13
Clinical Approach to Regional Dermatoses
Dermatitis of the Hands and Feet
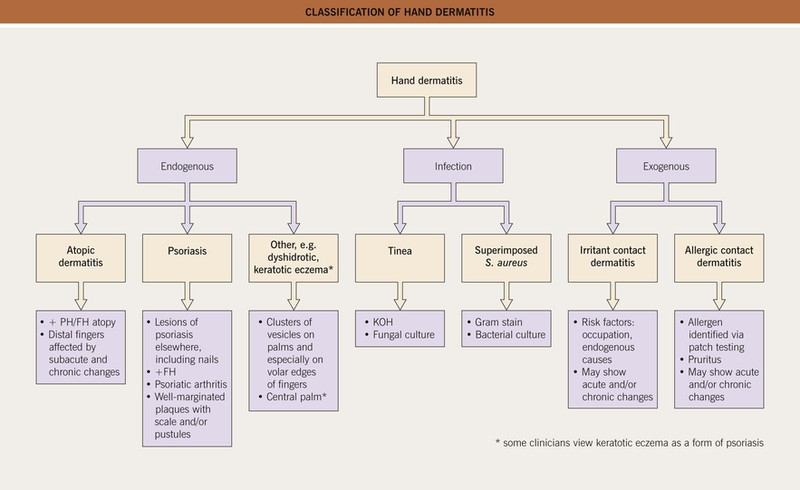
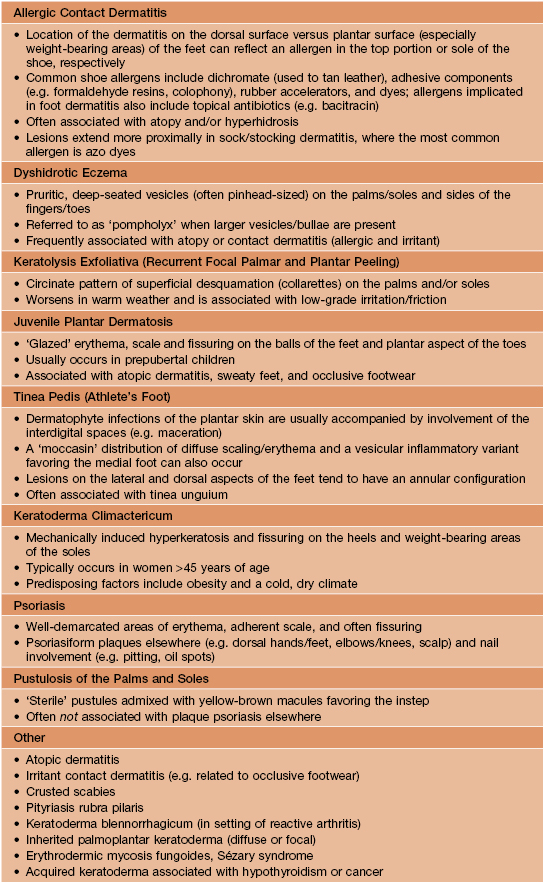
• An approach to the classification of hand dermatitis is presented in Fig. 13.1, and the differential diagnosis of foot dermatitis is summarized in Table 13.1.
Intertriginous Dermatitis
• The differential diagnosis of dermatitis in the major skin folds is presented in Fig. 13.2.
Table 13.2
Symmetrical drug-related intertriginous and flexural exanthema (SDRIFE): clinical criteria.
This entity is also referred to as drug-induced intertrigo, flexural drug eruption, and baboon syndrome. The latter term is also used for a form of systemic contact dermatitis.
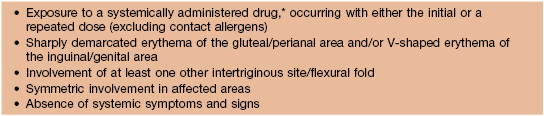
* Not a chemotherapeutic agent, so distinct from toxic erythema of chemotherapy.
Adapted from Häusermann P, Harr TH, Bircher AJ. Baboon syndrome resulting from systemic drugs: Is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Dermatitis 2004;51:297–310.
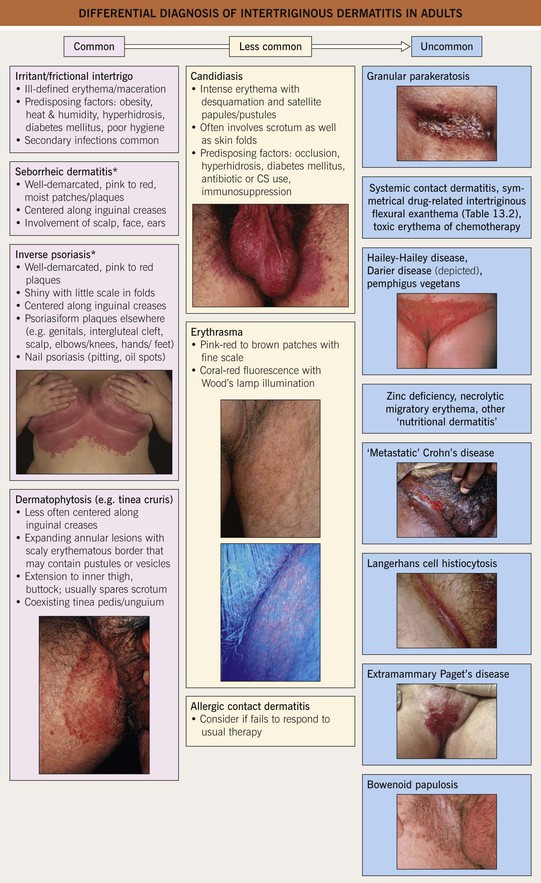
Fig. 13.2 Differential diagnosis of intertriginous dermatitis in adults. Individual patients often have multiple disorders superimposed upon one another. Bullous impetigo and streptococcal intertrigo are considerably more common in children than adults (see Fig. 13.4). *The term ‘sebopsoriasis’ may be used when features of both seborrheic dermatitis and psoriasis are present. Insets: Courtesy, Eugene Mirrer, MD; Louis Fragola, Jr., MD; David Mehregan, MD and Robert Hartman, MD.
