Chapter 216 Cervical Spine Fusion
Allograft versus Autograft
Argument for Allograft
Ventral approaches to the cervical spine were first introduced in the 1950s by Smith and Robinson,1 Cloward,2 and Bailey and Bagley.3 Early surgical techniques used autologous bone grafts. The longevity of these procedures is a testament to their efficacy. However, the use of autologous bone graft is unavoidably coupled with donor site morbidity. In an attempt to eliminate donor site morbidity, the use of allograft was proposed as early as the late 1950s. Since that time, allograft has been used in spinal fusions and has met with varying degrees of success. Allograft provides a comparable means to autograft by which to obtain spinal fusion while eliminating donor site morbidity.
Review of the literature reveals that allograft provides fusion rates and clinical outcomes similar to those obtained by autograft for single-level interbody cervical fusions.4–10 Multilevel interbody fusions are associated with increased nonunion rates and graft complication with both autograft and allograft.4,5,10,11 Nonunion rates and graft complications have been shown to increase with the number of motion segments fused with both autograft and allograft. 4,5,10,11
Various modifications in surgical technique and the use of rigid external fixation, dorsal cervical instrumentation, and, most recently, ventral cervical instrumentation have been tried in an attempt to improve fusion rates for multilevel interbody cervical fusions. The use of ventral cervical instrumentation as an adjunct to multilevel interbody cervical fusions has been shown to increase fusion rates, improve clinical outcomes, and reduce graft complication.12–15 For multilevel interbody cervical fusions, the combination of allograft supplemented with ventral cervical instrumentation has been shown to provide similar fusion rates and clinical outcomes to those obtained with autograft and ventral cervical instrumentation.12,13,15,16
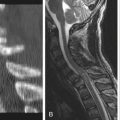
Single-level or multilevel corpectomies are used for the treatment of degenerative, congenital, traumatic, infectious, and neoplastic disorders of the cervical spine. Stabilization of decompressed segments presents spine surgeons with a formidable challenge. Numerous surgical techniques with various types of grafts have been proposed and used with varying degrees of success. As with multilevel interbody cervical fusions, single-level or multilevel corpectomies have an increasing rate of nonunion and graft complications as the number of motion segments fused increases, for both autograft and allograft.5,11 The literature is inconclusive regarding the ideal graft for single-level or multilevel corpectomies. Some authors find autograft to be significantly superior to allograft, with increased fusion rates and decreased graft complications.5,11,17 While other authors have found no difference between allograft and autograft, they have observed an increased time to incorporation of the graft.6,18,19
Modifications in surgical techniques and the use of rigid external fixation, dorsal cervical instrumentation, and, most recently, ventral cervical instrumentation have been used in an attempt to improve fusion rates in single- or multilevel corpectomies. The addition of ventral cervical instrumentation provides immediate cervical spine stability, improves fusion rates, and limits graft complications.12–1620
Various authors have found no difference in fusion rates, clinical outcome, and graft complications when comparing allograft and autograft supplemented with ventral cervical instrumentation for single-level and multilevel corpectomies.16,20,21 Most recently, Mahr et al.21 reported radiographic stability in 99.2% of their patients who underwent cervical corpectomies with fibular allograft reconstruction and ventral cervical instrumentation.
Allograft eliminates harvest site morbidity. Donor site morbidity has been reported to range from 9% to 29%.2,13,15,16,18,20,21 Harvest site complications include wound hematomas, osteomyelitis, wound infections, lateral femoral cutaneous nerve neurapraxia, fractures of the anterior superior iliac spine, and bowel perforations.13,17,22 In a study by Rawlinson,22 36% of patients had persistent donor site pain at 1 year after graft harvest. Rawlinson reported that in 45% of the patients in his study, “donor site pain had delayed their mobilization.”17 Thirty-one percent of patients in his study felt that they could have gone home sooner if not for donor site pain.16 Other advantages of allograft include decreased operative time and blood loss.9,15,16,20,21
Allograft carries the potential for transmission of infectious diseases. However, the risk of acquiring HIV infection from allograft has been estimated to be between one in 1 million and one in 1.6 million.16,21 Strict regulations regarding the testing, harvesting, treatment, handling, and storage of allograft should serve to minimize the risk of acquiring infectious disease via the implantation of allograft.
