CHAPTER 395 Classification of Spinal Arteriovenous Lesions
Arteriovenous Fistulas and Arteriovenous Malformations
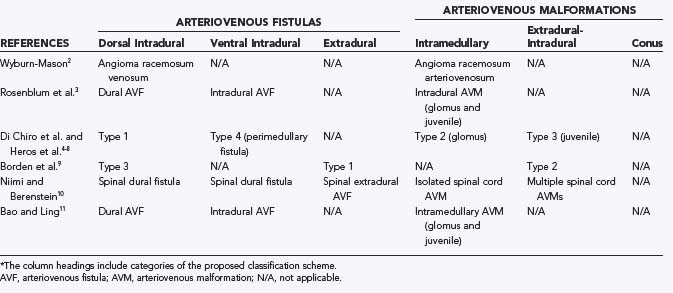
Spinal arteriovenous lesions are a collection of disparate and diverse entities, and our understanding of their pathophysiology has evolved significantly over the past century. Recently, significant microsurgical and endovascular advances have been made in the treatment of spinal arteriovenous malformations (AVMs). To select an effective treatment strategy, surgeons must first characterize a lesion accurately. In this chapter we propose a classification system derived from the senior author’s (R.F.S.) experience1 that is based on specific anatomic and pathophysiologic characteristics of the lesions. The lesions are divided into arteriovenous fistulas (AVFs) and AVMs (Table 395-1).2–11 AVFs are subdivided anatomically into extradural and intradural. Intradural AVFs are further divided into dorsal and ventral types according to their location. Based on size and the number of feeding branches, ventral dural AVFs are further divided into types A, B, and C. AVMs include extradural-intradural, intramedullary, and conus lesions.
TABLE 395-1 Proposed Classification of Spinal Arteriovenous Lesions and Comparison with Previous Nomenclature*
Historical Perspective and Previous Classifications
Spinal AVMs were first described by Gaupp in 1888.12 Twenty-three years later, Krause described the first surgically treated spinal dural fistula.13 In 1931, 5 years after its original clinical description, Foix-Alajouanine syndrome (subacute necrotic myelopathy) was linked to acute thrombosis of pathologic spinal AVM vessels.14–16
In 1943, Wyburn-Mason analyzed 110 patients with spinal AVMs.2 In his classic monograph, he recognized two main types of spinal vascular lesions: venous angioma (angioma racemosum venosum) and arteriovenous angioma (angioma racemosum arteriovenosum). The venous type consisted of a mass of turgid pial veins, usually located in the posterior aspect and below the midthoracic portion of the spinal cord. He described it microscopically as thick-walled pial vessels with marked “proliferation of intramedullary capillaries, precapillaries and venules.” The arteriovenous type was described as a fistulous capillary bed, most commonly found in the cervical or lumbar enlargement and often recognized early in life. Microscopically, there were many vessels of different size and structures, some resembling arteries and others veins.2
As spinal angiographic techniques have improved,4,5,17–19 authors have moved from descriptive pathologic analysis toward anatomically based classifications for spinal AVMs. Di Chiro and other investigators proposed the most common recent classification scheme in which spinal AVMs were divided into three types.4,5–8 Type I lesions are dural AVFs in which a dural branch from a radicular artery forms an abnormal communication with the dural veins at the nerve root sleeve. Type II lesions are glomus or intramedullary lesions. Type III lesions are juvenile or metameric AVMs associated with both extradural and intradural extension of the spinal AVM. Subsequently, Djindian and associates proposed a new category of ventral perimedullary fistula supplied by the anterior spinal artery (ASA).7 Heros and colleagues further characterized this type of lesion as a type IV spinal AVM.6
Borden and coworkers described a three-point anatomic classification of spinal dural AVFs and used the term dural arteriovenous fistulous malformation (AVFM).9 Type I AVFMs involve Batson’s epidural venous plexus. Type II lesions drain into both the epidural and perimedullary venous plexus. Type III AVFMs are supplied by meningeal branches of a radicular artery, which drain into the coronal venous plexus.4
Niimi and Berenstein divided vascular lesions of the spine into spinal vascular lesions and spinal cord vascular lesions.10 They subdivided spinal vascular lesions into dural and extradural fistulas. Spinal cord vascular lesions were referred to as spinal cord vascular malformations, of which there are two types: isolated, which includes AVMs and AVFs, and multiple, which includes metameric and nonmetameric forms.