• Low-potency topical CS are often effective for dermatoses in these areas, and prolonged use of more potent agents (including antifungal combination products; see below) has increased potential to result in side effects such as cutaneous atrophy (Fig. 13.3).
Diaper Dermatitis
• Develops in >50% of infants and has a variety of causes (Fig. 13.4).
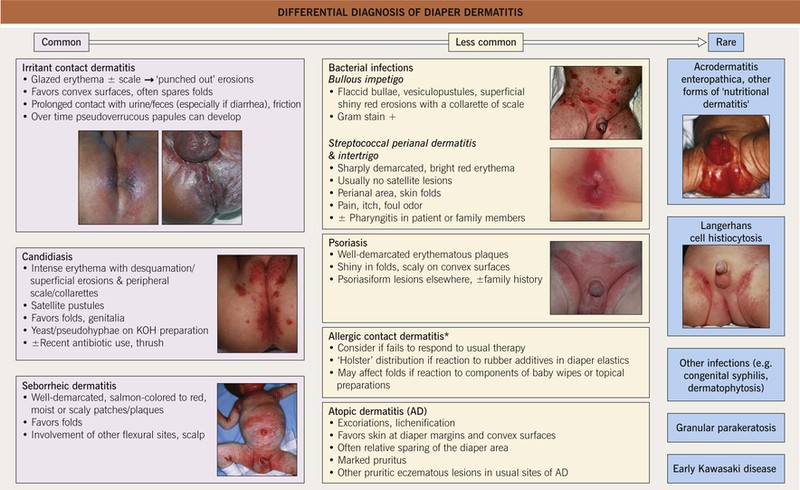
Fig. 13.4 Differential diagnosis of diaper dermatitis. Patients often have a combination of disorders, one superimposed upon another. Discrete papules or nodules can be seen in scabies, granuloma gluteale infantum, and perianal pseudoverrucous papules, whereas congenital syphilis may present with erosions or even ulcerations. *Potential allergens include sorbitan sesquioleate (an emulsifier in diaper balms), fragrances, disperse dyes, rubber additives (e.g. mercaptobenzothiazole), preservatives in baby wipes, and diaper components. Insets: Courtesy, Robert Hartman, MD, and Julie V. Schaffer, MD.
Cheilitis
• The differential diagnosis of cheilitis and clues to determining the etiology are outlined in Fig. 13.5.
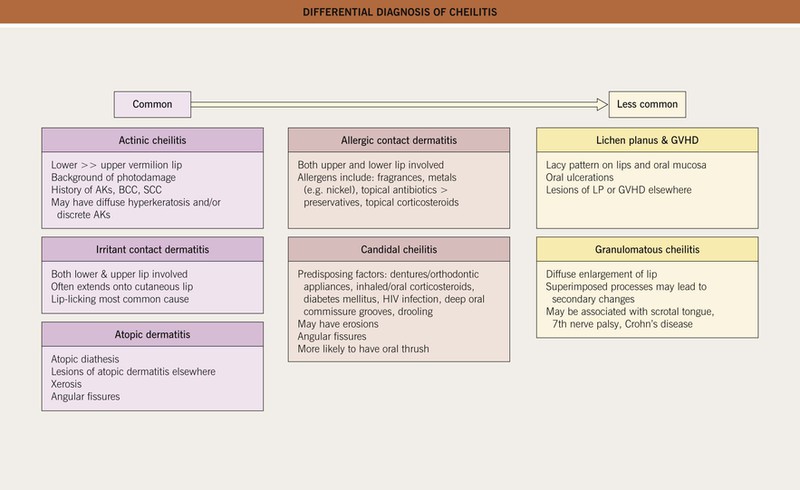
Fig. 13.5 Differential diagnosis of cheilitis. A combination of etiologies is often present, e.g. atopic dermatitis plus irritant contact dermatitis. Other uncommon causes include cheilitis glandularis, actinic prurigo, lichen sclerosus, and nutritional deficiencies. AKs, actinic keratoses; LP, lichen planus. Courtesy, Jean L. Bolognia, MD.
Eyelid Dermatitis
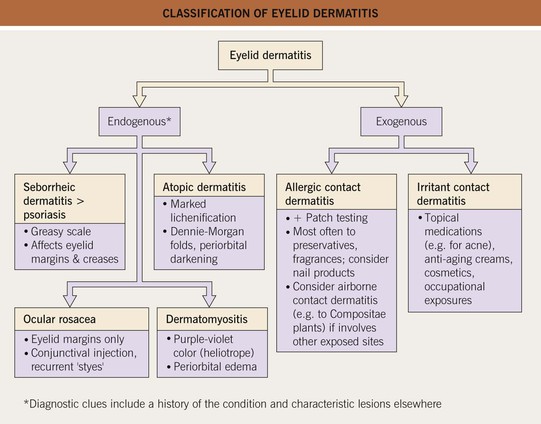
• An approach to the classification of eyelid dermatitis is presented in Fig. 13.6.
For further information see Chs. 13 and 15. From Dermatology, Third Edition.