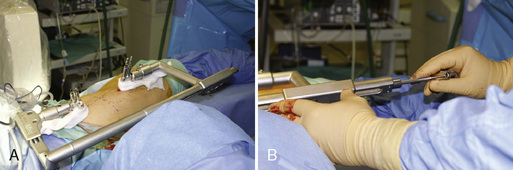
However, for such complex arthroscopic reconstructive surgery, longer traction times are necessary. It has been reported that traction times of more than 90 to 120 minutes on a traction table can provoke severe neurologic and perineal skin lesions in up to 15% of cases. The most frequent neurologic lesions reported are pudendal nerve lesions that result in clinical impotence as a result of the compression of the nerve on the perineal post of a traction table. Sciatic and femoral nerves are also at risk because of the overstretching that occurs during longer periods of time. Because these reconstructive procedures are time consuming, have a steep learning curve, and, above all, can provoke fearful complications, we have used invasive hip distraction (DR hip distractor, DR Medical, Solothurn, Switzerland) for these indications (Figure 12-1, A). Thus, by avoiding the need for traction against a perineal post with a traction table, we have not encountered the previously mentioned complications that occur with the use of the invasive hip distraction technique. The hip distractor allows the surgeon to perform these time-consuming surgical steps without the pressure of time to attain the same degree of perfection as occurs with open surgery. The results obtained are therefore identical to those of the open surgical technique. This is also a wonderful teaching tool, because beginners can also perform these more complex procedures without worrying about distraction time and the related complications.
Basic science
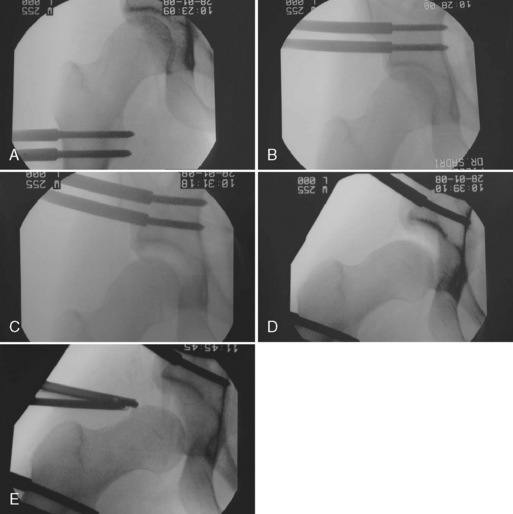
Sufficient hip distraction involves traction forces of about 250 N to 500 N. After the suction seal is broken, the force needed diminishes significantly. However, on a traction table, much of the traction force is lost by uselessly distracting the knee (about 5 mm) and ankle joints (another 5 mm). After the invasive hip distractor has been installed, it produces a traction force of 500 N exclusively on the hip joint; this force is calculated in the elasticity of the dedicated Schanz screws. After this traction force is attained, the dedicated Schanz screws will be seen on the image intensifier to start bending (Figure 12-2, A through D).
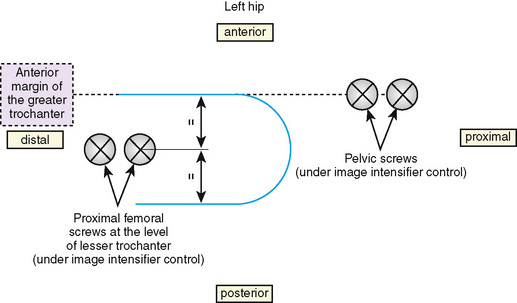
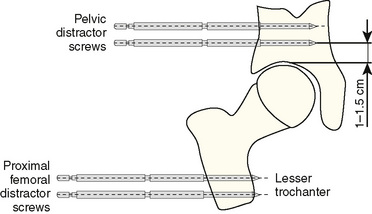
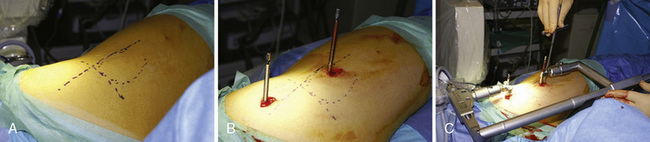
In addition, on a traction table, the femoral head has a tendency to slide anteriorly and to reduce the anterior joint space because of the acetabular anteversion. However, most often, the lesions are in the anterior and superior regions, and most surgeons prefer to internally rotate the lower extremity to avoid this anterior joint space narrowing on a traction table. Internal rotation moves the sciatic nerve anteriorly and thus puts it at risk if the surgeon chooses a posterolateral portal approach. Invasive hip distraction avoids this by allowing for a controlled anterior-to-posterior traction vector in neutral rotation (Figure 12-3, A and B). A posterolateral portal approach is thus very safe without putting the sciatic nerve at risk.