Bao and Ling classified spinal cord vascular lesions as intramedullary AVMs, intradural AVFs, dural AVFs, paravertebral AVMs, and Cobb’s syndrome.11 Intramedullary lesions include glomus and juvenile forms. Based on their size and degree of blood flow, intradural AVFs were subdivided into types I, II, and III. Paravertebral AVMs involve the paravertebral muscles and the paravertebral and epidural space. Cobb’s syndrome involves multiple structures within the same metamere.
Rosenblum and coworkers described two major types of spinal AVMs in 81 patients based on the location of the vascular nidus: dural versus intradural.3 Intradural AVMs were divided into intramedullary and dural AVFs. Intramedullary lesions were further subclassified into glomus (compact) and juvenile (diffuse) AVMs. Dural AVFs were supplied by a dural artery, with fistulous drainage into spinal veins, at least partially within the cord or pia. Intramedullary lesions were supplied by medullary arteries, and the arteriovenous shunt was located partially in the spinal cord or pia mater. Dural AVFs were supplied by a radicular branch along the dural nerve root sleeve that drained via an AVF into the coronal venous plexus. This classification system included no description of extradural-intradural or conus AVMs.
As detailed earlier, the previous nomenclature used to describe spinal vascular malformations was purely descriptive and based on incomplete understanding of the angioarchitecture and pathophysiology of these lesions. Our system reclassifies previously described entities according to the improved understanding of the anatomic location and pathophysiology of each lesion (see Table 395-1).20,21 Accurate characterization of these lesions allows correct diagnosis of them and optimization of treatment.
Finally, we believe that spinal vascular malformations are so complex that some lesions will defy any proposed classification system. As lesions that do not fit the current scheme are better defined, the classification system must be updated to include these malformations. For this reason, we added the separate category of conus medullaris AVMs. In his vast experience treating spinal vascular malformations, R.F.S. has encountered these lesions several times. Because their specific characteristics fit no existing category, a new one was created.1,22 By recognizing conus AVMs, our classification system is the first to include all currently recognized spinal vascular malformations and fistulas.
Proposed Classification System
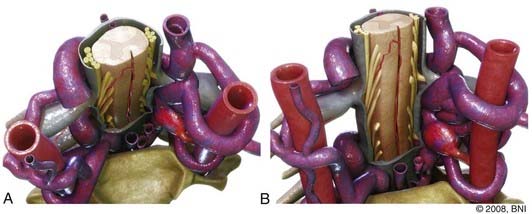
Extradural Arteriovenous Fistulas
