Cervical Spine
Examination of the cervical spine involves determining whether the injury or pathology occurs in the cervical spine or in a portion of the upper limb. Cyriax1 called this assessment the scanning examination. In the initial assessment of a patient who complains of pain in the neck and/or upper limb, this procedure is always carried out unless the examiner is absolutely sure of the location of the lesion. If the injury is in the neck, the scanning examination is definitely called for to rule out neurological involvement. After the lesion site has been determined, a more detailed assessment of the affected area is performed if it is outside the cervical spine.
Because many conditions affecting the cervical spine can be manifested in other parts of the body, the cervical spine is a complicated area to assess properly, and adequate time must be allowed to ensure that as many causes or problems are examined as possible.
Applied Anatomy
The cervical spine consists of several pairs of joints. It is an area in which stability has been sacrificed for mobility, making the cervical spine particularly vulnerable to injury because it sits between a heavy head and a stable thoracic spine and ribs. The cervical spine is divided into two areas—the cervicoencephalic for the upper cervical spine and the cervicobrachial for the lower cervical spine. The cervicoencephalic or cervicocranial region (C0 to C2) shows the relationship between the cervical spine and the occiput, and injuries in this region have the potential of involving the brain, brainstem, and spinal cord (Figure 3-1).2,3 Injuries in this area lead to symptoms of headache, fatigue, vertigo, poor concentration, hypertonia of sympathetic nervous system, and irritability. In addition, there may be cognitive dysfunction, cranial nerve dysfunction, and sympathetic system dysfunction.2,3
The atlanto-occipital joints (C0 to C1) are the two uppermost joints. The principal motion of these two joints is flexion-extension (15° to 20°), or nodding of the head. Side flexion is approximately 10°, whereas rotation is negligible. The atlas (C1) has no vertebral body as such. During development, the vertebral body of C1 evolves into the odontoid process, which is part of C2. The atlanto-occipital joints are ellipsoid and act in unison. Along with the atlanto-axial joints, these joints are the most complex articulations of the axial skeleton.
There are several ligaments that stabilize the atlanto-occipital joints. Anteriorly and posteriorly are the atlanto-occipital membranes. The anterior membrane is strengthened by the anterior longitudinal ligament. The posterior membrane replaces the ligamentum flavum between the atlas and occiput. The tectorial membrane, which is a broad band covering the dens and its ligaments, is found within the vertebral canal and is a continuation of the posterior longitudinal ligament. The alar ligaments are two strong rounded cords found on each side of the upper dens passing upwards and laterally to attach on the medial sides of the occipital condyles. The alar ligaments limit flexion and rotation and play a major role in stabilizing C1 and C2, especially in rotation.4
The atlanto-axial joints (C1 to C2) constitute the most mobile articulations of the spine. Flexion-extension is approximately 10°, and side flexion is approximately 5°. Rotation, which is approximately 50°, is the primary movement of these joints. With rotation, there is a decrease in height of the cervical spine at this level as the vertebrae approximate because of the shape of the facet joints. The odontoid process of C2 acts as a pivot point for the rotation. This middle, or median, joint is classified as a pivot (trochoidal) joint. The lateral atlanto-axial, or facet, joints are classified as plane joints. Generally, if a person can talk and chew, there is probably some motion occurring at C1 to C2. At the atlanto-axial joints, the main supporting ligament is the transverse ligament of the atlas, which holds the dens of the axis against the anterior arch of the atlas. It is this ligament that weakens or ruptures in rheumatoid arthritis. As the ligament crosses the dens, there are two projections off the ligament, one going superiorly to the occiput and one inferiorly to the axis. The ligament and the projections form a cross, and the three parts taken together are called the cruciform ligament of the atlas (Figure 3-2).
