17 Child with a Fever
• A fever is defined as a temperature of 38.0° C (100.4° F) or higher measured rectally.
• Response to antipyretics is not a predictor of the presence of bacterial illness and therefore should not influence clinical decision making.
• The diagnostic evaluation of a febrile child is based on clinical findings, immunization status, and age of the child.
• The peripheral white blood cell count is unreliable in determining the presence or absence of bacterial illness and should not guide diagnostic and treatment decisions.
Perspective
Fever is the most common chief complaint in children younger than 3 years seen in the emergency department (ED) (see Facts and Formulas box). Fever is defined as an elevation in temperature to 38.0° C (100.4° F) or higher. In young children, particularly those younger than 2 years, the temperature should be taken rectally because other methods such as tympanic and axillary are not as reliable or accurate.1 Parental report of fever determined by touch is likely to be accurate regarding the presence of a fever.2 A common misconception is that bundling a baby can account for an elevation in core temperature, but it cannot.3 More than 20% of fevers seen in the ED will be fevers without a source and require risk stratification based on the child’s age, appearance, and immunization status.
Infants are at particularly high risk for serious bacterial illnesses because of their minimal signs and symptoms, lack of immunity, maternal birth canal exposure, and difficulty in mounting a response to infections. To deal with this increased risk for infection, multiple protocols to evaluate a febrile infant have been developed (Box 17.1). As a general consensus, infants younger than 28 days with a temperature of 38.0° C should undergo a full sepsis evaluation, parenteral administration of antibiotics, and admission to the hospital.4 A full sepsis evaluation includes a complete blood count (CBC) with differential, blood culture, and a catheterized urine sample sent for urinalysis, Gram stain, and culture. If symptoms are present, stool studies or a chest radiograph should be performed. A lumbar puncture with cell count and differential, Gram stain, and culture should be obtained. Antibiotics recommended are ampicillin, 50 mg/kg, and cefotaxime, 50 mg/kg. Ceftriaxone is not used in the neonatal period because of possible disconjugation of bilirubin. Neonatal herpes should also be considered as a cause of the fever, particularly in infants younger than 2 weeks. Frequently, the mother’s history of maternal herpes is not known, nor does the child have any physical findings. If there is any concern, herpes polymerase chain reaction should be performed on cerebrospinal fluid and the child should be administered acyclovir (20 mg/kg). Overall, well-appearing febrile neonates have a 7% likelihood of having a serious bacterial infection, with the most common being a urinary tract infection.5–7
Box 17.1 Criteria Historically Used for Risk Stratification in Pediatric Fever
Rochester Criteria
Previously healthy term infants without perinatal complications, younger than 3 months, and no soft tissue, ear, or skeletal infections
No previous use of antimicrobials
Lack of a focus of infection on examination
Peripheral white blood cell (WBC) count: 5000-15,000/µL
Stool WBC count: up to 5 WBCs per high-power field in infants with diarrhea
Philadelphia Criteria
Observation Score
Quality of cry (strong, whimpering, weak, high pitched)
Reaction to parent stimulation (cries briefly then stops, intermittent cry, continual cry)
State variation (awake, awake with stimulation, unarousable)
Color (pink, acrocyanotic, cyanotic)
Infants 28 days to 2 to 3 months of age may be risk-stratified with the febrile infant protocol to help guide the evaluation of fever (Figs. 17.1 and 17.2). Many physicians use an age cutoff of 60 days or less to perform a full sepsis evaluation, although some physicians still perform a full sepsis evaluation in children up to 90 days of age.8 These practice variations are seen in different settings: ED-based evaluation versus office-based evaluation and academic settings versus those in private practice.9 If a young infant meets the low-risk criteria outlined in Box 17.1, the physician may send the infant home with no antibiotics and follow-up the next day (note that the Boston criteria do recommend antibiotic administration). If the physician has any reservation about the ability of the caregivers to follow-up or any social concerns, one should err on the side of caution and admit the child to the hospital. If the infant does not fall into the low-risk criteria outlined, parenteral antibiotics should be administered and the child admitted to the hospital. Parenteral antibiotics should be given only if a lumbar puncture has been performed. Antibiotics used in this age group are ceftriaxone, 50 mg/kg intravenously or intramuscularly, or cefotaxime, 50 mg/kg intravenously.