Extradural AVFs (Fig. 395-1) are extremely uncommon. They represent a direct connection between a branch of a radicular artery and the epidural venous plexus, which leads to the development of an extradural high-flow AVF. These fistulas are usually characterized by significant engorgement of the epidural venous complex, which leads to a mass effect on the nerve roots or the spinal cord, or on both. Venous congestion of the spinal cord can also cause myelopathic symptoms. In addition, shunting of large amounts of arterial blood into the venous system can steal blood flow from the spinal cord with resultant ischemia and worsening myelopathy.10,23–27
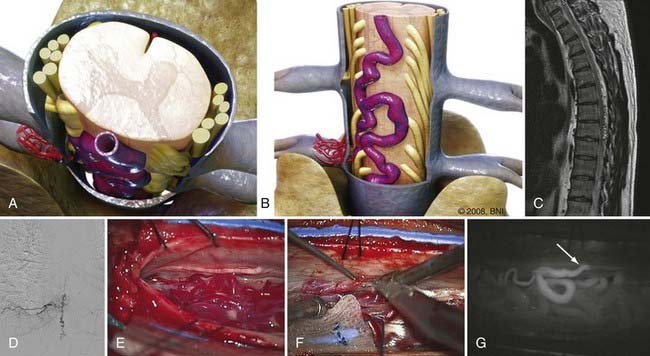
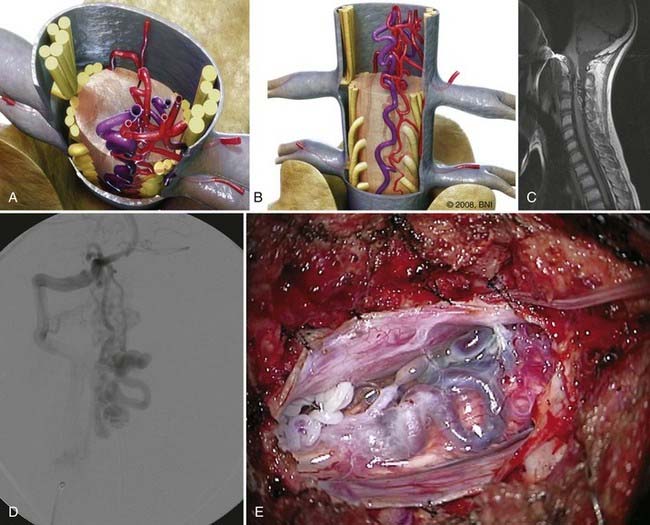
Intradural Dorsal Arteriovenous Fistulas
Intradural dorsal AVFs are the most common type of spinal AVF and usually occur in the thoracic region. Intradural dorsal AVFs (Fig. 395-2), which correlate with type I dural AVFs, are composed of a direct connection between a radicular feeding artery and the coronal venous plexus. A glomerular network of tiny branches of the radicular artery coalesces at the fistulous site, which is in the dural sleeve of the nerve root. Arterialization of the coronal venous plexus leads to myelopathic venous congestion and subsequent myelopathy.
Intradural Ventral Arteriovenous Fistulas
Intradural ventral AVFs (Fig. 395-3) consist of an abnormal connection between the ASA and the coronal venous plexus. They are midline lesions located in the ventral subarachnoid space. Intradural ventral AVFs have been divided into three types based on size.28 Type A fistulas are small shunts with slow blood flow and a moderate amount of venous hypertension. Types B and C have increasingly larger shunts, which often lead to a markedly distended coronal venous plexus. As flow through the fistula increases, progressive vascular steal and spinal cord compression take place and lead to worsening myelopathy.
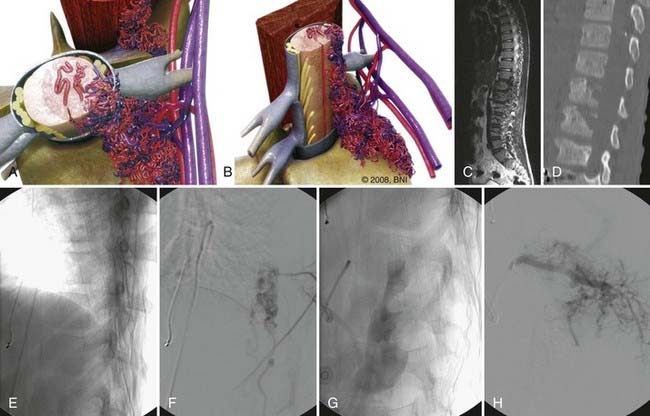
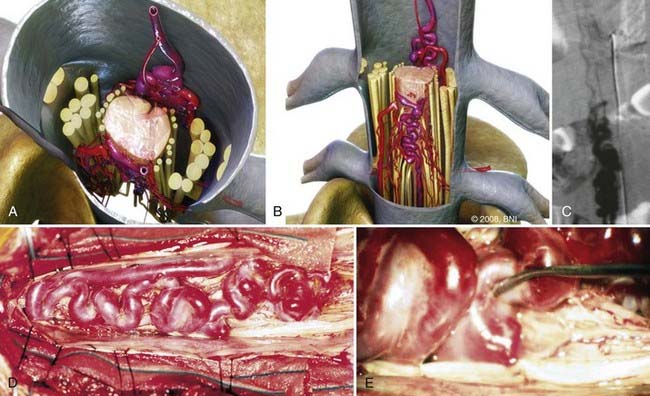
Extradural-Intradural Arteriovenous Malformations
Extradural-intradural AVMs (Fig. 395-4) are rare. In the past they have been called juvenile, metameric, or type III AVMs. As their old name implies, they tend to be most common in children but can also occur in adults. Typically, they respect no tissue boundaries and can involve bone, muscle, skin, spinal canal, spinal cord, and nerve roots along an entire spinal level. Such complete involvement of the AVM along an entire somitic level has been termed Cobb’s syndrome.
