Chapter 2 Characteristics, classification and incidence of disease
WHAT IS DISEASE?
A disease is a condition in which the presence of an abnormality of the body causes a loss of normal health (dis-ease). The mere presence of an abnormality is insufficient to imply the presence of disease unless it is accompanied by ill health, although it may denote an early stage in the development of a disease. The word disease is, therefore, synonymous with ill health and illness.
Each separately named disease is characterised by a distinct set of features (cause, signs and symptoms, morphological and functional changes, etc.). Many diseases share common features and thereby are grouped together in disease classification systems.
The abnormalities causing diseases may be structural or functional, or both. In many instances the abnormalities are obvious and well characterised (e.g. a tumour); in other instances the patient may be profoundly unwell but the nature of the abnormality is less well defined (e.g. depressive illness).
Limits of normality
Normal is impossible to define as a single discrete state for any biological characteristic. In addition to differences between individuals, the human body changes naturally during fetal development, childhood, puberty, pregnancy (gender permitting), ageing, etc. Therefore, ‘normal’ means the most frequent state in a population defined by age distribution, gender, etc.
Most quantifiable biological characteristics are normally distributed, in statistical terms, about an average value. There are no constant numbers that can be used to define a normal height, weight, serum sodium concentration, etc. Normality, when quantifiable, is expressed as a normal range, usually encompassed by two standard deviations (for a ‘normally’ distributed feature) either side of the mean (Ch. 4). The probability that a measurable characteristic is abnormal increases the nearer it is to the limits of the normal range, but a value lying outside the normal range is not necessarily indicative of abnormality—it is just very probably abnormal.
A distinction must also be drawn between what is usual and what is normal. It is usual to find atheroma (Ch. 13) in an elderly individual—but is it normal? In contrast, atheroma in a teenager is so unusual that it would be regarded as abnormal and worthy of further investigation.
Responses to the environment
The natural environment of any species contains potentially injurious agents to which the individual or species must either adapt or succumb.
Adaptation
Adaptation of the individual to an adverse environment is well illustrated by the following examples. Healthy mountaineers ascending rapidly to the rarefied atmosphere at high altitudes often develop ‘mountain sickness’; they recover by a process of adaptation (increased haemoglobin, etc.), but failure to do so can result in death from heart failure. Fair-skinned people get sunburnt from excessive exposure to ultraviolet light from the sun; some adapt by developing a protective tan, but untanned individuals run a higher risk of skin cancer if they persist in unprotected exposure to the sun for long periods. Environmental micro-organisms are a common cause of disease; those individuals who develop specific defences against them (e.g. antibodies) can resist the infection, but those who fail to adapt may succumb.
Disease: failure of adaptation
Susceptibility of a species to injurious environmental factors results in either its extinction or, over a long period, the favoured selection of a new strain of the species better adapted to withstand such factors. However, this holds true only if the injury manifests itself in the early years of life, thus thwarting propagation of the disease susceptibility by reproduction. If the injury manifests only in later life, or if a lifetime of exposure to the injurious agent is necessary to produce the pathological changes, then the agent produces no evolutionary pressure for change.
An arguable interpretation of disease is that it represents a set of abnormal bodily responses to agents for which, as yet, the human species has little or no tolerance.
Darwinian medicine
The relatively new science of Darwinian medicine is based on the belief that diseases not only have proximate causes and mechanisms (e.g. viruses, bacteria, mutations) but also have evolutionary causes. Darwinian medicine focuses on the latter aspect and, while it may not yield cures for many serious diseases, it can help us to understand their current prevalence. Darwinian medicine is also rooted in the belief that natural selection favours reproductive success rather than health or life-span.
In Why we get sick: the new science of Darwinian medicine, Randolph Nesse, an evolutionary biologist, and George Williams, a psychiatrist, explain the application of evolutionary ideas to medicine with these examples:
Ageing and adaptation
One of the main features of ageing is progressive inability of the individual to deal with new or worsening environmental threats (Ch. 12). This is exemplified by the gradual impairment of immune responses, resulting in:
Disease predisposition as an adaptive advantage
Paradoxically, a disease or disease predisposition can have beneficial effects on the individual. A few diseases or susceptibilities to diseases, in addition to their deleterious effects, confer adaptive protection against specific environmental pathogens. This advantage may explain the high prevalence of a disease in areas where the specific pathogen for another disease is endemic.
CHARACTERISTICS OF DISEASE
All diseases have a set of characteristic features enabling them to be better understood, categorised and diagnosed. For many diseases, however, our knowledge is still incomplete or subject to controversy. The characteristics of any disease are (Fig. 2.1):
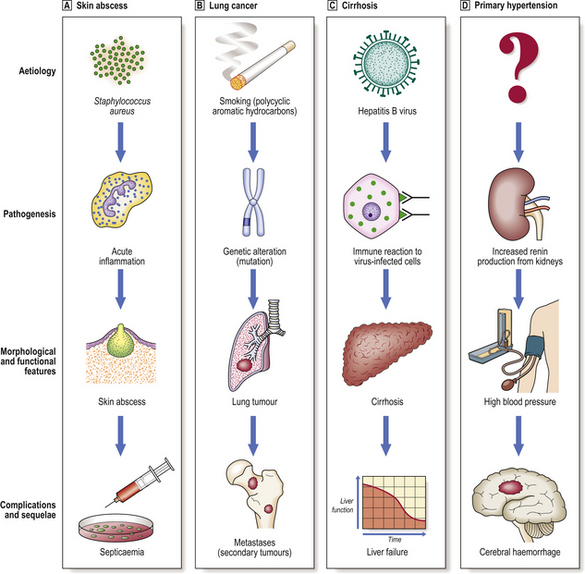
Fig. 2.1 Characteristics of disease. The relationship between aetiology, pathogenesis, morphological and functional manifestations, and complications and sequelae is exemplified by four diseases.  Skin abscess.
Skin abscess.  Lung cancer.
Lung cancer.  Cirrhosis.
Cirrhosis.  Primary hypertension.
Primary hypertension.
The aetiology and pathogenesis of a disease may be combined as aetiopathogenesis.