Finally, the cost of bone graft harvest has been shown to be similar to the cost of purchasing allograft and ventral cervical instrumentation.23
An H.S., Simpson J.M., Glover J.M., Stephany J. Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion. Spine (Phila Pa 1976). 1995;20:2211-2216.
Cloward R. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602-617.
Grossman W., Peppleman W.C., Baun J.A., Kraus D.R. The use of freeze-dried fibular allograft in anterior cervical fusion. Spine (Phila Pa 1976). 1992;17:565-569.
Young W.F., Rosenwasser R.H. An early comparative analysis of the use of fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine (Phila Pa 1976). 1993;18(9):1123-1124.
Zdeblick T.A., Ducker T.B. The use of freeze-dried allograft for anterior cervical fusion. Spine (Phila Pa 1976). 1991;16:726-729.
1. Smith G., Robinson R. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg [Am]. 1957;40:607.
2. Cloward R. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602-617.
3. Bailey R., Badgley C. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg [Am]. 1960;42:565-594.
4. An H.S., Simpson J.M., Glover J.M., Stephany J. Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion. Spine (Phila Pa 1976). 1995;20:2211-2216.
5. Butterman G.R., Glazer P.A., Bradford D.S. The use of bone allograft in the spine. Clin Orthop Relat Res. 1989;324:75-85.
6. Grossman W., Peppleman W.C., Baun J.A., Kraus D.R. The use of freeze-dried fibular allograft in anterior cervical fusion. Spine (Phila Pa 1976). 1992;17:565-569.
7. Rish B.L., McFadden J.T., Penix J.O. Anterior cervical fusion using homologous bone grafts: a comparative study. Surg Neurol. 1976;76:119-121.
8. Savolainen S., Vsenius J.P., Hernesnicmi J. Iliac crest versus artificial bone graft in 250 cervical fusions. Acta Neurochir. 1994;131:54-57.
9. Young W.F., Rosenwasser R.H. An early comparative analysis of the use of fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine. 1993;18(9):1123-1124.
10. Zdeblick T.A., Ducker T.B. The use of freeze-dried allograft for anterior cervical fusion. Spine. 1991;16:726-729.
11. Fernyhough J.C., White J.I., LaRocca H. Fusion rates in multi-level spondylosis comparing allograft fibula with autograft fibula in 126 patients. Spine (Phila Pa 1976). 1991;16:726-729.
12. Coric D., Brunch C.L.Jr., Jenkins J.D. Revision of anterior cervical pseudoarthrosis with anterior allograft fusion and plating. J Neurosurg. 1997;86:969-974.
13. Geisler F.H., Caspar W., Pitzen T., Johnson T.A. Reoperation in patients after anterior cervical plate stabilization in degenerative disease. Spine (Phila Pa 1976). 1998;23(8):911-920.
14. Johnston F.G., Crockard H.A. One-stage internal fixation and anterior fusion in complex cervical spinal disorders. J Neurosurg. 1995;82:234-238.
15. Shapiro S. Banked fibula and locking anterior cervical plate in anterior cervical fusions following cervical discectomy. J Neurosurg. 1996;84:161-165.
16. Eleraky M.A., Llanos C., Sonntag V.K. Cervical corpectomy: report of 185 cases and review of the literature. J Neurosurg. 1999;90:35-41.
17. Zdeblick T.A., Bohlman H.H. Cervical kyphosis and myelopathy. Treatment by anterior corpectomy and strut-grafting. J Bone Joint Surg [Am]. 1989;71:170-182.
18. Harsh G.R.4th, Sypert G.W., Weinstein P.R., et al. Cervical spine stenosis secondary to ossification of the posterior longitudinal ligament. J Neurosurg. 1987;67:849-857.
19. MacDonald R.L., Fehlings M.F., Tater C.H., et al. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg. 1997;86:990-997.