Intramedullary Arteriovenous Malformations
Much like their intracranial counterparts, intramedullary AVMs are located in the substance of the spinal cord. These lesions can be supplied by single or multiple branches of the ASA and posterior spinal artery (PSA). They are classified as compact or diffuse (Figs. 395-5 and 395-6), depending on the tightness of the nidus. These lesions are usually low-resistance, high-pressure, and high–blood flow vascular malformations. Associated nidal aneurysms are common.29
Intramedullary spinal cord AVMs usually become symptomatic with acute myelopathy from hemorrhage or compression. Vascular steal can lead to progressive myelopathy.30
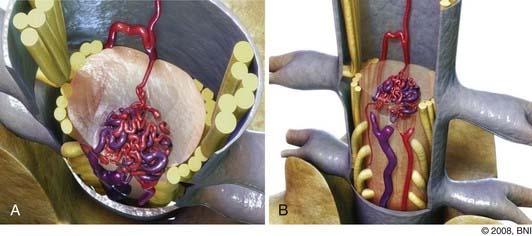
Conus Medullaris Arteriovenous Malformations
Conus medullaris AVMs (Fig. 395-7) are separate entities because they fit none of the aforementioned categories.1 These lesions typically exhibit complex nidal angioarchitecture with multiple direct shunts from the ASA, PSA, and radicular arteries and drainage into both the anterior and posterior venous plexuses. In addition to the multiple AVFs, these AVMs also usually contain a true AVM nidus. The nidus is of the glomus type and is typically extramedullary and pial based, but it can also have an intramedullary component.
Anson J, Spetzler R. Classification of spinal arteriovenous malformations and implications for treament. BNI Q. 1992;8:5-8.
Arnaud O, Bille F, Pouget J, et al. Epidural arteriovenous fistula with perimedullary venous drainage: case report. Neuroradiology. 1994;36:490-491.
Baker HLJr, Love JG, Layton DDJr. Angiographic and surgical aspects of spinal cord vascular anomalies. Radiology. 1967;88:1078-1085.
Bao YH, Ling F. Classification and therapeutic modalities of spinal vascular malformations in 80 patients. Neurosurgery. 1997;40:75-81.
Barrow DL. Spinal cord vascular lesions. J Neurosurg. 2002;96:143-144.
Biondi A, Merland JJ, Hodes JE, et al. Aneurysms of spinal arteries associated with intramedullary arteriovenous malformations. I. Angiographic and clinical aspects. AJNR Am J Neuroradiol. 1992;13:913-922.
Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995;82:166-179.
Di Chiro G, Doppman J, Ommaya A. Radiology of the spinal cord arteriovenous malformations. Prog Neurol Surg. 1971;4:329-354.
Di Chiro G, Doppman J, Ommaya AK. Selective arteriography of arteriovenous aneurysms of spinal cord. Radiology. 1967;88:1065-1077.
Djindjian M, Djindjian R, Hurth M, et al. Steal phenomena in spinal arteriovenous malformations. J Neuroradiol. 1978;5:187-201.
Djindjian M, Djindjian R, Rey A, et al. Intradural extramedullary spinal arterio-venous malformations fed by the anterior spinal artery. Surg Neurol. 1977;8:85-93.
Doppman J, Di Chiro G, Ommaya AK. Selective Arteriography of the Spinal Cord. St. Louis: CV Mosby; 1969.
Foix C, Alajounanine T. La myélite central angiohypertrophique évolution progressive: paraplégie amyotrophique lentement ascendan d’abord spasmodique, puis flasque. Rev Neurol. 1926;2:1-42.