Aetiology
The aetiology of a disease is its cause: the initiator of the subsequent events resulting in the patient’s illness. Diseases are caused by a variable interaction between host (e.g. genetic) and environmental factors. Environmental causes of diseases are called pathogens, although this term is used commonly only when referring to microbes; bacteria capable of causing disease are pathogenic bacteria and those that are harmless are non-pathogenic.
General categories of aetiological agents include:
Some diseases are due to a combination of causes, such as genetic factors and infective agents, and are said to have a multifactorial aetiology.
Sometimes the aetiology of a disease is unknown, but the disease is observed to occur more commonly in people with certain constitutional traits, occupations, habits or habitats; these are regarded as risk factors. These factors may provide a clue to an as yet unidentified aetiological agent. Other risk factors may simply have a permissive effect, facilitating the development of a disease in that individual; examples include malnutrition, which favours infections.
Some agents can cause more than one disease depending on the circumstances; for example, ionising radiation can cause rapid deterioration leading to death, scarring of tissues, or tumours.
Identification of the causes of disease
In terms of causation, diseases may be:
Most common diseases have an entirely environmental cause, but genetic influences in disease susceptibility are being increasingly discovered, and many diseases with no previously known cause are being shown to be due to genetic abnormalities (Ch. 3). This is the reward of applying the principles of clinical genetics and the new techniques of molecular biology to the study of human disease. The extent to which a disease is due to genetic or environmental causes can often be deduced from some of its main features or its association with host factors.
Features pointing to a significant genetic contribution to the occurrence of a disease include a high incidence in particular families or races, or an association with an inherited characteristic (e.g. gender, blood groups, histocompatibility alleles). Diseases associated with particular occupations or geographic regions tend to have an environmental basis; the most abundant environmental causes of disease are microbes (bacteria, viruses, fungi, etc.).
Probability of disease
The relationship between the quantity of causal agent and the probability that disease will result is not always simply linear (Fig. 2.2). For example, many infections occur only on exposure to a sufficient dose of micro-organisms; the body’s defence mechanisms have to be overcome before disease results. Some agents capable of causing disease, such as alcohol, are actually beneficial in small doses; those who abstain from alcohol have a slightly higher risk of premature death from ischaemic heart disease.
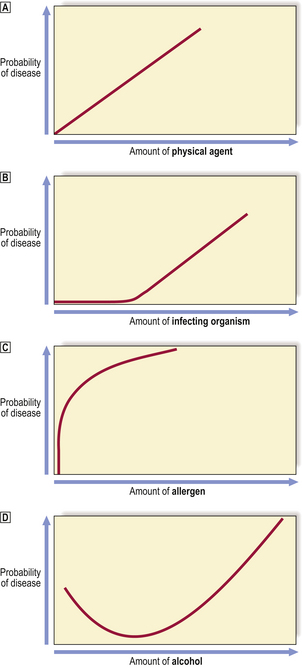
Fig. 2.2 Relationships between the amount of a causal agent and the probability of disease.  Physical agents. For example, the risk of traumatic injury to a pedestrian increases in proportion to the kinetic energy of the motor vehicle.
Physical agents. For example, the risk of traumatic injury to a pedestrian increases in proportion to the kinetic energy of the motor vehicle.  Infectious agents. Many infectious diseases result only if sufficient numbers of the micro-organism (e.g. bacterium, virus) are transmitted; smaller numbers are capable of being eliminated by the non-immune and immune defences.
Infectious agents. Many infectious diseases result only if sufficient numbers of the micro-organism (e.g. bacterium, virus) are transmitted; smaller numbers are capable of being eliminated by the non-immune and immune defences.  Allergens. In sensitised (i.e. allergic) individuals, minute amounts of an allergen will provoke a severe anaphylactic reaction.
Allergens. In sensitised (i.e. allergic) individuals, minute amounts of an allergen will provoke a severe anaphylactic reaction.  J-shaped curve. Best exemplified by alcohol, of which small doses (c. 1–2 units per day) reduce the risk of premature death from ischaemic heart disease, but larger doses progressively increase the risk of cirrhosis.
J-shaped curve. Best exemplified by alcohol, of which small doses (c. 1–2 units per day) reduce the risk of premature death from ischaemic heart disease, but larger doses progressively increase the risk of cirrhosis.
Host predisposition to disease
Many diseases are the predictable consequence of exposure to the initiating cause; host factors make relatively little contribution. This is particularly true of physical injury: the immediate results of mechanical trauma or radiation injury are dose-related; the outcome can be predicted from the strength of the injurious agent.
Other diseases are the probable consequence of exposure to causative factors, but they are not inevitable. This is exemplified by infections with potentially harmful bacteria: the outcome can be influenced by various host factors such as nutritional status, genetic influences and pre-existing immunity.
Some diseases occur more commonly in individuals with a congenital predisposition. For example, ankylosing spondylitis (Ch. 25), a disabling inflammatory disease of the spinal joints of unknown aetiology, occurs more commonly in individuals with the HLA-B27 allele.
Some diseases predispose patients to the risk of developing other diseases. Diseases associated with an increased risk of cancer are designated premalignant conditions; for example, hepatic cirrhosis predisposes to hepatocellular carcinoma, and ulcerative colitis predisposes to carcinoma of the large intestine. The histologically identifiable antecedent lesion from which the cancers directly develop is designated the premalignant lesion.
Some diseases predispose to others because they have a permissive effect, allowing environmental agents that are not normally pathogenic to cause disease. This is exemplified by opportunistic infections in patients with impaired defence mechanisms resulting in infection by organisms not normally harmful (i.e. non-pathogenic) to humans (Ch. 9). Patients with leukaemia or the acquired immune deficiency syndrome (AIDS), organ transplant recipients, or other patients treated with cytotoxic drugs or steroids, are susceptible to infections such as pneumonia due to Aspergillus fungi, cytomegalovirus or Pneumocystis jiroveci.
Causes and agents of disease
It is argued that a distinction should be made between the cause and the agent of a disease. For example, tuberculosis is caused, arguably, not by the tubercle bacillus (Mycobacterium tuberculosis) but by poverty, social deprivation and malnutrition—the tubercle bacillus is ‘merely’ the agent of the disease; the underlying cause is adverse socio-economic factors. There is, in fact, incontrovertible evidence that the decline in incidence of many serious infectious diseases is attributable substantially to improvements in hygiene, sanitation and general nutrition rather than to immunisation programmes or specific antimicrobial therapy. Such arguments are of relevance here only to emphasise that the socio-economic status of a country or individual may influence the prevalence of the environmental factor or the host susceptibility to it. In practice, causes and agents are conveniently embraced by the term aetiology.
