Chapter 9 Clinical information systems
Clinical record-keeping requires an integrated system to manage the information, including its acquisition during clinical care, and archiving and availability for future clinical, business and research uses.
The term ‘clinical information systems’ (CIS) refers to computerised systems for managing the clinical record, often within specialised areas of a hospital, such as intensive care, emergency medicine, operating theatres or cardiology. CIS for intensive care units (ICUs) have been developing since the late 1980s; however, their implementation has been limited by cost, functionality and clinician acceptance.1–8
The electronic medical record (EMR) and electronic health care records (EHR) embrace respective hospital and community-wide electronic systems for managing patient records which may be integrated with the more specialised CIS. Over the next decade we can expect to see EHR implementation throughout the health systems of the more developed nations. The driving incentive is community concern for safety and quality in health care and the EHR is the single most powerful measure to produce a safer, more effective and efficient health care system.8–12
In the UK the National Health Service (NHS) has embarked on an ambitious National Programme for Information Technology (NPfIT) featuring a national summary care record (SCR) or ‘spine’ to hold limited essential information on each consenting patient. Additional features include picture archiving and communication systems (PACS), more detailed data held on integrated local computer systems, electronic prescribing and computerised physician order entry (CPOE).13,14
The US government has placed a high priority on electronic health records, although progress will be uneven due to the fragmented nature of its health system. The Veterans Health Administration (VHA) has a system-wide EHR (VistA) that is closely integrated with its quality monitoring and enhancement programme and is delivering tangible results.15–17 Similarly, the Partners HealthCare System at the Brigham and Women’s Hospital and Massachusetts General Hospital has demonstrated real improvements in health care with cost and quality benefit outcomes.18–21
The coordination of effort in Europe will be similarly challenging, although the need is recognised by the European Commission. In Australia, the HealthConnect strategy is largely focused on broadband connections for primary health care providers and establishing data dictionaries and standards with limited strategies or funding for actual implementation of EHRs.22
FUNCTIONS AND ADVANTAGES OF CIS
CIS seek to deliver several key benefits (Table 9.1).23 These include the automation of repetitive manual tasks, improved accuracy through reductions in human error, attributable records simultaneously available from multiple points of care and integration with other bedside equipment and information systems. The built-in error checking and knowledge-based systems should also provide a safer and higher-quality clinical process. The CIS electronically capture the data and make this information potentially available to a multitude of systems. This obviates the need for repetitive manual data entry or transcription, while making the data accessible for a range of purposes which may include clinical, business and research reporting.
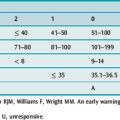
Table 9.1 Clinical information systems (CIS) benefits
The ICU is already a technology-rich environment, where bedside devices process and provide data elements in electronic format. Similarly, many clinical measurements are available on monitors, ventilators and pumps. Traditionally, these electronically derived values are transcribed on to observation charts and paper-based clinical records, as are repetitive clinical observations and arithmetic calculations which are often performed manually or with the aid of a calculator. The voluminous observation charts present a challenge for both storage and access, and transcription errors and arithmetic errors are prolific in these paper systems.
The CIS automates the process of electronic data collection from monitors, ventilators, infusion pumps, dialysis/filtration equipment, cardiac assist devices and other bedside devices and provides a real-time spreadsheet with arithmetic accuracy. Incorporation of clinical documentation and progress notes provides a legible and attributable record of events.
The patient record can then be accessed from geographically distant workstations in the ICU, the hospital, and even from other more remote sites. As long as the system is running, the record is easy to locate and always available.