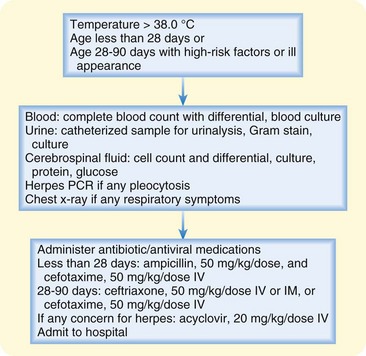
Fig. 17.1 Approach to febrile infants 0 to 28 days of age or ill-appearing children 29 to 90 days of age.
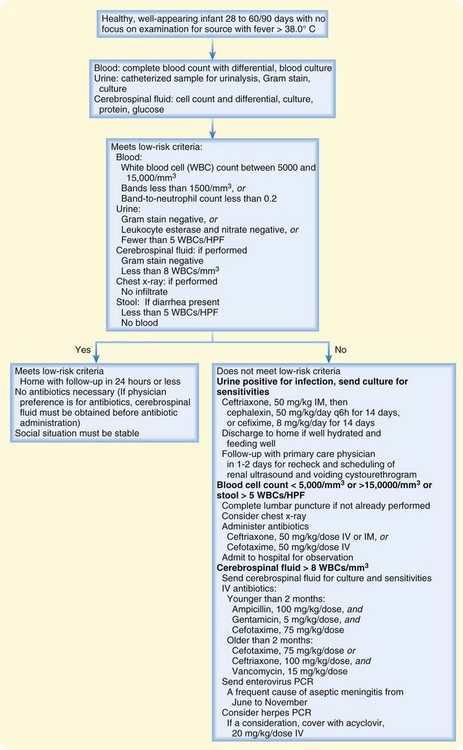
Fig. 17.2 Approach to children 28 to 90 days old with fever and no source on initial evaluation.
HPF, High-power field; PCR, polymerase chain reaction.
(Adapted from Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med 2000;36:605; and Hoberman A, Wald ER, Hickey RW, et al. Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics 1999;104:79-86.)
The approach to fever evaluation in a 2- to 3-month-old to 3-year-old has changed dramatically over the past 10 years because of vaccine development and an increasing rate of vaccination.10 An algorithm using an updated approach based on risk stratification is outlined in Figure 17.3. Before availability of the conjugated pneumococcal vaccine, a well-appearing child with a temperature of 39° C and no focus of infection would have blood drawn for a CBC and blood culture. The patient would have been administered a parenteral antibiotic if the white blood cell count was greater than 15,000/mm3.11 The concern was for occult bacteremia (OB) and possible progression of OB to meningitis. In 1987, the Haemophilus influenzae type B (Hib) vaccine was introduced and dramatically reduced the prevalence of OB secondary to Hib to the point of no longer being clinically pertinent.12 The heptavalent pneumococcal conjugated vaccine (PCV-7) was introduced in the United States in 2000 and has recently been expanded to thirteen valent (PCV-13). PCV-13 is aimed at the most invasive strains of S. pneumoniae and is administered at 2, 4, 6, and 12 to 15 months. After one dose, the vaccine has 90% efficacy against vaccine serotypes. Although the recommended vaccination schedule for the pneumococcal vaccine includes four immunizations, it has been reported that two vaccinations induce satisfactory antibody responses and may therefore be protective.13 It is thought that herd immunity may provide protection for older adults and unimmunized children.14–16
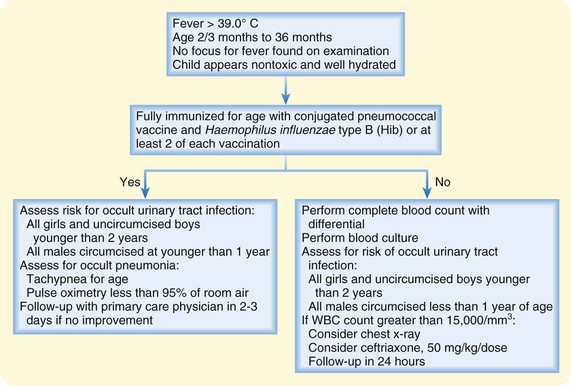
Fig. 17.3 Approach to children 3 to 36 months of age with fever and no obvious source.