Causal associations
A causal association is a marker for the risk of developing a disease, but it is not necessarily the actual cause of the disease. The stronger the causal association, the more likely it is to be the aetiology of the disease. Causal associations become more powerful if:
The utility of these statements is exemplified by reference to the association between lung cancer and cigarette smoking. Lung cancer is more common in smokers than in non-smokers; tobacco yields carcinogenic chemicals; the risk of lung cancer is proportional to cigarette consumption; population groups that have reduced their cigarette consumption (e.g. doctors) show a commensurate reduction in their risk of lung cancer.
Causal associations may be neither exclusive nor absolute. For example, because some heavy cigarette smokers never develop lung cancer, smoking cannot alone be regarded as a sufficient cause; other factors are required. Conversely, because some non-smokers develop lung cancer, smoking cannot be regarded as a necessary cause; other causative factors must exist.
Causal associations tend to be strongest with infections. For example syphilis, a venereal disease, is always due to infection by the spirochaete Treponema pallidum; there is no other possible cause for syphilis; syphilis is the only disease caused by Treponema pallidum.
Koch’s postulates
An infective (e.g. bacterial, viral) cause for a disease is not usually regarded as proven until it satisfies the criteria enunciated by Robert Koch (1843–1910), a German bacteriologist and Nobel prizewinner in 1905:
The last was added subsequently to Koch’s list. Although Koch’s postulates have lost their novelty, their relevance is undiminished. However, each postulate merits further comment because there are notable exceptions:
Pathogenesis
The pathogenesis of a disease is the mechanism through which the aetiology (cause) operates to produce the pathological and clinical manifestations. Groups of aetiological agents often cause disease by acting through the same common pathway of events.
Examples of pathogeneses of disease include:
These pathways of disease development constitute our knowledge of general pathology, and their description forms Part 2 of this textbook.
Latent intervals and incubation periods
Few aetiological agents cause signs and symptoms immediately after exposure. Usually, some time elapses. In the context of carcinogenesis, this time period is referred to as the latent interval; it is often two or three decades. In infectious disorders (due to bacteria, viruses, etc.), the period between exposure and the development of disease is called the incubation period; it is often measured in days or weeks, and each infectious agent is usually associated with a characteristic incubation period.
The reason for discussing these time intervals here is that it is during these periods that the pathogenesis of the disease is being enacted, culminating in the development of symptomatic pathological and clinical manifestations that cause the patient to seek medical help.
Structural and functional manifestations
The aetiological agent (cause) acts through a pathogenetic pathway (mechanism) to produce the manifestations of disease, giving rise to clinical signs and symptoms (e.g. weight loss, shortness of breath) and the abnormal features or lesions (e.g. carcinoma of the lung) to which the clinical signs and symptoms can be attributed. The pathological manifestations may require biochemical methods for their detection and, therefore, should not be thought of as only those visible to the unaided eye or by microscopy. The biochemical changes in the tissues and the blood are, in some instances, more important than the structural changes, many of which may appear relatively late in the course of the disease.
Although each separately named disease has its own distinctive and diagnostic features, it is possible to generalise about the range of structural and functional abnormalities, alone or combined, resulting in ill health.
Structural abnormalities
Common structural abnormalities causing ill health are:
Other structural abnormalities, visible only by light or electron microscopy, are very common and, even though they do not directly cause clinical signs or symptoms, they are nevertheless diagnostically useful and often specific manifestations of disease. For this reason, the morphological examination of diseased tissues is very rewarding for patient management and for clinical research. At an ultrastructural level (electron microscopy), one might see alien particles such as viruses in the affected tissue; there could be abnormalities in the number, shape, internal structure or size of tissue components such as intracellular organelles or extracellular material. By light microscopy, abnormalities in cellular morphology or tissue architecture can be discerned. Immunohistochemistry (Ch. 4) can be used to make visible otherwise invisible, but important, alterations in cells and tissues. With the unaided eye, changes in the size, shape or texture of whole organs can be discerned either by direct inspection or by indirect means such as radiology.
Functional abnormalities
Examples of functional abnormalities causing ill health include:
What makes patients feel ill?
The ‘feeling’ of illness is usually due to one or a combination of common symptoms:
Each of these common symptoms has a pathological basis and, in those conditions that remit spontaneously, all that is required for treatment is symptomatic relief.
In addition to the general symptoms of disease, there are other specific expressions of illness that help to focus attention, diagnostically and therapeutically, on a particular organ or body system. Examples include:
The symptoms of disease (the patient’s presenting complaints) invariably have an identifiable scientific basis. This is important to know because often nothing more than symptomatic treatment is required because either the disease will remit spontaneously (e.g. the common cold) or there is no prospect of recovery (e.g. disseminated cancer). Examples of known mediators of symptoms are listed in Table 2.1.
Table 2.1 Examples of the known mediators of the symptoms of disease
| Symptom | Mediators | Comment |
|---|---|---|
| Pain | Free nerve endings stimulated by mechanical, thermal or chemical agents (e.g. bradykinin, 5-HT, histamine; prostaglandins enhance sensitivity) | May signify irritation of a surface (e.g. peritoneum), distension of a viscus (e.g. bladder), ischaemia (e.g. angina), erosion of a tissue (e.g. by tumour) or inflammation |
| Swelling | Increased cell number or size, or abnormal accumulation of fluid or gas | Common manifestation of inflammation and of tumours |
| Shortness of breath (dyspnoea) | Increased blood CO2 or, to a lesser extent, decreased blood O2 concentration | Usually due to lung disease, heart failure or severe anaemia |
| Fever (pyrexia) | Interleukin-1 (IL-1) released by leukocytes acts on thermoregulatory centre in hypothalamus, mediated by prostaglandins (PG) |
Weight lossInadequate food intake or catabolic state mediated by humoral factors from tumoursCommon manifestation of cancer, not necessarily of the alimentary tract or disseminatedBleedingWeakness or rupture of blood vessel wall or coagulation defectCoagulation defects lead to spontaneous bruising or prolonged bleeding after injuryDiarrhoeaMalabsorption of food results in osmotic retention of water in stoolsMost commonly due to infective causes not requiring specific treatment other than fluid replacementDecreased transit time, possibly due to humoral effectsDamage to mucosa impairing absorption and exuding fluidItching (pruritus)Mast cell degranulation and release of histamineManifestation of, for example, allergyCoughNeuropeptide release in response, usually, to irritation of respiratory mucosaCommon manifestation of respiratory tract diseaseVomitingStimulation of vomiting centre in medulla, usually by afferent vagal impulsesUsually denotes upper gastrointestinal disease (e.g. gastroenteritis), but may be due to CNS lesionsCyanosisReduced oxygen content of arterial haemoglobinDue to respiratory disease, cardiac failure or congenital shunting
Lesions
A lesion is the structural or functional abnormality responsible for ill health. Thus, in a patient with myocardial infarction, the infarct or patch of dead heart muscle is the lesion; this lesion is in turn a consequence of another lesion—occlusion of the supplying coronary artery by a thrombus (coronary artery thrombosis). A lesion may be purely biochemical, such as a defect in haemoglobin synthesis in a patient with a haemoglobinopathy.
