CHAPTER 6 Clinical features, diagnosis and differential diagnosis
Incidence
Cataract is a common disease affecting more than 20 million people worldwide and a common cause of blindness. The prevalence increases with age. In the Beaver Dam Study, the relationship between age and incidence of cataracts was quadratic for nuclear cataract, cubic for cortical cataract, and linear for posterior subcapsular cataract (PSC)1. There are ethnic differences in the incidence of the types of cataract, with cortical cataract more common amongst those of African ancestry compared to those of European ancestry whilst nuclear and PSC are comparatively less common2.
Cataract types
There are three main types of cataract in the adult:
They may occur singly or in combination in a quarter of cases.
Cortical cataract
The cortical cataract is also called spoke cataract. These are wedge shaped opacities in both retroillumination and oblique illumination. They are triangular in shape with the apex pointing centrally. They are most commonly found in the inferonasal, then in the inferotemporal quadrant. Some have postulated that they are therefore the result of the greater exposure to sunlight, whilst twin studies have suggested that cortical cataract involves the action of dominant genes3. Their shape is due to the arrangement of the lens fibers inserting into the lens sutures. Cortical cataracts tend to start peripherally and therefore in the early stages are hidden by the iris and have little effect on vision. They are often associated with waterclefts4. These have been shown by scanning electron microscopy to be due to a separation along the suture line with globular components within it. The lens suture is not in itself a structure, but rather a zone of discontinuity within the lens where the tips of the expanded ends of the lens fibers meet. The watercleft therefore is best seen on retroillumination, and can be seen only with difficulty in oblique illumination. On slit illumination, they appear as optically empty spaces. As their refractive index is different from the surrounding fibers, they also cause confusing reflexes during retinoscopy.
Nuclear cataract
Nuclear cataract involves the lens nucleus only. It first presents as increased back scattering best seen on slit illumination. In some case, the nucleus appears very white, also called nuclear white scatter or opalescence. In many cases, the nucleus darkens and becomes brown; this is called nuclear brunescence. The increase in scattering is due to a series of non-enzymatic post-translational modifications of lens proteins. There is unfolding of the lens crystallins with formation of disulfide-linked aggregate formation. These scatter light leading to white nuclear scatter. The brown pigment is thought to be partly due to 3-hydroxy kynurenine. Scheimpflug-measured lens backscatter, an indirect measure of nuclear density, correlates with phacoemulsification time and energy. There is an exponential relationship between machine-measured effective phacoemulsification time and the degree of nuclear catatact (r2 = 0.48) and nuclear opalescence (r2 = 0.40)5.
Nuclear cataract is common after vitrectomy especially in the over-50-year-olds. It is thought to be the result of increased exposure to oxygen as the oxygen tension in the vitreous cavity next to the lens increases eight fold after vitrectomy6. It is of interest that use of multivitamins might have a protective effect in nuclear cataract but not other types7. There is an inverse association between high dietary lutein and zeaxanthine intake and prevalence of nuclear cataract8.
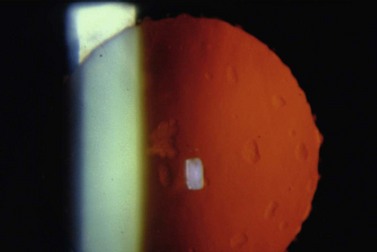
Nuclear cataracts have been shown to be commonly associated with retrodots (Fig 6.1).
Posterior subcapsular cataract
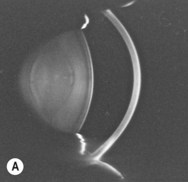
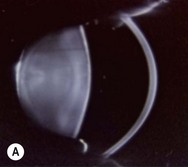
These are the least common of the cataracts. They are seen most readily by retroillumination. They are usually roughly circular lying in the posterior subcapsular zone. The anterior clear zone (ACZ) is reduced or absent. This zone is best seen in slit illumination and at maximum magnification and illumination. It is a thin clear zone of fibers measuring approximately 125 microns lying just beneath the anterior capsule (Fig. 6.2A,B.) With advancing posterior subcapsular cataract, the ACZ thins and eventually disappears (Fig. 6.3A,B). In diabetics, the ACZ can be larger than normal. Histological studies have shown that there is an equatorial lens bow where new fibers are being produced. In posterior subcapsular cataract (PSC), the normal lens bow is disturbed. Instead of clear fibers, aberrant lens material is produced and migrates to the posterior subcapsular region. In radiation cataract, from total body radiation for example, opacities can be seen streaming from the periphery to the posterior pole. This results in a PSC. The posterior subcapsular cataract may be associated with an anterior capsular component. However, this is not often seen clinically, but aberrant fibers can be identified in the anterior subcapsular region on histological section.