(Adapted from Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med 2000;36:605.)
Lee et al. determined that at rates of pneumococcal bacteremia greater than 1.5%, obtaining a CBC, performing blood cultures, and administering antibiotics empirically was cost-effective.17 Conversely, if the rate of pneumococcal bacteremia was less than 0.5%, strategies using empiric testing and antibiotics would no longer be cost-effective. Since the work of Lee et al. several investigations have determined the overall frequency of pneumococcal bacteremia to be well below 1%.14,18,19 The rate of bacteremia may be low enough to support the evolving practice of not drawing blood for routine CBC and blood cultures in previously healthy febrile children between 2 and 36 months of age who have received at least one PCV-7 vaccination.20 Evidence is mounting that the bacteremia rate and particularly the pneumococcal bacteremia rate have declined to the extent that empiric testing and treatment may no longer be necessary.
![]() Facts and Formulas
Facts and Formulas
Fever: for ages 0 to 2 months, a temperature of 38.0° C or higher measured rectally; for ages 2 to 36 months, a temperature of 39° C or higher measured rectally
Fever without a source: acute febrile illness without localizing signs or symptoms despite a careful history and physical examination
Bacteremia: presence of bacteria in the bloodstream
Occult bacteremia: presence of bacteria in the bloodstream of a febrile child who may not appear particularly sick and has no apparent other source of infection
Serious bacterial illness: accounts for 2% to 4% of fevers. Examples include pneumonia, cellulitis, septic arthritis, osteomyelitis, urinary tract infection, meningitis, and sepsis21,22
Pathophysiology
Fever is the host’s adaptive response to an invading microorganism. The microorganism comes in contact with cells of the immune system, including macrophages and leukocytes, and such contact leads to the release of various cytokines, most notably interleukin-1, tumor necrosis factor, and interleukin-6. These cytokines circulate and come in contact with neuronal cell groups around the edges of the brain’s ventricular system. Prostaglandin E2 is then released and binds to receptors on neurons in the hypothalamus and brainstem, which leads to upregulation of the hypothalamic thermostatic set-point.23,24 Once the thermoregulatory center is reset, a higher body temperature is maintained through various mechanisms such as cutaneous vasoconstriction and shivering. The febrile response is not fully developed in young infants, and fever or even hypothermia may occur in response to infection. The physiologic limit of thermoregulation is estimated to be 41.1° C (106° F). According to McCarthy, children with a fever of this degree have a high rate of central nervous system insult.1
Presenting Signs and Symptoms
When evaluating a febrile child, the clinician must obtain key information from the history and physical examination (Box 17.2 and see the Documentation box). According to McCarthy et al., the sensitivity of clinical evaluation in an infant younger than 3 months and between 3 and 36 months of age is 78% and 89% to 92%, respectively.1,25 After the history and physical examination, the source of fever remains inapparent in 20% of febrile children.26,27
Differential Diagnosis
The differential diagnosis of acute pediatric fever is vast (Box 17.3). It is imperative to become familiar with the myriad causes of pediatric fever. The defining characteristics of each diagnosis can be found elsewhere in this text.