A major contribution of CIS to clinical safety and quality is through the provision of an electronic prescribing and administration record for drugs and fluids. Errors in prescription and administration are a leading cause of adverse events with associated morbidity.18,24 CIS provide both legibility and varying levels of decision support which may include defining usual dosages and administration routes, suggesting dose modification in the setting of organ failures, or preventing prescribing in cases of known allergy or likely drug interaction.25
ARCHITECTURE AND COMPONENTS OF CIS
BASIC CIS ARCHITECTURE
All CIS share certain basic components consisting of workstations, a network and central servers (Figure 9.1). The user interface is presented at the workstation, which is usually at each bedside but may also be in nearby central and administrative areas, such as the nurses’ station, or more distant in the offices of clinical or administrative staff. Workstations commonly consist of relatively standard personal computer (PC) hardware being desk-, pendant or trolley-mounted, but may include laptops or personal digital assistants (PDAs) with wireless systems where technical challenges related to speed and reliabiltiy of data transmission can be overcome.
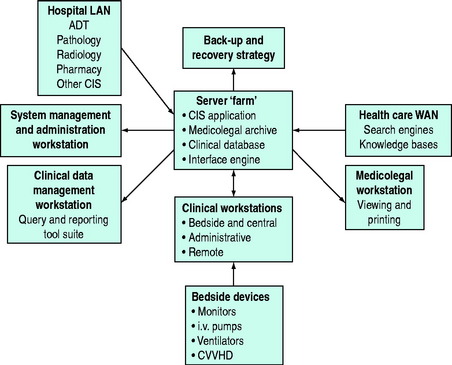
Figure 9.1 Clinical information systems architecture. LAN, local area network; WAN, wide area network; ADT, admission/discharge/transfer; CVHD, continuous venovenous haemodialysis.
Most CIS allow other applications, such as PACS, word processing or e-mail, to be run on the same PC, but this is potentially a rich source of system conflicts and requires careful administration.
Workstations are linked to each other and a centralised set of servers through a network of communication cables. Hubs, switches and routers control network traffic. A dedicated network, either actual or virtual, enhances system performance but it is important to ensure built-in redundancy in network loops and power sources to minimise potential interruptions from physical disruption or component failure.
The configuration of computer servers varies widely but it is common to have ‘paired’ or ‘mirrored’ servers, which duplicate their partner’s function. This provides protection from hardware failure, minimising system down time, and provides some degree of data protection. Servers have a finite capacity to process data from multiple workstations and other peripheral connections, and so larger systems may require multiple server pairs.
CIS usually require a separate workstation or server to manage the interfaces with other systems. These include hospital demographics (ADT systems for admission/discharge/transfer), pathology laboratory, pharmacy, radiology and hospital finance. Interfacing requires a software platform known as an interface engine. Additional software identifies the relevant data and directs and processes these data to the correct field in the appropriate format. Due to the huge variety of current and legacy systems, this process almost always requires custom-written code and programming, representing one of the major risks and expenses of systems integration.13
Bedside monitoring systems usually include a central station or server that can be linked with the CIS servers to transfer their downloaded information back to the bedside. Transferring data from other bedside devices is usually achieved by a cable connection from the device to a bedside concentrator in the patient bay. The connection requires an electronic decoder, specific to the manufacturer and model of the device. The concentrator must then communicate with the central servers via a subsidiary server that provides the software translator to complete the interface. A selection of established interfaces to commonly utilised equipment exists but often additional customised interfaces must be written.
MEDICOLEGAL STORAGE
Electronic data capture does not necessarily result in long-term electronic data storage. Many CIS sites have continued to require the printing-out of all reports from the patient episode to store in the paper-based hospital medical record. Modern servers have extensive storage capacity but this can be rapidly consumed by the equally enormous amount of data being collected from every patient. Some server pairs can only hold 2–3 months of data before data begin to be purged or overwritten. Although hard-disk memory is ever-increasing and more affordable, additional strategies such as more efficient databases or offline storage formats may be needed. When the choice of storage solution is made, it is equally important to be aware that the format of data storage is determined by the anticipated use of the data and to ensure that future software upgrades do not render the stored data unreadable.