Indications
Surgical technique
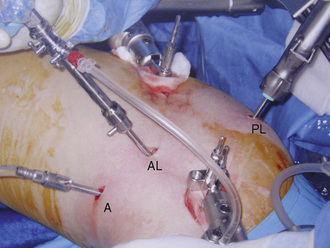
We have tried the lateral and supine approaches for this indication. We are largely in favor of the lateral decubitus position, and the setup is in a way that is similar to that of the classic lateral approach, with some differences. Three standard arthroscopy portals are used: the posterolateral portal, the anterolateral portal, and the anterior portal (Figure 12-4).
We have abandoned the use of a traction table for hip arthroscopy as a result of a high associated neurologic complication rate. Although we followed the standard recommendations to avoid the neurologic complications of hip arthroscopy that were found in the literature (e.g., the use of a very large perineal post), of our first 20 cases, two slowly regressive pudendal nerve lesions with clinical impotence were encountered. These complications were likely the result of the fact that more than 90 minutes of traction were used to correct complex acetabular anomalies. We now have experience with more than 1000 cases of hip arthroscopy, and, sadly, our operative and traction times have not changed; this is because more and more complex cases are operated on arthroscopically and because labral suturing is necessary in about a third of cases. In the case of labral suturing, an average of four anchors is necessary, with some cases requiring eight anchors; this anchoring is of course time consuming, and it puts the nerves at risk. For this reason, since 2000, we have been using an invasive hip distraction device (see Figure 12-1, A and B), which is still in use at our institution. The device avoids the use of the perineal post, which is responsible for the pudendal nerve lesions. For more than 1000 cases, we have not documented a single nerve lesion as a result of traction with this type of hip distraction. Neurologic complication rates from procedures that involve the use of traction tables can be as high as 10% to 15%. These complications are certainly also related to experience with the technique and thus also to traction times. However, as mentioned previously in the case of complex surgery, the acetabular corrective surgery can be time consuming, particularly if labral reattachment or autologous cartilage transplantation is involved.
We prefer the lateral approach and invasive hip distraction for the following practical reasons:
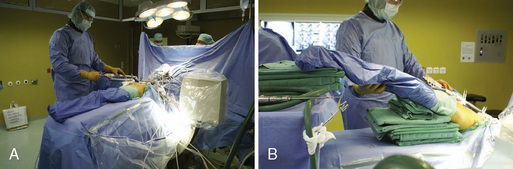
The lower extremity is draped so that it can be moved freely (Figure 12-5, A and B). The C-arm fluoroscope is brought under the table and draped, thus providing a good anterior-to-posterior view (see Figure 12-2, A through E, and 12-5, A and B). The invasive hip distractor is set up with the patient in slight hip flexion. One dedicated Schanz screw is placed 1 cm above the acetabular sourcil under image intensifier control, and another is placed at the level of the lesser trochanter. The proximal screws are in line with the anterior trochanteric margin (see Figure 12-3, A and B, and 12-6, B). The relative positions of the proximal and distal Schanz screws produce an anterior-to-posterior traction vector that optimizes the anterior joint space opening, even if no lower limb internal rotation is applied. The invasive hip distractor is installed on the inserted Schanz screws (see Figure 12-6, A through C). The device has a precision screw mechanism that can move the tubes precisely so that they fit onto the Schanz screws. After the distractor is installed, two other Schanz screws—one proximally in the acetabulum and one distally in the femur—are applied through the distractor’s guiding tubes (see Figure 12-6, C). This stabilizes the rotational forces and allows for a better anterior-to-posterior distraction vector. Bolts are then put on every Schanz screw to push the tubes around the screws down onto the bone. The whole hip distractor is thus an angularly stable construct that improves traction forces. After the invasive hip distractor is installed, distraction is applied on the hip by turning the axial distraction screw (see Figure 12-1, A and B). The lower extremity is then set in abduction of approximately 30 degrees to 45 degrees (see Figure 12-5, A and B). This maneuver and the previously mentioned slight flexion of about 10 degrees will relax the superior and anterior hip capsule, including the iliofemoral ligament, and this will permit better distraction (see Figure 12-5, B). With adequate distraction (ideally 12 mm), the hip joint is decompressed with a large spinal needle, and the suction seal is broken. However, about 5% of hips are considered not distractable or insufficiently distractable on traction tables. In these cases, invasive hip distraction can be useful by permitting for controlled capsular releases, which is described later in this chapter. With the use of a cannulated system, the arthroscope is first introduced into the anterolateral portal (see Figure 12-4). We prefer using the 70-degree scope, which provides a better view initially, especially in tighter joints. The posterolateral and anterior portals are then created under direct visual control, with the labrum and the femoral head being avoided. The hip is first viewed under air, and this is followed by fluid.