Diagnostic Testing
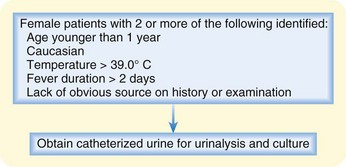
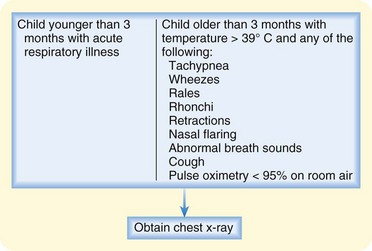
Diagnostic evaluation is based on the patient’s age group.11,26,28 Figures 17.4 and 17.5 outline the indications for other common diagnostic tests in children with fever.29–33
Urinalysis and Culture
Occult urinary tract infections occur in 2% to 3% of male infants younger than 1 year. Most of these infections occur in uncircumcised boys and infants younger than 6 months. Occult urinary tract infections occur in 8% to 9% of female children younger than 2 years.26 Girls between 2 months and 2 years of age can be risk-stratified for urinary tract infection (see Fig. 17.4) with a sensitivity of 95% and specificity of 31%.34
Urine can be collected for testing in several ways. Bag collection is a noninvasive, convenient method, but it is not recommended because of a false-positive rate of nearly 85%.25,35 Percutaneous bladder aspiration is another approach, but because this method is more invasive, it is also not the preferred approach except in male infants with severe phimosis.29 Urethral catheterization is generally regarded as the preferred method of obtaining urine, and its sensitivity and specificity are reported to be 95% and 99%, respectively.29 Once a catheterized urine specimen has been obtained, it should be sent for testing. A negative urinalysis and a negative Gram stain are not sufficient to exclude a urinary tract infection because up to 50% of patients with a urinary tract infection documented by urine culture have a false-negative urinalysis result. Therefore, it is important to obtain a urine culture in conjunction with urinalysis and a Gram stain.29,35,36
The utility of an elevated peripheral white blood cell count in evaluating a febrile child is debatable. It has been shown to be an inaccurate screen for bacteremia and meningitis in febrile infants.37,38 The decision to administer antibiotics, to perform or withhold lumbar puncture, or to admit or discharge the patient should not be based solely on interpretation of the white blood cell count.37,38
Radiography
Deciding when to perform a chest radiograph in a febrile child can be challenging. Nearly 7% of all febrile children younger than 2 years with a temperature higher than 38° C have pneumonia.34 In an investigation by Bachur et al., occult pneumonia (defined as the presence of an infiltrate on a chest radiograph in a child without clear clinical evidence of pneumonia) was discovered in up to 26% of febrile children without a source and with a white blood cell count higher than 20,000/mm3.39–41 Several criticisms of this study have been raised, including the high degree of interobserver variability in interpretation of chest radiographs, failure to perform a peripheral white blood cell count in more than half the infants with a temperature of 38° C or higher, and performance of the majority of clinical assessments by physicians in training rather than by faculty physicians.42–44 Nonetheless, data in the literature are sufficient to support the policy of the American College of Emergency Physicians, which outlines the indications for obtaining a chest radiograph in children younger than 3 years29 (see Fig. 17.5).
Treatment and Disposition
The clinician should administer appropriate dose of antipyretic early in the evaluation of a febrile child (acetaminophen, 15 mg/kg, or ibuprofen, 10 mg/kg). The response to antipyretics is not a useful determinant of the presence of bacterial illness and should not influence clinical decision making.32 Treatment and disposition of infants younger than 90 days are outlined in Figures 17.1 and 17.2. For infants managed on an outpatient basis, tests performed in the ED occasionally come back positive after the patient has been discharged. If blood cultures are positive, the child should be admitted for evaluation of sepsis and parenteral administration of antibiotics, especially in the setting of persistent fever.26 For positive urine cultures, the patient’s symptoms affect disposition. In the setting of persistent fever, the child should be admitted to the hospital for evaluation of sepsis and parenteral administration of antibiotics. In an afebrile and well-appearing child, outpatient management with oral antibiotics is a reasonable plan. Follow-up studies, including repeated cultures of urine and blood, as well as voiding cystourethrography and renal ultrasound scanning, should be arranged.