20. Hermann J.M., Sonntag V.K.H. Cervical corpectomy and plate fixation for postlaminectomy kyphosis. J Neurosurg. 1994;80:963-970.
21. Mayr M.T., Subach B., Comey C.H., et al. Cervical spinal stenosis: outcome after anterior corpectomy, allograft reconstruction, and instrumentation. J Neurosurg. 2002;96(Suppl 1):10-16.
22. Rawlinson J.N. Morbidity after anterior cervical decompression and fusion. The influence of the donor site in recovery and the result of a trial of surgical bone compared to autologous bone. Acta Neurochir. 1994;131:106-118.
23. Hadley M.N. Banked fibula and anterior cervical locking plate [letter]. J Neurosurg. 1996;85:736-773.
Argument for Autograft
Multiple studies have directly compared autograft to allograft. In 1990, Zdeblick and Ducker1 compared allograft and autograft retrospectively for single-level and multilevel anterior cervical discectomy and fusion (ACDF) without a plate. The fusion rate for single-level fusion was 95% for both substrates; however, the fusion rate for two-level ACDF with autograft was 83%, compared with a dismal 37% for allograft. Pooling all patients in this study, the overall fusion rates for autograft and allograft were 92% and 78%, respectively. In a similar, but larger, study, Bishop et al. 2 evaluated 132 patients who had undergone single-level or multilevel ACDF with either autograft or allograft without a plate. Allograft again was found to be inferior to autograft in terms of fusion for both single-level fusion (87% vs. 97%) and multilevel fusion (53% vs. 87%). In another retrospective study, Samartzis et al.3 compared allograft with autograft for single-level and multilevel ACDF with plate in 80 patients, and like the previous authors, reported fusion rates in favor of autogenous bone, 100% versus 94%. Suchomel et al.4 prospectively evaluated 79 patients who underwent single-level or multilevel ACDF with a plate. The fusion rates for either one- or two-level surgery were not found to be different statistically; however, the authors concluded that fusion takes longer with allograft bone.
Several case series have evaluated fusion with either allograft or autograft with a plate. Kostuik et al.5 reported 100% fusion rates for single-level ACDF with a plate and autograft in 42 patients. Similarly, Connolly et al.6 reported 100% fusion rates for the same surgery in 43 patients following single-level or multilevel ACDF. Fusion rates of 100% also were reported by Schneeberger et al.7 for one-, two-, or three-level ACDF with plate and autograft. Wang et al.8 reported a 100% success rate for two-level ACDF with autograft and a plate. Wang et al.9 also reported a fusion rate of 82% for three-level ACDF with plate and autograft, in contrast to the 71% fusion rate for a three-level ACDF with plate and allograft reported by Yue et al.10 In a large retrospective series of one- and two-level ACDF with plate and allograft, Martin et al.11 reported fusion rates of 90% and 72%, respectively.
To be fair, single-level fusion using allograft bone and a plate has been shown to result in reasonable rates of fusion. The highest level of evidence available for the use of allograft bone for single-level ACDF with a plate comes from the cervical disc arthroplasty investigational device exemption (IDE) trials. The control arm in the Prestige IDE trial as reported by Mummeneni et al.12 had a fusion rate of 98.7%. The fusion rate for single-level fusion with allograft and a plate in the Prodisc-C trial was reported to be 90.2%,13 and in the Bryan Disc IDE trial, the fusion rate was 94.3%.14 Although allograft bone may result in sufficient fusion rates for instrumented single-level fusions, several studies have demonstrated that allograft bone is not the ideal substrate for the more biologically challenging multilevel ACDF.1,2,10,11
The main criteria for success following ventral cervical fusion are ample neurologic decompression and successful fusion. Nonunion has been associated with suboptimal clinical outcomes in multiple studies. Phillips et al.15 evaluated 48 patients with known pseudarthrosis following ventral cervical fusion surgery. Thirty-two patients (67%) were symptomatic, with either neck pain and/or radiculopathy, and 22 patients (45%) required secondary surgery due to the nonunion. Similarly, poor outcomes were reported by Wright and Eisenstein.16 In their series, 18 patients developed pseudarthrosis, and 9 of them (50%) required secondary surgeries. Furthermore, only 60% of the patients who had revision surgeries improved clinically. Nonunion was found to be associated with inadequate outcomes in yet another study by Kuhns et al.17 In that study, 33 patients were treated with dorsal fusion following failed ventral fusion; follow-up was assessed by the Cervical Spine Outcomes Questionnaire, SF-36, and Arthritis Impact Measurement Scale 2. Although all patients achieved fusion following dorsal revision fusion, 20% of the patients reported “discomforting” pain, and 28% of the patients continued to have “moderate to severe” pain. Clearly, the need to achieve fusion cannot be overemphasized.