Of course, not all diseases have overtly visible lesions associated with them, despite profound consequences for the patient; for example, schizophrenia and depressive illness yield nothing visibly abnormal in the brain if examined using conventional methods.
Pathognomonic abnormalities
Pathognomonic features are restricted to a single disease, or disease category, and without them the diagnosis is impossible or uncertain. For example, Reed–Sternberg cells are said to be pathognomonic of Hodgkin’s disease; they are exceptionally rare in any other condition. Similarly, the presence of Mycobacterium tuberculosis, in the appropriate context, is pathognomonic of tuberculosis.
Pathognomonic abnormalities are extremely useful clinically, because they are absolutely diagnostic. Their presence leaves no doubt about the diagnosis. Unfortunately, some diseases are characterised only by a combination of abnormalities, none of which on its own is absolutely diagnostic; it is the particular combination that is diagnostic. Some diseases characterised by multiple abnormalities are called syndromes (p. 20).
Complications and sequelae
Diseases may have prolonged, secondary or distant effects. Examples include the spread of an infective organism from the original site of infection, where it had provoked an inflammatory reaction, to another part of the body, where a similar reaction to it will occur. Similarly, malignant tumours arise initially in one organ as primary tumours, but tumour cells eventually permeate lymphatics and blood vessels and thereby spread to other organs to produce secondary tumours or metastases. The course of a disease may be prolonged and complicated if the body’s capacity for defence, repair or regeneration is deficient.
Prognosis
The prognosis forecasts the known or likely course of the disease and, therefore, the fate of the patient. When we say that the 5-year survival prospects for carcinoma of the lung are about 5%, this is the prognosis for that condition. Sometimes we can be very specific because the information available about an individual patient and their disease may enable an accurate forecast; for example, a patient who presents with a carcinoma of the lung that has already spread to the liver, bones and the brain very probably (and unfortunately) has a 6-month survival prospect of nil.
The prognosis for any disease is of course subject to influence by medical or surgical intervention. So one must distinguish between the prognosis for a disease that is allowed to follow its natural course and the prognosis for the same disease in a group of patients receiving appropriate therapy.
In assessing the long-term prognosis for a chronic disease, it is important to compare the survival of a group of patients with actuarial data for comparable populations without the disease. The survival data for the group with the disease should be corrected to allow for deaths that are likely to occur from other diseases.
Remission and relapse
Not all chronic diseases pursue a relentless course. Some are punctuated by periods of quiescence when the patient enjoys relatively good health. Remission is the process of conversion from active disease to quiescence. Later, the signs and symptoms may reappear; this is the process of relapse. Some diseases may oscillate through several cycles of remission and relapse before the patient is cured of or succumbs to the disease. Diseases characterised by a tendency to remit and relapse include chronic inflammatory bowel disease (Crohn’s disease and ulcerative colitis) and treated acute leukaemia (particularly in childhood).
The tendency of some diseases to go through cycles of remission and relapse can make it difficult to be certain about prognosis in an individual case.
Morbidity and mortality
The morbidity of a disease is the sum of the effects upon the patient. The morbidity of a disease may or may not result in disability of the patient. For example, a non-fatal myocardial infarct (heart attack) leaves an area of scarring of the myocardium, impairing its contractility and predisposing to heart failure: this is the morbidity of the disease in that particular patient. The heart failure manifests itself with breathlessness, restricting the patient’s activities: this is the patient’s disability.
The mortality of a disease is the probability that death will be the end result. Mortality is expressed usually as a percentage of all those patients presenting with the disease. For example, the mortality rate of myocardial infarction could be stated as 50% under defined circumstances.
Disability and disease
Many diseases result in only transient disability; for example, influenza or a bad cold may necessitate time off work for an employed person. Some diseases, however, are associated with a significant risk of permanent disability; in such cases, treatment is intended to minimise the risk of disability. Some investigations and treatments carry a small risk of harm, often permanent, and the risk of disability must be outweighed by the potential benefit to the patient.
As a general rule, the earlier a disease is diagnosed, the smaller the risk of disability either from the disease itself or from necessary treatment. This is one of the main objectives of screening programmes for various conditions (e.g. for cancers of the cervix and breast). The objective assessment, preferably measurement, of disability is important in the evaluation of the impact of a disease or the adverse effects of its treatment. There is, for example, a balance between the longevity of survival from a disease and the quality of life during the period of survival after diagnosis: a treatment that prolongs life may be unacceptable because it prolongs suffering; treatment that makes a patient more comfortable, but does not prolong life and may actually shorten it, may be more acceptable. The measure that takes account of the duration and quality of survival is QALYs (quality–adjusted life years), and enables scientifically based judgements about the impact of diseases, treatments and preventive measures.
NOMENCLATURE OF DISEASE
Before proceeding to a detailed discussion of disease it is important to clarify the meaning of some of the common terms, prefixes and suffixes used in the nomenclature of diseases and their pathological features. Until the 19th century, many diseases and causes of death were recorded in a narrative form, often based on symptoms. The early medical statisticians, William Farr (1807–1883) and Jacques Bertillon (1851–1922), pioneered a systematic and uniform approach to disease classification, thereby laying the foundations of modern disease nomenclature.