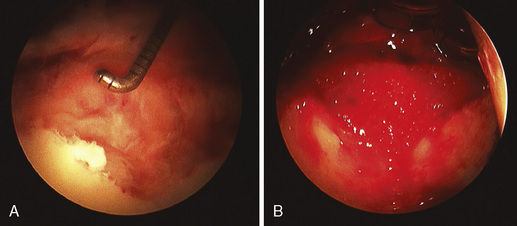
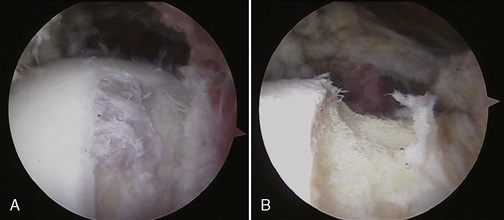
On the acetabular side, complex labral tears are debrided with an adequate shaver or an angulated radiothermal device (30 degrees or 60 degrees). The articular cartilage lesions are similarly debrided or smoothed to a stable area, and microfracture is performed when necessary. If the cartilage lesions of the acetabulum are larger than 3 cm2, we believe that cartilage transplantation techniques can be considered. We have used three-dimensional matrix-based transplantations, such as autologous chondrocyte transplantation with the use of a three-dimensional scaffold (M-ACT), autologous membrane-induced chondrogenesis, and scaffold-augmented microfracture. When M-ACT (Figure 12-7, A and B) is applied, we use the head–neck junction as the donor site for chondrocytes.
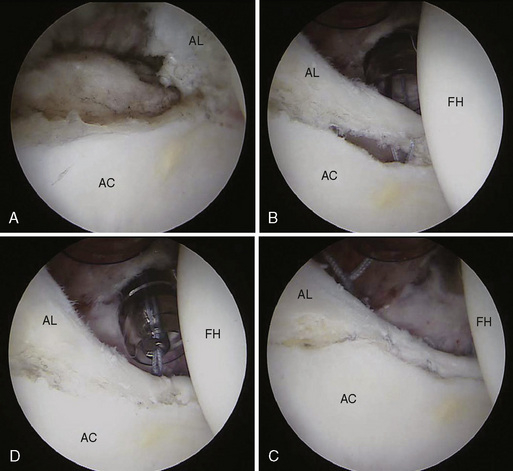
If the labrum can be preserved, which it typically can be in the case of articular longitudinal partial tears, it is detached from the acetabular rim to create a bucket-handle tear (Figure 12-8, A through D), as would be done during open surgery. Often, this reveals labral ossifications (see Figure 12-8, A). In the case of acetabular retroversion or labral ossifications, these are resected with a burr. Rarely, if no acetabular version anomaly or labral ossification is present, the acetabular bone rim is freshened with a burr. In the former and the latter cases, the labrum is then reinserted (see Figure 12-8, A through D) with the use of impacted bioabsorbable small anchors with high-traction–resistant nonabsorbable sutures (2.4-mm and 3.0-mm Bio-SutureTak or knotless 2.5-mm and 3.0-mm PushLock [Arthrex, Karlsfeld, Germany]). We prefer bioabsorbable anchors because they do not influence magnetic resonance imaging signals in case this type of imaging technique is needed in the future. In the case of future total hip arthroplasties, these anchors will not interfere with the implantation. Highly resistant sutures such as FiberWire (Arthrex, Germany) are essential because of the 360-degree angulation that is usually needed in the hip when suture management is required; absorbable sutures tend to break in this situation. In our experience, suture passers (Hip Low Profile Suture Lasso [Arthrex, Germany]) and shuttle techniques are the least aggressive methods of labral suturing. Indeed, the labrum is very thin in some cases, and bird-beak–type instruments are too bulky. Usually a minimum labral width of 5 mm seems to be the reasonable limit for reinsertion. It is essential to tie the knots on the extra-articular side of the joint (2.4-mm and 3.0-mm Bio-SutureTak [Arthrex, Germany]) so that they do not interfere with hip mechanics and thus preserve the cartilage. Knotless anchors can also be an advantage in that they avoid the presence of knots (2.5- mm and 3.0- mm PushLock [Arthrex, Germany]). Typically, the joint is viewed from the posterolateral portal, the drill comes in from the anterolateral portal, and shuttling (Hip Low Profile Suture Lasso [Arthrex, Germany]) is performed between the anterolateral and anterior portals or vice versa, depending on the region in which the suture is placed. Two long 8.25 mm × 90 mm or 8.25 mm × 110 mm transparent cannulas (hip disposable kits [Arthrex, Karlsfeld, Germany]) are used in the anterolateral and anterior portals.