Should the cataractogenic insult be limited such as in renal transplantation or a short course of steroids, the posterior subcapsular cataract can recover with the clear new lens fibers being produced. These will be superficial to the posterior subcapsular cataract, which will then appear to sink into the cortex. There will be a gradual recovery in size of the ACZ. Examination of the ACZ can therefore be a guide to prognosis and allow prediction of whether the posterior subcapsular cataract will recover10.
Other types of acquired cataract
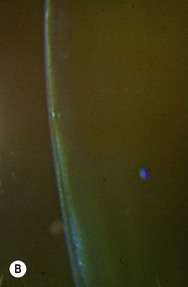
Fiber folds used to be called lamellar separation. They are best seen in focal illumination. They consist of a series of whitish branching lines (Fig. 6.4). In fact, electron microscopy has shown that they are the result of breaks in the lens fibers in the equatorial region (Fig. 6.5). This appears to release the tension on the lens fibers, which then bunch up into folds. They are associated with spoke cataracts. They are not due to separation of the lens lamellar and this term should therefore be abandoned11.
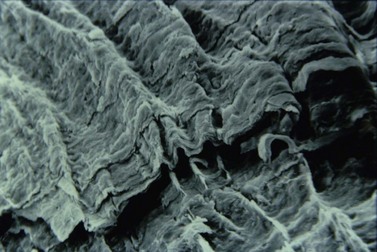
Fig. 6.5 SEM of fiber folds showing the extensive folding of the lens fibers.
Reproduced with permission from Professor G.F. Vrensen.
Vacuoles are round transparent spaces within the lens cortex. They show an unreversed light effect and are therefore of low refractive index in contradistinction to retrodots (Fig. 6.6). They can be transient.
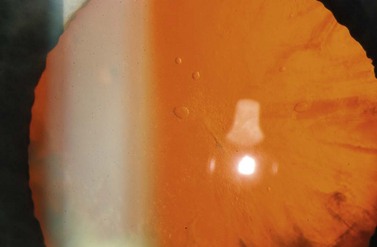
Fig. 6.6 Lens vacuoles seen in retroillumination. Note that there is no reversal of the background illumination in contrast to retrodots seen in Fig. 6.1.
Christmas tree cataracts can be unilateral or bilateral. They are needle like, highly reflective multicolored, and birefringent. Interestingly they cut across the lens fibers without causing opacification. It has been suggested that they consist of cystine, one of the least soluble amino acids, and on scanning electron microscopy consist of plate-like structures. They are commonly confused with the polychromatic cataract of myotonic dystrophy, which is made up of much smaller particles12.
Effect on visual acuity and function
There is an association between severity of cataract as classified by LOCS II grading and LogMAR visual acuity. Using multiple regression analysis, the correlation for cortical cataract is good (r2 = 0.65), and nuclear (r2 = 0.80), but less for PSC (r2 = 0.36)13.
Cataracts cause backscatter towards the observer and this is what is obvious at the slit lamp. However, it is forward scatter by the lens on the retina which causes image degradation and veiling luminance. There is no direct relationship between forward and back scatter. This explains why retrodots and waterclefts impair vision even though they are not readily seen by backscatter14. Cortical and especially PSC cause backscatter and the patient notices glare with incoming headlights at night.
Visual acuity is particularly affected in PSC compared to nuclear and cortical cataract. PSC impairs reading performance. Even though visual acuity is similar, PSC leads to greater visual impairment as measured by the VF-14 score15. Night and day glare estimated using Vistech MCT8000 are associated only with increasing severity of PSC16.
Nuclear cataract is associated with a myopic change so that some may suddenly find that they no longer need reading glasses. Subjects over the age of 55 with clear lenses who present a myopic change of 1 diopter over 4 years are very likely to develop a nuclear cataract, i.e. myopic change precedes onset of nuclear cataract and low grade myopia is not a risk factor for cataract17.
Early cataract causes reduction in contrast sensitivity at intermediate and high spatial frequencies and late cataract at all frequencies18. Higher order aberrations have been associated with loss of contrast sensitivity19. Coma (0.29 microns) is more common in cortical cataract, and spherical aberration in nuclear cataract (0.45 microns). Both induced a higher amount of tetrafoil20.
Waterclefts and cortical cataract produce monocular diplopia. Pin hole and accurate refraction will often reduce this effect. It has been shown that the combination of trefoil and spherical aberration can cause triplopia21.
Cataract classification systems
There are two main classification systems, the Oxford Clinical Cataract Classification System (OCCCS)22 and the Lens Opacity Classification System III (LOCSIII)23. OCCCS is a slit lamp-based system in which nuclear brunescence, white scatter, cortical, PSC, anterior clear zone, and focal dot opacities are graded by comparison with standard diagrams and Munsell color chips. There are equal interval steps between the grades. It has a high inter-observer reproducibility (kappa = +0.68) and intra-observer reproducibility (kappa = +0.55). LOCS uses standard photographs. There is a linear relationship between the grades for nuclear and PSC between the two systems but LOCSIII scores for cortical cataract need to be squared to achieve a linear relationship24.