Primary and secondary
The words primary and secondary are used in two different ways in the nomenclature of disease:
Secondary means that the disease represents a complication or manifestation of some underlying lesion. Thus, secondary hypertension is defined as abnormally high blood pressure as a consequence of some other lesion (e.g. renal artery stenosis).
Acute and chronic
Acute and chronic are terms used to describe the dynamics of a disease. Acute conditions have a rapid onset, often but not always followed by a rapid resolution. Chronic conditions may follow an acute initial episode, but often are of insidious onset, and have a prolonged course lasting months or years. Subacute, a term not often used now, is intermediate between acute and chronic. These terms are most often used to qualify the nature of an inflammatory process. However, they can be used to describe the dynamics of any disease. The words may be used differently by patients to describe some symptoms, such as an ‘acute’ pain being sharp or severe.
Benign and malignant
Benign and malignant are emotive terms used to classify certain diseases according to their likely outcome. Thus, benign tumours remain localised to the tissue of origin and are very rarely fatal unless they compress some vital structure (e.g. brain), whereas malignant tumours invade and spread from their origin and are commonly fatal. Benign hypertension is relatively mild elevation of blood pressure that develops gradually and causes insidious injury to the organs of the body. This situation contrasts with malignant hypertension, in which the blood pressure rises rapidly and causes severe symptoms and tissue injury (e.g. headaches, blindness, renal failure, cerebral haemorrhage).
Eponymous names
An eponymous disease or lesion is named after a person or place associated with it. Eponymous names are used commonly either when the nature or cause of the disease or lesion is unknown, or when long-term usage has resulted in the name entering the language of medicine, or to commemorate the person who first described the condition. Examples include:
Syndromes
A syndrome is an aggregate of signs and symptoms or a combination of lesions without which the disease cannot be recognised or diagnosed. Syndromes often have eponymous titles. Examples include:
Numerical coding systems
Standard numerical codes, rather than names, are often used for disease registration and in epidemiological studies. Each disease or disease group is designated a specific number. The most widely used systems are ICD (International Classification of Diseases, a World Health Organization System) and SNOMED (Systematized Nomenclature of Medicine).
PRINCIPLES OF DISEASE CLASSIFICATION
Diseases do not occur to conform to any classification. Disease classifications are creations of medical science and are justified only by their utility. Classifications are useful in diagnosis to enable a name (disease or disease category) to be assigned to a particular illness.
Disease classification at a relatively coarse level of categorisation is unlikely to change quickly. However, the more detailed the level of classification, the more likely it is to change as medical science progresses. The general classification of disease into categories such as inflammatory and neoplastic (see below) is long established.
General classification of disease
The most widely used general classification of disease is that based on pathogenesis or disease mechanisms (Fig. 2.3). Most diseases can be assigned a place in the following classification:
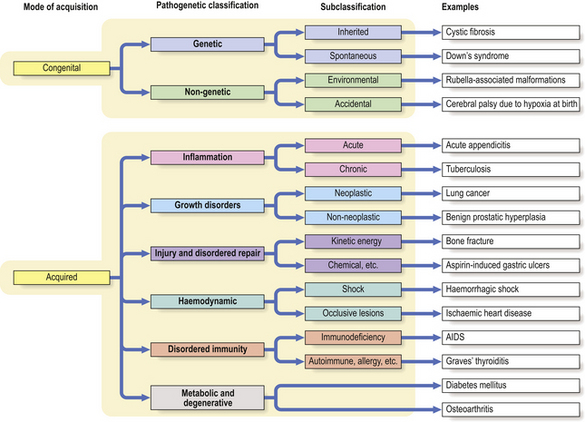
Fig. 2.3 A general classification of disease. The most widely used general classification of disease is based on the mode of acquisition of the disease (i.e. congenital or acquired) and the principal disease mechanism (e.g. genetic, vascular). The main pathogenetic classes are divided into two or more subclasses. There is, however, significant overlap and many acquired diseases are more common in those with a genetic predisposition.
Two important points must be made here. First, the above classification is not the only possible classification of disease. Second, many diseases share characteristics of more than one of the above categories.
Patients might prefer the following disease classification:
This classification is perfectly legitimate and may be foremost in the patient’s mind, but it is not particularly useful either as a diagnostic aid or for categorisation according to the underlying pathology.
Congenital diseases
Congenital abnormalities (genetic/chromosome disorders and malformations) occur in approximately 5% of births in the UK. They comprise:
Common malformations include congenital heart defects, spina bifida and limb deformities. Single gene defects include conditions such as phenylketonuria and cystic fibrosis. Chromosomal aberrations are exemplified by Turner’s syndrome (XO sex chromosomes) and Down’s syndrome (trisomy 21—three copies of chromosome 21). The risk of chromosomal abnormalities increases with maternal age: for example, the risk of a child being born with Down’s syndrome, the commonest chromosome abnormality, is estimated at 1 in 1500 for a 25-year-old mother, rising to 1 in 30 at the age of 45 years.
Congenital diseases are initiated before or during birth, but some may not cause clinical signs and symptoms until adult life. Congenital diseases may be due to genetic defects, either inherited from the parents or genetic mutations before birth, or to external interference with normal embryonic and fetal development. An example of a genetic defect is cystic fibrosis, which is a disorder of cell membrane transport inherited as an autosomal recessive abnormality. Examples of non-genetic defects include congenital diseases such as deafness and cardiac abnormalities resulting from fetal infection by maternal rubella (German measles) during pregnancy.
A common natural consequence of an abnormal pregnancy is a miscarriage or spontaneous abortion. However, some abnormal pregnancies escape natural elimination and may survive to full-term gestation unless there is medical intervention.
Fetal origins of adult disease
Some diseases occurring in late adult life, such as ischaemic heart disease, are more common in individuals who had a low weight at birth. This is postulated to be due to subtle abnormalities of morphogenesis associated with nutritional deprivation in utero (the ‘Barker hypothesis’).
Acquired diseases
Acquired diseases are due to environmental causes. Most diseases in adults are acquired.
Acquired diseases can be further classified according to their pathogenesis.