In children 2 to 3 months to 36 months of age, the clinical impression and the patient’s temperature guide management decisions. This approach is outlined in Figure 17.3. Toxic-appearing children with fever should be admitted to the hospital and treated. Well-appearing children with a temperature lower than 39° C should be treated with antipyretics and may be discharged. Laboratory testing should be withheld in these patients, and parents should be provided with instructions to return if their children have persistent fever or their condition deteriorates. In a well-appearing child with a temperature higher than 39° C, the guidelines for urine testing and chest radiography outlined in Figures 17.4 and 17.5 should be followed. Regardless of the management approach chosen, close outpatient follow-up should be ensured, and the patient’s parents should be provided with clear instructions that describe when to return to the ED for reevaluation. Box 17.4 provides information to provide to the parent. Fever is a common complaint in the ED in children younger than 36 months. The Hib and pneumococcal vaccines have reduced the incidence of OB and thus have altered the evaluation and management of febrile infants and children. This remains an evolving process, with the rate and degree of evolution yet to be determined.
Box 17.4 Information for the Parent
Goals for Care at Home
3. Monitor for worsening or life-threatening illness and return immediately to the emergency department for:
![]() Patient Teaching Tips
Patient Teaching Tips
Explain to the caretaker that a fever in the absence of a serious bacterial illness is not harmful.
Explain how to take a temperature properly.
It is best to take the infant’s or toddler’s temperature rectally.
Hold the child belly down on your lap.
Lubricate the thermometer with water-soluble jelly.
Spread the buttocks and insert the lubricated thermometer approximately 1 inch into the rectum.
Tips and Tricks
Perform most of the physical examination with the child in the parent’s lap.
Begin with less noxious components of the examination and proceed gradually to those that may be upsetting to the child (i.e., the pulmonary, cardiac, and neurologic components of the physical examination are performed before the abdominal, tympanic, and pharyngeal components).
Attempt to calm a fussy or uncooperative child through feeding, use of antipyretics, or aid of the child life team. For an apprehensive toddler, demonstrate examination of the particular body part on the parent holding the child before performing it on the child.
![]() Red Flags
Red Flags
Meningeal signs are not highly reliable in the first 12 to 16 months of life.
Remember to document the child’s general appearance carefully.
Do not overly rely on the white blood cell count to determine the extent of evaluation in an infant.
In cases in which the reliability of the caregiver is in question, it is safer to admit the patient to the hospital. Indicators of unreliable follow-up are as follows:
Close (next day) and reliable follow-up is important.
Whenever possible, consult with the infant’s pediatrician to obtain information regarding parental reliability, to discuss evaluation, and to arrange close follow-up.
In cases in which follow-up is uncertain, extensive evaluation and hospital admission are reasonable.
![]() Priority Actions
Priority Actions
Administer appropriate doses of antipyretics early in the patient’s evaluation (acetaminophen, 15 mg/kg, or ibuprofen, 10 mg/kg).
When indicated, antibiotics should be administered as early in the patient’s evaluation as possible.
Ensure close, reliable follow-up. When follow-up is uncertain, consider more extensive evaluation and hospital admission.
Baraff LJ. Management of infants and young children with fever without source. Pediatr Ann. 2008;37:673–679.
Ishimine P. Fever without source in children 0 to 36 months of age. Pediatric Clin North Am. 2006;53:167–194.
Ishimine P. The evolving approach to the young child who has fever and no obvious source. Emerg Med Clin North Am. 2007;25:1087–1115.
Joffe MD, Alpern ER. Occult pneumococcal bacteremia: a review. Pediatric Emerg Care. 2010;26:448–454.