Data archiving for medicolegal purposes requires that the clinical information be readily accessible and preferably presented in exactly the same format as it was recorded and reviewed by the clinicians during the episode of patient care. Any changes to the clinical record during the patient episode must be clearly displayed and attributable – this is known as an audit trail or change history. An audit trail is a standard feature of most CIS and actually offers improved accountability over paper-based systems. It may be desirable to make it impossible to alter the record after the patient episode, which requires specialised storage formats or strict access restrictions to the data archive.
Once the record is stored, by whatever method, it must be protected from accidental loss. This usually requires a carefully engineered and documented management plan with regular scheduled back-ups, off-site storage of duplicates and robust recovery strategies. When these requirements are fulfilled, the electronic medicolegal archive can readily exceed the performance of a paper-based record through its assured availability and authenticity.
CLINICAL DATABASE STORAGE
A major objective of CIS is to provide a comprehensive clinical database which will accumulate data in real time that can be stored and queried for a wide range of reports for a variety of purposes. The relevant data need to be held in an accessible and readily searchable database that will allow a variety of sophisticated reports to be prepared on both a scheduled and ad hoc basis. These requirements are quite different from those of medicolegal storage and usually require a separate form of data storage, commonly known as a clinical database, data repository, data warehouse or data management solution.
It may be desirable to adopt a significantly different database structure from the core CIS database which may have been designed with prospective user configurability in mind, rather than allowing easy location of data fields in a structure designed for rapidly processing queries. The design of the clinical database is a compromise between saving effectively the large amount of data collected while maintaining speed and ease of use in running queries. Even when the vendor has utilised an industry-standard database application, such as Oracle or SQL, in the core CIS application, designing and running queries may still present a challenging specialist task because of the complexity of the table structure or the huge amount of aggregated data.
The clinical data management solutions currently offered are quite diverse. One solution simply provides an industry-standard data transfer protocol (e.g. ‘ODBC driver’) as a means of accessing the data. The local circumstances of each hospital then dictate customised queries or secondary database designs for local use. Alternatively, an industry-standard query tool is used to generate reports from the core CIS database, but the number of queries that can be designed and preconfigured in this fashion is often limited, particularly as the user configurations of the CIS vary widely. There is inevitably a compromise between standardisation and flexibility. Data fields must be standardised in the configuration of the CIS to allow standard queries to be performed. Some CIS solutions offer a proprietary subsidiary database containing selected clinical data with a wider range of reports preconfigured into the query tool.
EVALUATION AND IMPLEMENTATION OF CIS
Clinicians frequently underestimate the managerial requirements, human resource demands and opportunity costs of CIS implementation.11 The process should be viewed as a major project requiring advanced planning and management skills (Table 9.2). The project team must be multidisciplinary, consult widely and consider workplace flows and processes, or else a suboptimal result is guaranteed, as has been demonstrated in the literature.26,27 The CIS will impact on medical, nursing, allied health, managerial and technical staff within the ICU, together with those from other clinical disciplines. Involvement of hospital information management and medical records staff is strongly recommended. Extensive documentation and continued scheduled reviews are required throughout the process.
Table 9.2 Clinical information systems (CIS) implementation
Business case development to secure funding is less problematic than previously and assisted by the quality benefits of CIS implementation.11,21 The most basic system can be expected to cost in the order of AUD $25 000–50 000 per bed, while more advanced systems may be two to three times that cost. Annual recurrent costs are significant and usually exceed 20% of the capital cost of the system.
The CIS industry is subject to the same vagaries as other parts of the IT industry, including high turnover of personnel and frequent inability to deliver on promised functionality and timelines. CIS selection is best conducted as a formal tender process, and the evaluation of submissions is a complex task (Table 9.3). Availability and expense of on-site support during and following implementation are also critical factors.