Inflammatory diseases
Inflammation (Ch. 10) is a physiological response of living tissues to injury. Diseases in which an inflammatory reaction is a major component are classified accordingly. They are usually named from the organ affected followed by the suffix ‘-itis’. Thus the following are all examples of inflammatory diseases:
There are, however, potentially confusing exceptions to the nomenclature. For example, tuberculosis, leprosy and syphilis are infections characterised by an inflammatory reaction. Pneumonia and pleurisy refer to inflammation of the lung and pleura respectively.
Each separate inflammatory disease has special features determined by:
Vascular disorders
Vascular disorders (Chs 8 and 13) are those resulting from abnormal blood flow to, from or within an organ. Blood vessels are vital conduits. Any reduction in flow through a vessel leads to ischaemia of the tissue it supplies. If the ischaemia is sustained, then death of the tissue or infarction results. Vascular disorders have become major health problems in developed countries. Examples include:
Growth disorders
Diseases characterised by abnormal growth include adaptation to changing circumstances. For example, the heart enlarges (by hypertrophy) in patients with high blood pressure, and the adrenal glands shrink (by atrophy) if a disease of the pituitary gland causes loss of ACTH production. The most serious group of diseases characterised by disordered growth is neoplasia or new growth formation, leading to the formation of solid tumours (Ch. 11) and leukaemias (Ch. 23).
The suffix ‘-oma’ usually signifies that the abnormality is a solid tumour. Exceptions include ‘granuloma’, ‘haematoma’ and ‘atheroma’; these are not tumours.
Injury and repair
Mechanical injury or trauma leads directly to disease, the precise characteristics of which depend upon the nature and extent of the injury. The progress of disease is influenced by the body’s reaction to it. In particular, repair mechanisms may be defective due to old age, malnutrition, excessive mobility, presence of foreign bodies, and infection. This subject is discussed in detail in Chapter 6.
Metabolic and degenerative disorders
Metabolic and degenerative disorders are numerous and heterogeneous. Some metabolic disorders are congenital (inborn errors of metabolism) and due to defective parental genes. Other metabolic disorders are mainly acquired (e.g. diabetes mellitus, gout), although there may be a degree of genetic predisposition, and some are abnormalities secondary to disease (e.g. hypercalcaemia due to hyperparathyroidism). Degenerative disorders are characterised by a loss of the specialised structure and function of a tissue; as such, this category could include almost every disease, but the designation is reserved for those conditions in which degeneration appears to be the primary or dominant feature and the cause poorly understood. These disorders are discussed in detail in Chapter 7.
Iatrogenic diseases
The broad meaning of iatrogenic disease is any ill health induced by a medical practitioner’s words or actions. Currently, iatrogenic diseases are regarded as those attributable to practitioners’ actions. However, the suggestion that words could induce harm is not as fanciful as it seems. For example, a patient with a relatively trivial respiratory complaint is likely to be alarmed when asked by a doctor, who mistakenly suspects lung cancer, ‘How much weight have you lost?’ and ‘Have you coughed up any blood?’ The disturbing suggestions implicit in the line of questioning cause iatrogenic ‘dis-ease’ in the patient. (While it is perfectly reasonable to consider the possibility of lung cancer, such questions are better asked in the neutral form of ‘What’s been happening to your weight recently?’ and ‘Have you noticed anything about your sputum?’)
All medical intervention is associated with some risk to the patient. Ethically, the probability that harm might result must be outweighed by the probability that the patient will benefit. If harm results, litigation may follow. However, there is a considerable difference in principle between harm resulting from culpable negligence and that resulting from appropriate intervention justified by the clinical circumstances.
The scope of iatrogenic diseases is very wide (Table 2.2). It includes harm resulting from investigations and treatment, from drugs and surgery. It is said, with justification, that in the 20th century surgery became safer while medicine became more dangerous. Adverse drug reactions constitute a major category of iatrogenic disease and surveillance arrangements are in force in many countries, for example the ‘yellow card’ system of reporting to the Commission on Human Medicines in the UK.
Table 2.2 Examples of iatrogenic diseases
| Causative agent | Resulting disease or abnormality |
|---|---|
| Radiation (therapeutic) |
Radiation (diagnostic)
Blood transfusion and blood products (e.g. clotting factor concentrates)
PenicillinAllergyAspirin and other non-steroidal anti-inflammatory drugsGastritis and gastric erosionsAminoglycoside antibioticsDeafnessChlorpromazineCholestatic jaundiceSteroid therapyCushing’s syndrome
Adverse drug reactions
Adverse drug reactions can be categorised as follows:
Dose-dependent drug reactions occur predictably in any person taking a sufficient dose of the drug. For example, paracetamol always produces hepatic necrosis if, unwisely, a sufficiently large dose is taken. Similarly, steroids can cause Cushing’s syndrome (obesity, hirsutism, osteoporosis, etc.) in any patient receiving doses in excess of the usual bodily requirements. Often, the adverse effects disappear when the dosage is reduced, and mortality tends to be low.
Unpredictable adverse drug reactions are due to:
One of the commonest idiosyncratic drug reactions is due to allergy to penicillin. Another common example is cholestatic jaundice induced by chlorpromazine. Idiosyncratic reactions are due to unexpected metabolic or immunological responses to the drug. This type of drug reaction merits withdrawal of the drug and substitution of alternative therapy. The mortality rate is higher than that associated with predictable reactions.
In unpredictable adverse drug reactions where the effect is permissive, the drug itself produces no harm, but it predisposes the patient to other diseases. For example, some antibiotic therapy may be complicated by pseudomembranous colitis (Ch. 15) because it permits overgrowth of Clostridium difficile in the colon. Steroids and other immunosuppressive agents predispose to infections by organisms that would not normally be harmful (e.g. Pneumocystis jiroveci pneumonia, cytomegalovirus pneumonia).
EPIDEMIOLOGY
Epidemiology is the study of disease in populations. It also concerns the identification of the causes and modes of acquisition of disease. Epidemiology involves recording and analysing data about disease in groups of people rather than in the individual patient.
Knowledge about the population characteristics of a disease is important for:
Epidemiological clues to the causes of disease
Epidemiology, sometimes referred to as the ‘pathology of populations’, often provides important clues to the causes of a disease. If, for example, in a particular geographical region or group of individuals the actual incidence of a disease exceeds the expected incidence, this suggests that the disease may be due to:
The analysis of epidemiological data can be very arduous. Humans live in a complex and changing environment, often modified by their own action. Populations vary in their ethnic origins, their age distribution, their occupational histories and their lifestyles. These variations and the concomitant variations in disease incidence provide fertile opportunities for epidemiological study.