1 McCarthy PL. Fever. Pediatr Rev. 1998;19:401–407.
2 Hooker EA, Smith SW, Miles T, et al. Subjective assessment of fever by parents: comparison with measurement by noncontact tympanic thermometer and calibrated rectal glass thermometer. Ann Emerg Med. 1996;28:313–317.
3 Grover G, Berkowitz CD, Lewis RJ, et al. The effects of bundling on infant temperature. Pediatrics. 94, 1994. 669-664
4 Baraff LJ. Management of infants and young children with fever without source. Pediatr Ann. 2008;37:673–679.
5 Baker MD, Bell LM. Unpredictability of serious bacterial illness in febrile infants from birth to 1 month of age. Arch Pediatr Adolesc Med. 1999;153:508–511.
6 Jaskiewicz JA, McCarthy CA. Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester criteria and implications for management. Pediatrics. 1994;94:390–396.
7 Kadish HA, Loverdige B, Tobey J, et al. Applying outpatient protocols in febrile infants 1-28 days of age: can the threshold be lowered? Clin Pediatr (Phila). 2009;39:81–88.
8 Baker MD, Ayner JR, Bell LM. Failure of infant observation scales in detecting illness in febrile 4- to 8-week-old infants. Pediatrics. 1990;85:1040–1043.
9 Pantell RH, Newman TB, Bernzweig J, et al. Management and outcomes of care of fever in early infancy. JAMA. 2004;291:1203–1212.
10 Joffe MD, Alpern ER. Occult pneumococcal bacteremia: a review. Pediatric Emerg Care. 2010;26:448–454.
11 Baraff LJ, Bass JW, Fleischer GF, et al. Practice guideline for the management of infants and children 0 to 36 months of age with fever without source: Agency for Healthcare Policy and Research. Ann Emerg Med. 1993;22:1198–1210.
12 Centers for Disease Control and Prevention (CDC). Progress towards elimination of Haemophilus influenzae type b disease among infants and children: 1987-1995. MMWR Morb Mortal Wkly Rep. 1996;45(42):901–906.
13 Käyhty H, Åhman H, Eriksson K, et al. Immunogenicity and tolerability of a heptavalent pneumococcal conjugate vaccine administered at 3, 5 and 12 months of age. Pediatr Infect Dis J. 2005;24:108–114.
14 Rudinsky SL, Carstairs KL, Reardon JM, et al. Serious bacterial infections in febrile infants in the post–pneumococcal conjugate vaccine era. Acad Emerg Med. 2009;16:585–590.
15 Poehling KA, Talbot TR, Griffin MR, et al. Invasive pneumococcal disease among infants before and after introduction of pneumococcal conjugate vaccine. JAMA. 2006;295:1668–1674.
16 Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348:1737–1746.
17 Lee GM, Fleisher GR, Harper MB. Management of febrile children in the age of the conjugate pneumococcal vaccine: a cost-effectiveness analysis. Pediatrics. 2001;108:835–844.
18 Stoll ML, Rubin LG. Incidence of occult bacteremia among highly febrile young children in the era of the pneumococcal conjugate vaccine. Arch Pediatr Adolesc Med. 2004;158:671–675.
19 Herz AM, Greenhow TL, Alcantara J, et al. Changing epidemiology of outpatient bacteremia in 3- to 36-month-old children after the introduction of the heptavalent-conjugated pneumococcal vaccine. Pediatr Infect Dis J. 2006;25:293–300.
20 Carstairs KL, Tanen DA, Johnson AS, et al. Pneumococcal bacteremia in febrile infants presenting to the emergency department before and after the introduction of the heptavalent pneumococcal vaccine. Ann Emerg Med. 2007;49:772–777.
21 Dagan R, Powell KR, Hall CB, et al. Identification of infants unlikely to have serious bacterial infection although hospitalized for suspected sepsis. J Pediatr. 1985;10:855–860.