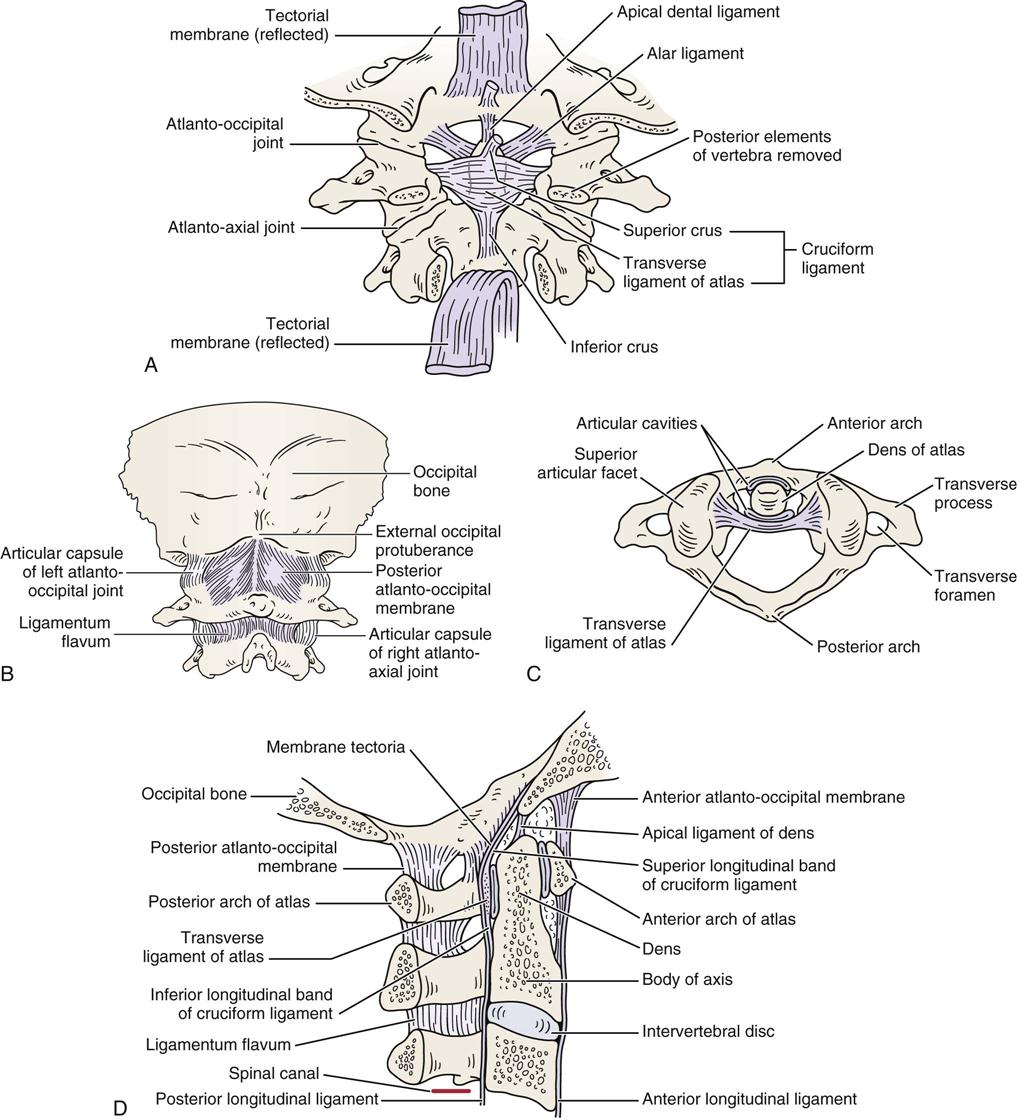
A, Posterior deep view. B, Posterior superficial view. C, Superior view. D, Lateral view.
The vertebral artery—part of the vertebrobasilar system that passes through the transverse processes of the cervical vertebrae usually starting at C6 but entering as high as C4—supplies 20% of the blood supply to the brain (primarily the hindbrain) along with the internal carotid artery (80%) (Figure 3-3).5,6 In its path, the vertebral artery lies close to the facet joints and vertebral body where it may be compressed by osteophyte formation or injury to the facet joint. In addition, in older individuals, atherosclerotic changes and other vascular risk factors (e.g., hypertension, high fat or cholesterol levels, diabetes, smoking) may contribute to altered blood flow in the arteries.7 The vertebral and internal carotid arteries are stressed primarily by rotation, extension, and traction movements, but other movements may also stretch the artery.8–10 Rotation and extension of as little as 20° have been shown to significantly decrease vertebral artery blood flow.11,12 The greatest stresses are placed on the vertebral arteries in four places: where it enters the transverse process of C6, within the bony canals of the vertebral transverse processes, between C1 and C2, and between C1 and the entry of the arteries into the skull.13,14 These latter two areas have the greatest potential for problems (e.g., thrombosis, dissection, stroke) related to treatment and their concomitant stress on the vertebral arteries.15 Dutton13 reports that the most common mechanism for non-penetrating injury to the vertebral artery is neck extension, with or without side flexion or rotation.16,17 Given the type of injury possible, symptoms may be delayed.18,19 Symptoms related to the vertebral artery include vertigo, nausea, tinnitus, “drop attacks” (falling without fainting), visual disturbances, or, in rare cases, stroke or death.