Epidemiologically derived clues about the causes of a disease invariably require direct confirmation by laboratory testing.
Disease incidence, prevalence, remission and mortality rates
Incidence, prevalence, remission and mortality rates are numerical data about the impact of a disease on a population:
From these four measures one can deduce much about the behaviour of a disease (Fig. 2.4). Chronic (long-lasting) diseases have a high prevalence: although the incidence of new cases might be low, the total number of cases in the population accumulates. Diseases with relatively acute manifestations may have a high incidence but a low prevalence, because cases have either high remission rates (e.g. chickenpox) or high mortality rates (e.g. lung cancer).
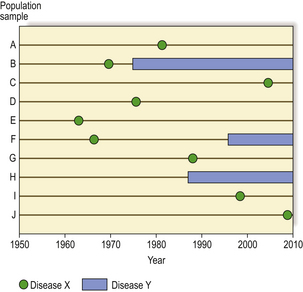
Fig. 2.4 Disease incidence and prevalence. A population sample of 10 individuals (A to J), all born in 1950, is followed for 60 years to determine the relative incidence and prevalence of two diseases. Disease X is an acute illness with no long-term effects; it has a very high incidence (affecting 90% in this sample), but a low prevalence because at any one time the number of cases to be found is very low. Disease Y is a chronic illness; it has a lower incidence (affecting only 30% in this sample) but a relatively high prevalence (from 1990 onwards in this sample) because of the accumulation of cases in the population.
In comparing the occurrence of a disease in different populations, epidemiologists have to standardise the data to eliminate any bias due to the average age of the population and its life expectancy. Diseases that are more common in the elderly may be relatively rare in some populations, simply because most of the people do not live long enough to develop them.
Migrant populations are especially useful to epidemiologists, enabling them to separate the effects of genetic (racial) factors and the environment (e.g. diet) (Ch. 3).
The net effect of disease and nutritional deprivation on a population can be illustrated as age pyramids, the profiles often revealing striking contrasts between countries (Fig. 2.5).
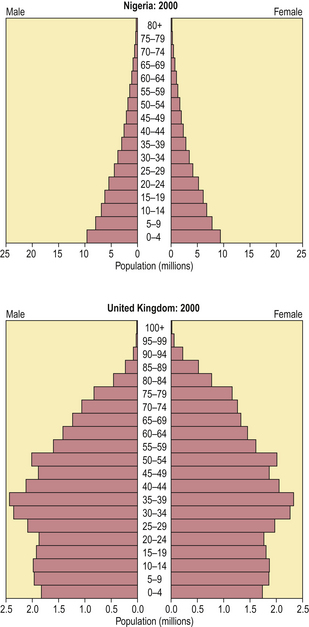
Fig. 2.5 National health revealed by age pyramids. In Nigeria, among other African countries, disease and nutritional problems severely curtail life expectancy. In the United Kingdom, among other ‘developed countries’, a high proportion of the population survives into old age, albeit often accompanied by chronic ill health.
(Data from US Census Bureau, International Data Base)
Data capture
Data on the frequency of diseases are often more likely to be in the form of mortality statistics rather than actual disease incidence. The reason is that, unless legislation requires cases of the disease under study to be formally notified to some register, the most reliable data are likely to be derived from official death certificates. This means that, if a disease does not often have a fatal outcome, mortality data will severely underestimate its incidence. The only common exceptions to this are certain infectious diseases, designated as notifiable in the UK, and cancers, for which many developed countries have registries.
In countries with well-developed health care systems, the epidemiology of many serious diseases should be relatively easy to determine from statistical data already held on databases (e.g. cancer registries); retrospective studies are usually possible. In countries with relatively poor systems, however, it may be necessary to search actively for the disease in order to determine its true incidence and the distribution in the general population; most studies have to be done prospectively.
Geographic variations
Although many diseases occur worldwide, there are many geographic variations, even within one country. There are considerable differences between so-called developed and developing countries; for example, cardiovascular disorders, psychiatric illness and some cancers predominate in countries such as the USA and the UK, but these conditions are less common in most of Africa and Asia. In developing countries, the major health problems are due to infections and malnutrition.
Historical changes in disease incidence and mortality
Changes in disease incidence with time (Fig. 2.6) reflect variation in the degree of exposure to the cause, or preventive measures such as immunisation. Changes in mortality additionally reflect the success of treatment.
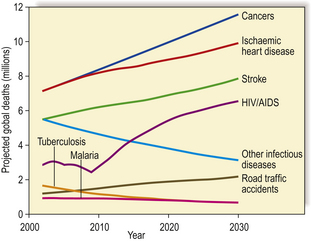
Fig. 2.6 Projected global causes of death, 2002–2030. Other than HIV/AIDS, there is an anticipated decline in mortality from infectious diseases contrasting with the steady increase in deaths from cancer and cardiovascular conditions due to ageing of the global population.
(Based on World Health Statistics 2007, World Health Organization)
The reduced incidence or elimination of serious infections (e.g. typhoid, cholera, tuberculosis, smallpox) is the result of improved sanitation and, in some instances, the effectiveness of immunisation programmes. Indeed, it is likely that sanitation, particularly sewerage and the provision of fresh water supplies, has had a much greater impact on the incidence of these diseases than have advances in medical science. Mortality from bacterial infections is also much reduced due to the advent of antibiotic therapy. Many viral infections elude specific treatment, but mass immunisation has led to a considerable reduction in their incidence.
During the 19th and 20th centuries, the declining incidence in many serious infections was accompanied by an increasing incidence of other conditions, notably cardiovascular disorders (e.g. hypertension, atherosclerosis) and their complications (e.g. ischaemic heart disease, strokes). The apparent increase is partly due to the fact that the average age of the population in most developed countries is increasing; cardiovascular disorders are more common with increasing age, unlike infections which afflict all ages. Nevertheless, irrespective of this age-related trend, there is a genuine increased incidence of these disorders. This increase is due to changes in diet (e.g. fat content) and lifestyle (e.g. smoking, lack of exercise) and the consequent obesity. Intervention by reducing dietary and behavioural risk factors has begun to yield a beneficial reduction in the risk of developing the complications of cardiovascular disorders.