Table 9.3 Clinical information systems (CIS) evaluation
Implementation planning should be detailed and requires a full-time project officer on site. A standard implementation needs 4–6 months prior to the ‘go live’ date with hospital-wide consultation, issue management and carefully scheduled staff training. It is desirable to have as many as possible of the interfaces and bedside devices linked to the CIS at the implementation date. This will maximise perceived benefits early and thereby encourage acceptance of the system. It should be implemented through the whole ICU as partial implementations are rarely successful.
Post-implementation review is essential to progress outstanding issues, which are usually prolific, and help establish the arrangements for the support and continued development of the system. A system management plan identifies the responsibility centres for management of the CIS components and clarifies requirements and expectations. A permanent on-site system management position is required for system maintenance, progressing outstanding issues and managing future upgrades and developments.
BENEFITS OF CIS: THE STATE OF THE ART
Basic CIS requirements are fulfilled by the majority of systems currently available:
Decision support systems have previously been disappointing but their further development offers substantial benefits.25,28 A legible and available record of previous and ongoing care does offer an improved level of decision support, albeit one that the general community would already expect and see as mandatory. Passive decision support with access to knowledge-based systems through CIS and hospital intranets, as well as resources such as pharmacopoeia, literature search engines and online texts and journals, is widely available. It is intuitive that these resources would improve the quality of clinical outcomes; but there is little evidence to support this.
Active decision support has not been generally available, including the flagging of drug allergies and interactions and the integration of relevant information, such as baseline renal function, recent urine output, last measured creatinine and required dose of aminoglycoside. Decision support systems to recommend antimicrobial prescribing, ventilatory therapy or haemodynamic measurement have been developed in dedicated centres of excellence, but are also not generally available nor necessarily able to be migrated successfully across boundaries of international practice. The provision of prompts has been shown to be effective for routine prophylaxis and care processes, supported by clinical pathways and guidelines.19,29 Increasing emphasis on decision support from safety and quality initiatives may be expected to accelerate developments.
CPOE is exemplified in electronic prescribing, but its benefits extend to other areas such as pathology and radiology orders and results viewing. There is good evidence that a reduction in ordering occurs through reduced duplication and timeliness and access to results.25,28 The availability of CPOE (computerised physician order entry) varies with the level of systems integration and compatibility with other legacy and proprietary computer systems. Standardised communications protocols (e.g. HL-7) are helpful but only provide similarities of electronic language. High-level interfaces require continued maintenance and development and therefore expenditure. Other solutions include seamless and simultaneous operation in multiple systems (Clinical Context Object Workgroup) or placing all data in a single repository for access by multiple applications.13
Clinical databases remain a significant challenge, whether at a local departmental, hospital, regional or national level. Although many products are purported to include data management and query solutions, those that are available ‘off the shelf’ may be quite rudimentary and their development may require additional expenditure and a major commitment from the clinical staff. Part of the problem is the need for clinicians to define prospectively what is expected of the system. This requires exhaustive definition of the questions that the system should be able to answer and therefore also specification of the detailed nature of the data and queries that will be required.
Accurate analysis of diagnoses and procedures requires that key information is entered correctly and consistently and that reliable and high-quality data capture is achieved. Data entry should be ‘once-only’, simple and robust, and should be easily performed as the clinical scenario unfolds. There is very limited agreement and standardisation between clinicians with respect to mandatory data fields, diagnostic criteria and classifications. Standardised reports are therefore difficult to develop in different clinical environments, let alone regions or countries. The eventual adoption of common international standards and classifications (e.g. SNOMED for diagnoses, National Library of Medicines for pharmaceuticals) would greatly facilitate solution design and querying. Other issues, including the speed of data access in huge data repositories, the development of unique patient/episode identifiers and privacy considerations, are still significant.
FUTURE DEVELOPMENTS
Over the next decade the EHR will provide the most significant and comprehensive improvement in the delivery of health care in developed nations. Central clinical repositories will probably initially hold sentinel data for consenting patients such as identifiers, past and present diagnoses, medications and allergies. More detailed data will be held in peripheral repositories where the challenge is ensuring appropriate accessibility and/or systems integration. The use of CIS with active decision support and computerised order entry will be an integral part of delivering and monitoring improved patient care. Despite requiring huge levels of investment, these developments are happening now and should include clinical involvement and leadership to realise and maximise their benefits.