After the labrum is treated by either resection or suture, the cartilage lesions are addressed. Depending on the size of the lesion, a decision is made to use a matrix-based treatment. Appropriate sized cannulas are also used with the same dimensions as previously mentioned. The matrix is then sutured to the labrum or placed on anchors at the rim with similar techniques (see Figure 12-7, A and B).
The traction is then reduced, and the head is viewed from the posterolateral portal. An anterior and superior capsulectomy is performed with the use of a punch and a very aggressive, large-diameter shaver (5.0 or 7.0 PITBULL shaver [DR Medical, Solothurn, Switzerland]) to visualize the anterior and superior portion of the head. Instruments are brought in through the anterolateral portal. The head–neck junction is inspected, and the fatty pars reflecta, which contains the nutrient vessels of the femoral head, is visualized. This is essential because this area contains the terminal branches of the medial circumflex artery, and it is thought to be the major blood supply of the femoral head. Typically, the impingement areas of the head–neck junction caused by the nonspheric portion of the femoral head are marked by chondral damage (Figure 12-9, A and B). This area will be resected with a burr in the anterolateral portal, which will render it concave (see Figure 12-9, B). After the resection is completed while viewing from the posterolateral portal, the viewing portal is switched to the anterolateral portal, the burr is brought in through the anterior portal, and the fluid outflow is changed to the posterolateral portal. The most important anterosuperior head correction is then initiated while viewing in this position. Medially, it is the medial synovial fold that usually marks the end of the head osteoplasty. This anterior area of the head–neck junction is indeed the major area in which impingement occurs, and it typically impinges during flexion and internal rotation.
During the procedure, fluoroscopy helps to quantify the head–neck junction resection. A depth of resection of 7 mm to 10 mm is usually required. However, the final dynamic testing of the hip is the most important step of the surgery. Typically, for a test of extreme flexion, extreme abduction, 90 degrees of flexion, and maximum internal rotation are necessary; this will detect whether the resection is sufficient or not. If the resection is not sufficient, it must be continued until impingement-free motion can be visually documented (Figure 12-10, A through C).
Beck M., Leunig M., Parvizi J., et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop.. 2004:67-73.
Byrd J.W., Pappas J.N., Pedley M.J. Hip arthroscopy: an anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy.. 1995;11:418-423.
Precise portal placement is described as a function of anatomy..
Espinosa N., Rothenfluh D.A., Beck M., et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg A.. 2006;88:925-935.
Funke E.L., Munzinger U. Complications in hip arthroscopy. Arthroscopy.. 1996;12:156-159.
Ganz R., Parvizi J., Beck M., et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop.. 2003;417:112-120.
Gautier E., Ganz K., Krugel N., et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br.. 2000;82:679-683.
The importance of the medial circumflex artery in femoral head vascularization is shown..
Glick J.M. Complications of hip arthroscopy by the lateral approach. In: Sherman O.H., Minkoff J., editors. Current management of complications in orthopaedics: arthroscopic surgery. Baltimore: Williams & Wilkins; 1990:193-201.
Langlais F., Lambotte J.C., Lannou R., et al. Hip pain from impingement and dysplasia in patients aged 20-50 years. Workup and role for reconstruction. Joint Bone Spine.. 2006;73:614-623.
Lavigne M., Parvizi J., Beck M., et al. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop.. 2004;418:61-66.
Principles for the treatment of femoroacetabular impingement are reported..
Sadri H. Eingriffe am Hyalinen Knorpel. In: Dienst M., editor. Hüftarthroscopie. Munich: Elsevier Urban & Fischer, 2009.
Sadri H, Menetrey J, Fritchy D, et al. Femoro-acetabular impingement: arthroscopic treatment compared with open surgery, a prospective randomized study. Clin Orthop. (accepted for publication)
Sadri H., Menetrey J., Kraus E., et al. Arthroskopische Behandlung des femoroazetabulären Impingements. Arthroskopie.. 2006;19:67-74. (German)
Arthroscopic techniques for and the results of treating femoro-acetabular impingement are reported..
Sampson T.G. Complications of hip arthroscopy. Clin Sports Med.. 2001;20:831-835.
This is the URL of the Web site of the creator of invasive hip distraction..