22 Kuppermann N. Occult bacteremia in young febrile children. Pediatr Clin North Am. 1999;46:1073–1109.
23 Mackowiak PA. Concepts of fever. Arch Intern Med. 1998;158:1870–1881.
24 Saper CB, Breder CDL. The neurologic basis of fever. N Engl J Med. 1994;330:1880–1886.
25 McCarthy PL, Lembo RM, Fink HD, et al. Observation, history, and physical examination in diagnosis of serious illnesses in febrile children less than or equal to 24 months. J Pediatr. 1987;110:26–30.
26 Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med. 2000;36:602–614.
27 Lee G, Harper MD. Risk of bacteremia for febrile young children in the post–Haemophilus influenzae type B era. Arch Pediatr Adolesc Med. 1998;152:624–628.
28 Steere M, Sharieff GQ, Stenklyft PH. Fever in children less than 36 months of age: questions and strategies for management in the emergency department. J Emerg Med. 2003;25:149–157.
29 American College of Emergency Physicians Clinical Policies Committee. Clinical policy for children younger than three years presenting to the emergency department with fever. Ann Emerg Med. 2003;42:530–545.
30 Bramson RT, Meyer TL, Silbiger ML, et al. The futility of the chest radiograph in the febrile infant without respiratory symptoms. Pediatrics. 1993;92:524–526.
31 Leventhal JM. Clinical predictors of pneumonia as a guide to ordering chest roentgenograms. Clin Pediatr (Phila). 1982;21:730–734.
32 Baker MD, Fosarelli PD, Carpenter RO. Childhood fever: correlation of diagnosis with temperature response to acetaminophen. Pediatrics. 1987;80:315–318.
33 Scarfone RJ. Compliance with scheduled visits to a pediatric emergency department [abstract]. Acad Emerg Med. 1994;1:41A.
34 Gorelick MH, Shaw KN. Clinical decision rule to identify febrile young girls at risk for urinary tract infection. Arch Pediatr Adolesc Med. 2000;154:386–390.
35 American Academy of Pediatrics Committee on Quality Improvement, Subcommittee on Urinary Tract Infection. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. Pediatrics. 1999;103:843–852.
36 Reardon JM, Carstairs KL, Rudinsky SL, et al. Urinalysis is not reliable to detect a urinary tract infection in febrile infants presenting to the ED. Am J Emerg Med. 2009;27:930–932.
37 Bonsu BK, Chb M, Harper MB. Identifying febrile young infants with bacteremia: is the peripheral white blood cell count an accurate screen? Ann Emerg Med. 2003;42:216–225.
38 Bonsu BK, Harper MB. Utility of the peripheral blood white blood cell count for identifying sick young infants who need lumbar puncture. Ann Emerg Med. 2003;41:206–214.
39 Taylor JA, Del Beccaro M, Done S, et al. Establishing clinically relevant standards for tachypnea in febrile children younger than 2 years. Arch Pediatr Adolesc Med. 1995;149:283–287.
40 Petersen-Smith A, Barber N, Coody D, et al. Comparison of aural infrared with traditional rectal temperatures in children from birth to age three years. J Pediatr. 1994;125:83–85.
41 Bachur R, Perry H, Harper MB. Occult pneumonias: empiric chest radiographs in febrile children with leukocytosis. Ann Emerg Med. 1999;33:166–173.
42 McCarthy PL, Spiesel SZ, Stashwick CA, et al. Radiographic findings and etiologic diagnosis in ambulatory childhood pneumonias. Clin Pediatr (Phila). 1981;20:686–691.
43 Davies HD, Wang EE, Manson D, et al. Reliability of the chest radiograph in the diagnosis of lower respiratory infections in young children. Pediatr Infect Dis J. 1996;15:600–604.
44 Kramer MS, Roberts-Brauer R, Williams RL. Bias and “overcall” in interpreting chest radiographs in young febrile children. Pediatrics. 1992;90:11–13.