Historical changes in the incidence of neoplastic diseases (i.e. tumours) can provide vital clues to their aetiology. For example, a dramatic increase in the incidence of a formerly uncommon tumour may be the result of exposure to a new environmental hazard. Historical changes led to the discovery of the association between ionising radiation and many types of cancer, and between smoking and lung cancer.
Socio-economic factors
Socio-economic factors undoubtedly influence the incidence of certain diseases and the host response to them. Overcrowding encourages the spread of infections, leading to the rapid development of epidemics. Economic hardship is commonly accompanied by malnutrition (Ch. 7), a condition causing ill health directly and also predisposing to infections.
A particularly sensitive and widely used indicator of the socio-economically related health of a population is the infant mortality rate. This rate varies considerably between countries, but in general the rate is lower in countries regarded as being developed (Fig. 2.7).
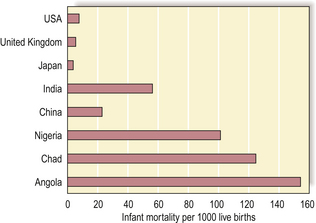
Fig. 2.7 International variations in infant mortality rates. Infant (age less than 1 year) mortality rates are important and sensitive indicators of a nation’s health and health service provision. Common causes of infant death in countries with high infant mortality rates are diarrhoeal diseases and pneumonia.
(Data derived from World Health Statistics 2007, World Health Organization)
Within a developed country, such as the UK, less affluent individuals have a higher incidence of cervical cancer, ischaemic heart disease and respiratory infections, among many other conditions.
Occupational factors
The association of a disease with a particular occupation can reveal the specific cause. Well-documented, but now less common, associations include:
It is important to identify occupational hazards so that they can be minimised. Furthermore, in many countries, patients disabled by occupational diseases may be entitled to compensation.
Hospital and community contrasts
Medical students often develop a biased impression of the true incidence of diseases because most of their training takes place in a hospital environment. The patients and diseases they see are selected rather than representative; only those cases requiring hospital investigation or treatment are sent there. For most diseases, even in countries with well-developed health services, patients remain in the community. For example, patients seen by a community medical practitioner are most likely to have psychiatric illness, upper respiratory tract infections and musculoskeletal problems. The general hospital cases are more likely to be patients with cardiovascular diseases, proven or suspected cancer, drug overdoses, severe trauma, etc.
Age and disease
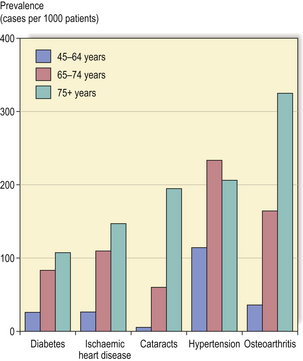
Many diseases become more prevalent with increasing age (Fig. 2.8). Indeed, the occurrence of these diseases is a key feature of elderly populations and an important determinant of health care planning.
Common causes of mortality and morbidity
Death is inevitable. In many people surviving into their seventies and eighties, death may be preceded by a variable period of senility, during which there is cumulative deterioration of the structure and function of many organs and body systems (Ch. 12). Unless an acute episode of serious illness supervenes, the accumulated deterioration of the body reduces its viability until it reaches the point where death supervenes. In almost every case, however, there is a final event that tips the balance and is registered as the immediate cause of death. In younger individuals dying prematurely, death is usually more clearly attributable to a single fatal condition in an otherwise reasonably healthy individual.
In developed countries, such as the USA and in Europe, diseases of the cardiovascular system account for much ill health (Fig. 2.9). It is estimated that a newborn infant in these countries has a 1 in 3 chance of ultimately dying in adult life from ischaemic heart disease, and a 1 in 5 chance of ultimately dying from cancer. In some famine-ridden countries, newborn infants have similar probabilities of dying from diarrhoeal diseases and malnutrition in childhood.
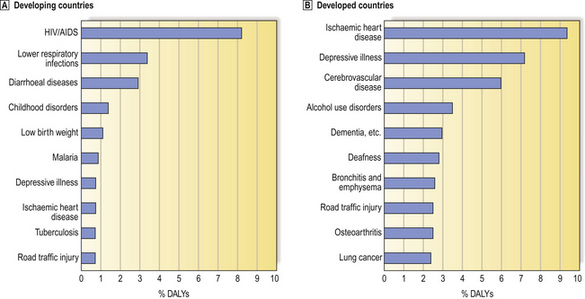
Fig. 2.9 The top ten major burdens of disease in ‘developing’ and ‘developed’ countries (2000). Based on the The World Health Report 2002 (World Health Organization), the burden of disease is estimated in disability-adjusted life years (DALYs).  In developing countries, infections such as HIV/AIDS account for much ill health and death.
In developing countries, infections such as HIV/AIDS account for much ill health and death.  In contrast, in developed countries, cardiovascular conditions are among the leading causes.
In contrast, in developed countries, cardiovascular conditions are among the leading causes.
Coggon D., Rose G., Barker D.J.P.. Epidemiology for the uninitiated. London: BMJ Publishing, 2003.
Donaldson R .J., Donaldson L .J.. Essential public health, 2nd edn. Newbury: Librapharm, 2000.
Harris E.E., Malyango A.A.. Evolutionary explanations in medical and health profession courses: are you answering your students’ ‘why’ questions? BMC Medical Education. 2005;5:16-23.
Lazarou J, Pomeranz B H. Incidence of adverse drug reactions in hospitalized patients. JAMA. 1998;279:1200-1205.
Nesse R.M., Williams G.C. Why we get sick: the new science of Darwinian medicine. New York: Vintage, 2004
Stearns S.C., Koella J.C.. Evolution in health and disease. Oxford: Oxford University Press, 2007.
Webb P., Bain C., Pirozzo S.. Essential epidemiology: an introduction for students and health professionals. Cambridge: Cambridge University Press, 2005.
World Health Organization. World Health Statistics 2007. WHO, Geneva
US Census Bureau: International Data Base. http:// www.census.gov/ipc/www/idb/index.html
World Health Organization website. http://www.who.int