Graziani N, Bouillot P, Figarella-Branger D, et al. Cavernous angiomas and arteriovenous malformations of the spinal epidural space: report of 11 cases. Neurosurgery. 1994;35:856-863.
Guapp J. Hamorrhoiden der pia mater spinalis im gebiet des lendenmarks. Beitr Pathol. 1888;2:516.
Heier LA, Lee BC. A dural spinal arteriovenous malformation with epidural venous drainage: a case report. AJNR Am J Neuroradiol. 1987;8:561-563.
Heros RC, Debrun GM, Ojemann RG, et al. Direct spinal arteriovenous fistula: a new type of spinal AVM. Case report. J Neurosurg. 1986;64:134-139.
Krause F. Chirurgie des Gehirns und Ruckenmarks nach eigenen Erfarungen. Berlin: Urban & Schwarzenberg; 1911.
Lasjaunias P. Spinal cord vascular lesions. J Neurosurg. 2003;98:117-119.
Lhermitte J, Fribourg-Blanc J, Kyriaco N. La gliose angéio-hypertrophique de la moelle épinière (myélite nécrotique de Foix-Alajouanine). Rev Neurol. 1931;2:37-53.
Malis L. Arteriovenous malformations of the spinal cord. In: Youmans J, editor. Neurological Surgery: A Comprehensive Reference Guide to the Diagnosis and Management of Neurosurgical Problems. Philadelphia: WB Saunders; 1982:1850-1874.
Miyagi Y, Miyazono M, Kamikaseda K. Spinal epidural vascular malformation presenting in association with a spontaneously resolved acute epidural hematoma. Case report. J Neurosurg. 1998;88:909-911.
Niimi Y, Berenstein A. Endovascular treatment of spinal vascular malformations. Neurosurg Clin N Am. 1999;10:47-71.
Ommaya AK. Spinal arteriovenous malformations. In: Wilkins R, Rengachary S, editors. Neurosurgery. New York: McGraw-Hill; 1985:1495-1499.
Pia HW, Vogelsang H. [Diagnosis and therapy of spinal angioma.]. Dtsch Z Nervenheilkd. 1965;187:74-96.
Riina H, Lemole G, Kim L, et al. Spinal arteriovenous malformations. In: Mohr J, Choi D, Grotta J, et al, editors. Stroke: Pathophysiology, Diagnosis, and Management. Philadelphia: Churchill Livingstone; 2004:1417-1422.
Rosenblum B, Oldfield EH, Doppman JL, et al. Spinal arteriovenous malformations: a comparison of dural arteriovenous fistulas and intradural AVM’s in 81 patients. J Neurosurg. 1987;67:795-802.
Scully R, Mark E, McNeely W, et al. Case records of the Massachusetts General Hospital. N Engl J Med. 1987;317:225-235.
Spetzler RF, Detwiler PW, Riina HA, et al. Modified classification of spinal cord vascular lesions. J Neurosurg. 2002;96:145-156.
Wyburn-Mason R. The Vascular Abnormalities and Tumors of the Spinal Cord and Its Membranes. London: H. Klimpton; 1943.
1 Spetzler RF, Detwiler PW, Riina HA, et al. Modified classification of spinal cord vascular lesions. J Neurosurg. 2002;96:145-156.
2 Wyburn-Mason R. The Vascular Abnormalities and Tumors of the Spinal Cord and Its Membranes. London: H. Klimpton; 1943.
3 Rosenblum B, Oldfield EH, Doppman JL, et al. Spinal arteriovenous malformations: a comparison of dural arteriovenous fistulas and intradural AVM’s in 81 patients. J Neurosurg. 1987;67:795-802.
4 Di Chiro G, Doppman J, Ommaya A. Radiology of the spinal cord arteriovenous malformations. Prog Neurol Surg. 1971;4:329-354.
5 Doppman J, Di Chiro G, Ommaya AK. Selective Arteriography of the Spinal Cord. St. Louis: CV Mosby; 1969.
6 Heros RC, Debrun GM, Ojemann RG, et al. Direct spinal arteriovenous fistula: a new type of spinal AVM. Case report. J Neurosurg. 1986;64:134-139.