1 Teich JM, Glaser JP, Beckley RF, et al. The Brigham integrated computing system (BICS): advanced clinical systems in an academic hospital environment. Int J Med Inform. 1999;54:197-208.
2 de Keizer NF, Stoutenbeek CP, Hanneman LA, et al. An evaluation of patient data management systems in Dutch intensive care. Intens Care Med. 1998;24:167-171.
3 Harrison JP, Palacio C. The role of clinical information systems in health care quality improvement. Health Care Manage (Frederick). 2006;25:206-212.
4 Metnitz PG, Lenz K. Patient data management systems in intensive care – the situation in Europe. Intens Care Med. 1995;21:703-715.
5 Urschitz M, Lorenz S, Unterasinger L, et al. Three years experience with a patient data management system at a neonatal intensive care unit. J Clin Monit Comput. 1998;14:119-125.
6 Fraenkel DJ. Clinical information systems in intensive care. Crit Care Resusc. 1999;1:179.
7 Ash JS, Bates DW. Factors and forces affecting EHR system adoption: report of a 2004 ACMI discussion. J Am Med Inform Assoc. 2005;12:8-12.
8 Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348:2526-2534.
9 Bates DW, Cohen M, Leape LL, et al. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001;8:299-308.
10 Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? JAMA. 2005;293:2384-2390.
11 Frisse ME. Comments on return on investment (ROI) as it applies to clinical systems. J Am Med Inform Assoc. 2006;13:365-367.
12 The Leapfrog Group Fact Sheet. Available online at http://www.leapfroggroup.org/about_us/leapfrog-factsheet Accessed 7 November 2006
13 Tackley R. Integrating anaesthesia and intensive care into the national care record. Br J Anaesth. 2006;97:69-76.
14 National Health Service. NHS Connecting for Health. Available online at http://www.connectingforhealth.nhs.uk/ Accessed 7 November 2006
15 Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med. 2004;141:938-945.
16 Hynes DM, Perrin RA, Rappaport S, et al. Informatics resources to support health care quality improvement in the Veterans Health Administration. J Am Med Inform Assoc. 2004;11:344-350.
17 United States Department of Veterans Affairs. VA VISTA Innovations Award. Available online at http://www.innovations.va.gov/innovations/ Accessed 7 November 2006
18 Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311-1316.
19 Kucher N, Koo S, Quiroz R, et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352:969-977.
20 Wang SJ, Middleton B, Prosser LA, et al. A cost benefit analysis of electronic medical records in primary care. Am J Med. 2003;114:397-403.
21 Kaushal R, Jha AK, Franz C, et al. Return on investment for a computerized physician order entry system. J Am Med Inform Assoc. 2006;13:261-266.
22 Health Connect. Available online at http://www.health.gov.au/internet/hconnect/publishing.nsf/Content/home Accessed 7 November 2006
23 Fraenkel DJ, Cowie M, Daley P. Quality benefits of an intensive care clinical information system. Crit Care Med. 2003;31:120-125.
24 Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice study I. N Engl J Med. 1991;24:370-376.
25 Teich JM, Osheroff JA, Pifer EA, et al. Clinical decision support in electronic prescribing: recommendations and an action plan: report of the joint clinical decision support workgroup. J Am Med Inform Assoc. 2005;12:365-376.
26 Han YY, Carcillo JA, Venkataraman ST, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;116:1506-1512.
27 Sittig DF, Ash JS, Zhang J, et al. Lessons from ‘Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system.’. Pediatrics. 2006;118:797-801.
28 Garg AX, Adhikari NK, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293:1223-1238.
29 Evans RS, Pestotnik SL, Classen DC, et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med. 1998;338:232-238.