The lower cervical spine (C3 to C7) is called the cervicobrachial area, since pain in this area is commonly referred into the upper extremity.2,3 Pathology in this region leads to neck pain alone, arm pain alone, or both neck and arm pain. Thus, symptoms include neck and/or arm pain, headaches, restricted range of motion (ROM), paresthesia, altered myotomes and dermatomes, and radicular signs. Cognitive dysfunction and cranial nerve dysfunction are not commonly symptoms of injuries in this area although sympathetic dysfunction may be. Injury to both areas, if severe enough, may result in psychosocial issues.
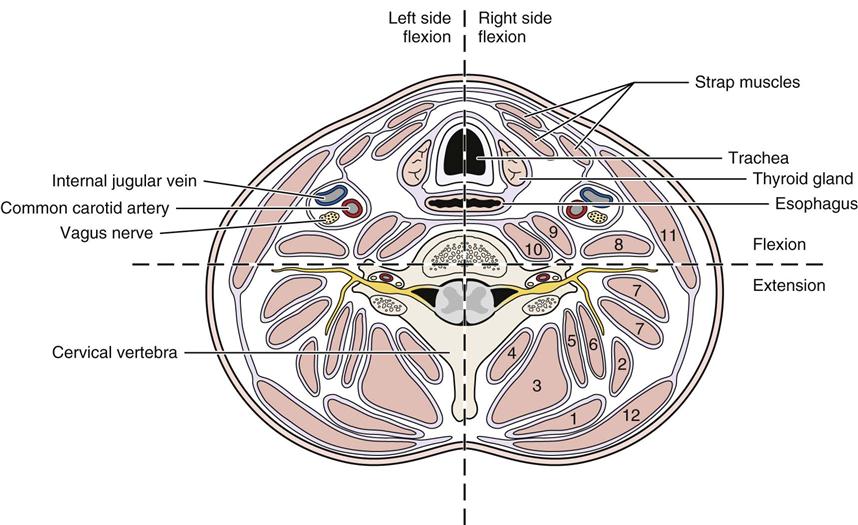
There are 14 facet (apophyseal) joints in the cervical spine (C1 to C7). The upper four facet joints in the two upper thoracic vertebrae (T1 to T2) are often included in the examination of the cervical spine. The superior facets of the cervical spine face upward, backward, and medially; the inferior facets face downward, forward, and laterally (Figure 3-4). This plane facilitates flexion and extension, but it prevents simple rotation or side flexion without both occurring to some degree together. This is called a coupled movement with rotation and side flexion both occurring with either movement.20 Ishii et al.21,22 reported that between C0 and C2, as well as C7 and T1, the two movements occur in opposite directions while between C2 and C7, they occur in the same direction. These joints move primarily by gliding and are classified as synovial (diarthrodial) joints. The capsules are lax to allow sufficient movement. At the same time, they provide support and a check-rein type of restriction at end range. The greatest flexion-extension of the facet joints occurs between C5 and C6; however, there is almost as much movement at C4 to C5 and C6 to C7. Because of this mobility, degeneration is more likely to be seen at these levels. The neutral or resting position of the cervical spine is slightly extended. The close packed position of the facet joints is complete extension.
The recurrent meningeal, or sinuvertebral, nerve innervates the anterior dura sac, the posterior annulus fibrosus, and the posterior longitudinal ligament. The facet joints are innervated by the medial branch of the dorsal primary rami.23 For C3 to C7, the main ligaments are the anterior longitudinal ligament, the posterior longitudinal ligament, the ligamentum flavum, and the supraspinal and interspinal ligaments (Figure 3-5). There are also ligaments between the transverse processes (intertransverse ligaments), but in the cervical spine, they are rudimentary.