Phillips F.M., Carlson G., Emery S.E., Bohlman H.H. Anterior cervical pseudarthrosis. Natural history and treatment. Spine (Phila Pa 1976). 1997;22(14):1585-1589.
Samartzis D., Shen F.H., Matthews D.K., et al. Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J. 2003;3(6):451-459.
Wang J.C., McDonough P.W., Endow K.K., Delamarter R.B. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2000;25(1):41-45.
Wang J.C., McDonough P.W., Kanim L.E., et al. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2001;26(6):643-646.
Yue W.M., Brodner W., Highland T.R. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976). 2005;30(19):2138-2144.
1. Zdeblick T.A., Ducker T.B. The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976). 1991;16(7):726-729.
2. Bishop R.C., Moore K.A., Hadley M.N. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. J Neurosurg. 1996;85(2):206-210.
3. Samartzis D., Shen F.H., Matthews D.K., et al. Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J. 2003;3(6):451-459.
4. Suchomel P., Barsa P., Buchvald P., et al. Autologous versus allogenic bone grafts in instrumented anterior cervical discectomy and fusion: a prospective study with respect to bone union pattern. Eur Spine J. 2004;13(6):510-515.
5. Kostuik J.P., Connolly P.J., Esses S.I., Suh P. Anterior cervical plate fixation with the titanium hollow screw plate system. Spine (Phila Pa 1976). 1993;18(10):1273-1278.
6. Connolly P.J., Esses S.I., Kostuik J.P. Anterior cervical fusion: outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord. 1996;9(3):202-206.
7. Schneeberger A.G., Boos N., Schwarzenbach O., Aebi M. Anterior cervical interbody fusion with plate fixation for chronic spondylotic radiculopathy: a 2- to 8-year follow-up. J Spinal Disord. 1999;12(3):215-220.
8. Wang J.C., McDonough P.W., Endow K.K., Delamarter R.B. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2000;25(1):41-45.
9. Wang J.C., McDonough P.W., Kanim L.E., et al. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2001;26(6):643-646.
10. Yue W.M., Brodner W., Highland T.R. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976). 2005;30(19):2138-2144.
11. Martin G.J.Jr., Haid R.W.Jr., MacMillan M., et al. Anterior cervical discectomy with freeze-dried fibula allograft. Overview of 317 cases and literature review. Spine (Phila Pa 1976). 1999;24(9):852-858.
12. Mummaneni P.V., Burkus J.K., Haid R.W., et al. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007;6(3):198-209.
13. Murrey D., Janssen M., Delamarter R., et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9(4):275-286.
14. Heller J.G., Sasso R.C., Papadopoulos S.M., et al. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976). 2009;34(2):101-107.
15. Phillips F.M., Carlson G., Emery S.E., Bohlman H.H. Anterior cervical pseudarthrosis. Natural history and treatment. Spine (Phila Pa 1976). 1997;22(14):1585-1589.
16. Wright I.P., Eisenstein S.M. Anterior cervical discectomy and fusion without instrumentation. Spine (Phila Pa 1976). 2007;32(7):772-774.
17. Kuhns C.A., Geck M.J., Wang J.C., Delamarter R.B. An outcomes analysis of the treatment of cervical pseudarthrosis with posterior fusion. Spine (Phila Pa 1976). 2005;30(21):2424-2429.