7 Malis L. Arteriovenous malformations of the spinal cord. In: Youmans J, editor. Neurological Surgery: A Comprehensive Reference Guide to the Diagnosis and Management of Neurosurgical Problems. Philadelphia: WB Saunders; 1982:1850-1874.
8 Ommaya AK. Spinal arteriovenous malformations. In: Wilkins R, Rengachary S, editors. Neurosurgery. New York: McGraw-Hill; 1985:1495-1499.
9 Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995;82:166-179.
10 Niimi Y, Berenstein A. Endovascular treatment of spinal vascular malformations. Neurosurg Clin N Am. 1999;10:47-71.
11 Bao YH, Ling F. Classification and therapeutic modalities of spinal vascular malformations in 80 patients. Neurosurgery. 1997;40:75-81.
12 Guapp J. Hamorrhoiden der pia mater spinalis im gebiet des lendenmarks. Beitr Pathol. 1888;2:516.
13 Krause F. Chirurgie des Gehirns und Ruckenmarks nach eigenen Erfarungen. Berlin: Urban & Schwarzenberg; 1911.
14 Foix C, Alajouanine T. La myélite central angiohypertrophique évolution progressive: Paraplégie amyotrophique lentement ascendan d’abord spasmodique, puis flasque. Rev Neurol. 1926;2:1-42.
15 Lhermitte J, Fribourg-Blanc J, Kyriaco N. La gliose angéio-hypertrophique de la moelle épinière (myélite nécrotique de Foix-Alajouanine). Rev Neurol. 1931;2:37-53.
16 Pia HW, Vogelsang H. [Diagnosis and therapy of spinal angioma.]. Dtsch Z Nervenheilkd. 1965;187:74-96.
17 Baker HLJr, Love JG, Layton DDJr. Angiographic and surgical aspects of spinal cord vascular anomalies. Radiology. 1967;88:1078-1085.
18 Di Chiro G, Doppman J, Ommaya AK. Selective arteriography of arteriovenous aneurysms of spinal cord. Radiology. 1967;88:1065-1077.
19 Djindjian M, Djindjian R, Rey A, et al. Intradural extramedullary spinal arterio-venous malformations fed by the anterior spinal artery. Surg Neurol. 1977;8:85-93.
20 Barrow DL. Spinal cord vascular lesions. J Neurosurg. 2002;96:143-144.
21 Lasjaunias P. Spinal cord vascular lesions. J Neurosurg. 2003;98:117-119.
22 Riina H, Lemole G, Kim L, et al. Spinal arteriovenous malformations. In: Mohr J, Choi D, Grotta J, et al, editors. Stroke: Pathophysiology, Diagnosis, and Management. Philadelphia: Churchill Livingstone; 2004:1417-1422.
23 Arnaud O, Bille F, Pouget J, et al. Epidural arteriovenous fistula with perimedullary venous drainage: case report. Neuroradiology. 1994;36:490-491.
24 Graziani N, Bouillot P, Figarella-Branger D, et al. Cavernous angiomas and arteriovenous malformations of the spinal epidural space: report of 11 cases. Neurosurgery. 1994;35:856-863.
25 Heier LA, Lee BC. A dural spinal arteriovenous malformation with epidural venous drainage: a case report. AJNR Am J Neuroradiol. 1987;8:561-563.
26 Miyagi Y, Miyazono M, Kamikaseda K. Spinal epidural vascular malformation presenting in association with a spontaneously resolved acute epidural hematoma. Case report. J Neurosurg. 1998;88:909-911.
27 Scully R, Mark E, McNeely W, et al. Case records of the Massachusetts General Hospital. N Engl J Med. 1987;317:225-235.
28 Anson J, Spetzler R. Classification of spinal arteriovenous malformations and implications for treament. BNI Q. 1992;8:5-8.
29 Biondi A, Merland JJ, Hodes JE, et al. Aneurysms of spinal arteries associated with intramedullary arteriovenous malformations. I. Angiographic and clinical aspects. AJNR Am J Neuroradiol. 1992;13:913-922.
30 Djindjian M, Djindjian R, Hurth M, et al. Steal phenomena in spinal arteriovenous malformations. J Neuroradiol. 1978;5:187-201.