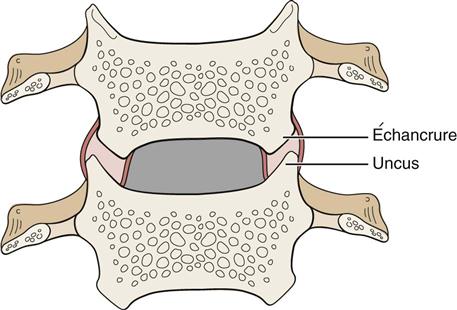
Some anatomists24–27 refer to the costal or uncovertebral processes as uncinate joints or joints of Luschka (Figure 3-6). These structures were described by von Luschka in 1858. The uncus gives a “saddle” form to the upper aspect of the cervical vertebra, which is more pronounced posterolaterally; it has the effect of limiting side flexion. Extending from the uncus is a “joint” that appears to form because of a weakness in the annulus fibrosus. The portion of the vertebra above, which “articulates” or conforms to the uncus, is called the échancrure, or notch. Notches are found from C3 to T1, but according to most authors,24–27 they are not seen until age 6 to 9 years and are not fully developed until 18 years of age. There is some controversy as to whether they should be classified as real joints because some authors believe they are the result of degeneration of the intervertebral disc.
The intervertebral discs make up approximately 25% of the height of the cervical spine. No disc is found between the atlas and the occiput (C0 to C1) or between the atlas and the axis (C1 to C2). It is the discs rather than the vertebrae that give the cervical spine its lordotic shape (Figure 3-7). The nucleus pulposus functions as a buffer to axial compression in distributing compressive forces, whereas the annulus fibrosus acts to withstand tension within the disc. The intervertebral disc has some innervation on the periphery of the annulus fibrosus.28,29
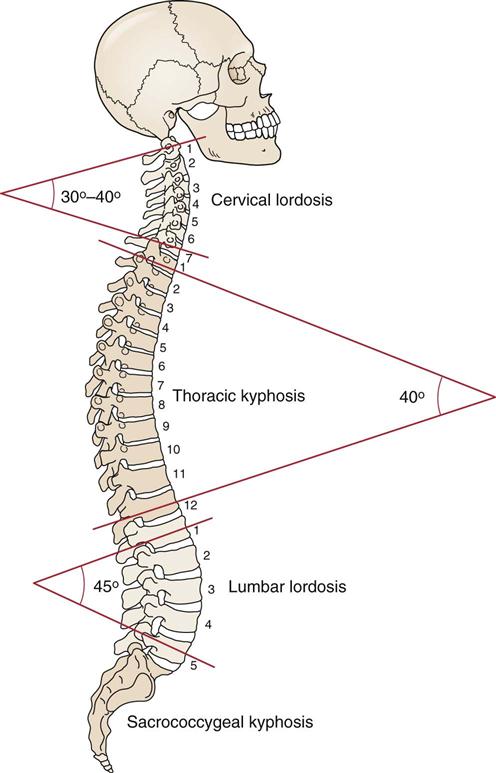
The curvatures represent the normal resting postures of the region. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 276.)
There are seven vertebrae in the cervical spine with the body of each vertebra (except C1) supporting the weight of those above it. The facet joints may bear some of the weight of the vertebrae above, but this weight is minimal if the normal lordotic posture is maintained. However, even this slight amount of weight bearing can lead to spondylitic changes in these joints. The outer ring of the vertebral body is made of cortical bone, and the inner part is made of cancellous bone covered with the cartilaginous end plate. The vertebral arch protects the spinal cord, while the spinous processes, most of which are bifid in the cervical spine, provide for attachment of muscles. The transverse processes have basically the same function. In the cervical spine, the transverse processes are made up of two parts: the anterior portion that provides the foramen for the vertebral body, and the posterior portion containing the two articular facets (see Figure 3-4, B). In the cervical spine, the spinous processes are at the level of the facet joints of the same vertebra. Generally, the spinous process is considered to be absent or at least rudimentary on C1. This is why the first palpable vertebra descending from the external occiput protuberance is the spinous process of C2.
Although there are seven cervical vertebrae, there are eight cervical nerve roots. This difference occurs because there is a nerve root exiting between the occiput and C1 that is designated the C1 nerve root. In the cervical spine, each nerve root is named for the vertebra below it. As an example, C5 nerve root exists between the C4 and C5 vertebrae (Figure 3-8). In the rest of the spine, each nerve root is named for the vertebra above; the L4 nerve root, for example, exists between the L4 and L5 vertebrae. The switch in naming of the nerve roots from the one below to the one above is made between the C7 and T1 vertebrae. The nerve root between these two vertebrae is called C8, accounting for the fact that there are eight cervical nerve roots and only seven cervical vertebrae.
Patient History
In addition to the questions listed under Patient History in Chapter 1, the examiner should obtain the following information from the patient:
1. What is the patient’s age? Spondylosis (also called spondylosis deformans) is often seen in persons 25 years of age or older, and it is present in 60% of those older than 45 years and 85% of those older than 65 years of age.30,31 It is a generalized disease of aging initiated by intervertebral disc degeneration. Symptoms of osteoarthritis do not usually appear until a person is 60 years of age or older (Table 3-1).