1 Klein BE, Klein R, Lee KE, et al. Incidence of age-related cataract over a 15-year interval the Beaver Dam Eye Study. Ophthalmology. 2008;115(3):477-482.
2 Wong T, Hyman L. Population based studies in ophthalmology. Am J Ophthalmol. 2008;146:656-663.
3 Hammond CJ, Duncan DD, Snieder H, et al. The heritability of age-related cortical cataract: the twin eye study. Invest Ophthalmol Visual Sci. 2001;42(3):601-605.
4 Brown NP, Harris ML, Shun-Shin GA, et al. Is cortical spoke cataract due to lens fibre breaks? The relationship between fibre folds, fibre breaks, waterclefts and spoke cataract. Eye (Lond). 1993;7(Part 5):672-679.
5 Davison JA, Chylack LT. Clinical application of the lens opacities classification system III in the performance of phacoemulsification. J Cataract Refract Surg. 2003;29(1):138-145.
6 Holekamp NM, Shui YB, et al. Vitrectomy surgery increases oxygen exposure to the lens: A possible mechanism for nuclear cataract formation. Am J Ophthalmol. 2005;139(2):302-310.
7 Maraini G, Sperduto RD, Ferris F, et al. A randomized, double-masked, placebo-controlled clinical trial of multivitamin supplementation for age-related lens opacities. Clinical trial of nutritional supplements and age-related cataract report no. 3. Ophthalmology. 2008;115(4):599-607.
8 Vu HT, Robman L, Hodge A, et al. Lutein and zeaxanthin and the risk of cataract: the Melbourne visual impairment project. Invest Ophthalmol Visual Sci. 2006;47(9):3783-3786.
9 Vrensen GF, Willekens B, De Jong PT, et al. Heterogeneity in ultrastructure and elemental composition of perinuclear lens retrodots. Invest Ophthalmol Vis Sci. 1994;35(1):199-206.
10 Shun-Shin GA, Ratcliffe P, Bron AJ, et al. The lens after renal transplantation. Br J Ophthalmol. 1990;74:267-271.
11 Brown NA, Vrensen G, Shun-Shin GA, et al. Lamellar separation in the human lens: the case for fibre folds. A combined in vivo and electron microscopy study. Eye (Lond). 1989;3(Part 5):597-605.
12 Shun-Shin GA, Vrensen GF, Brown NP, et al. Morphologic characteristics and chemical composition of Christmas tree cataract. Invest Ophthalmol Vis Sci. 1993;34(13):3489-3496.
13 Maraini G, Rosmini F, Graziosi P, et al. Italian American Cataract Study Group. Influence of type and severity of pure forms of age-related cataract on visual acuity and contrast sensitivity. Invest Ophthalmol Visual Sci. 1994;35:262-267.
14 Frost NA, Sparrow JM, Moore L. Associations of human crystalline lens retrodots and waterclefts with visual impairment: an observational study. Invest Ophthalmol Visual Sci. 2002;43(7):2105-2109.
15 Stifter E, Sacu S, Thaler A, et al. Contrast acuity in cataracts of different morphology and association to self-reported visual function. Invest Ophthalmol Visual Sci. 2006;47(12):5412-5422.
16 Lasa MS, Datiles MB, Podgor MJ, et al. Contrast and glare sensitivity tests. Association with the type and severity of the cataract. Ophthalmology. 1992;99:1045-1049.
17 Brown NA, Hill AR. Cataract: the relation between myopia and cataract morphology. Br J Ophthalmol. 1987;71:405-414.
18 Chua BE, Mitchell P, Cumming RG. Effects of cataract type and location on visual function: The Blue Mountains Eye Study. Eye. 2004;18:765-772.
19 Kuroda T, Fujikado T, Maeda N, et al. Wavefront analysis in eyes with nuclear or cortical cataract. Am J Ophthalmol. 2002;134(1):1-9.
20 Rocha KM, Nose W, Bottos K, et al. Higher-order aberrations of age-related cataract. J Cataract Refract Surg. 2007;33(8):1442-1446.
21 Fujikado T, Kuroda T, Maeda N, et al. Wavefront analysis of an eye with monocular triplopia and nuclear cataract. Am J Ophthalmol. 2004;137(2):361-363.
22 Sparrow JM, Ayliffe W, Bron AJ, et al. Inter-observer and intra-observer variability of the Oxford clinical cataract classification and grading system. Int Ophthalmol. 1988;11:151-157.
23 Chylack LTJr, Wolfe JK, Singer DM, et al. The Longitudinal Study of Cataract Study Group. The Lens Opacities Classification System III. Arch Ophthalmol. 1993;111:831-836.
24 Hall AB, Thompson JR, Deane JS, et al. LOCS III versus the Oxford Clinical Cataract Classification and Grading System for the assessment of nuclear, cortical and posterior subcapsular cataract. Ophthal Epidemiol. 1997;4:179-194.