2. What are the symptoms, and which are most severe? Table 3-2 outlines many of the signs and symptoms that may arise from cervical spine pathology.32 Where are the symptoms most severe—in the neck, the shoulder, above or below the elbow, in the hands, and/or fingers?33 Location of the symptoms may help determine what level of the cervical spine is involved (e.g., tingling in the middle finger may indicate a problem at C6 to C7). Are the symptoms constant, intermittent or variable?33 The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and its Associated Disorders recommended that neck pain sufferers be divided into four groups (Table 3-3).34
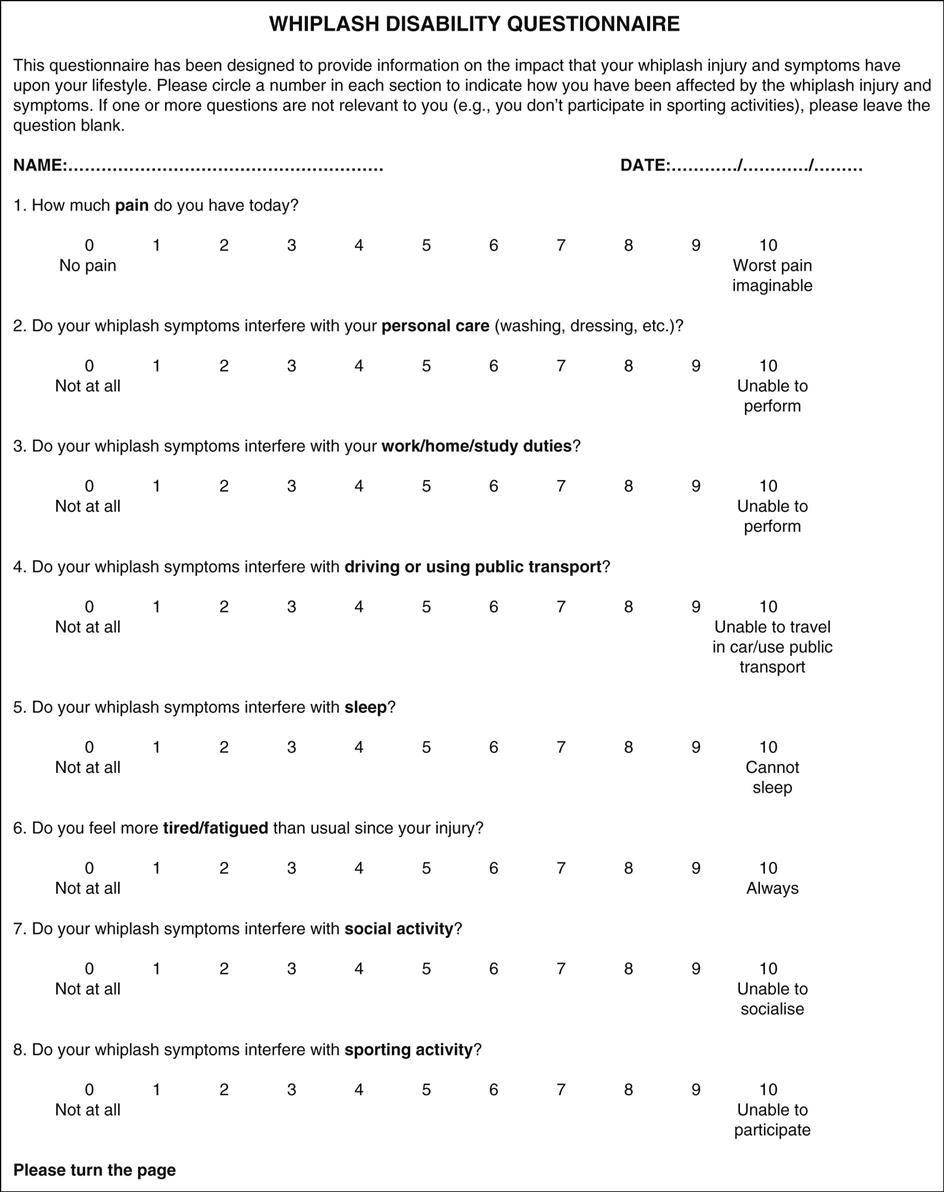
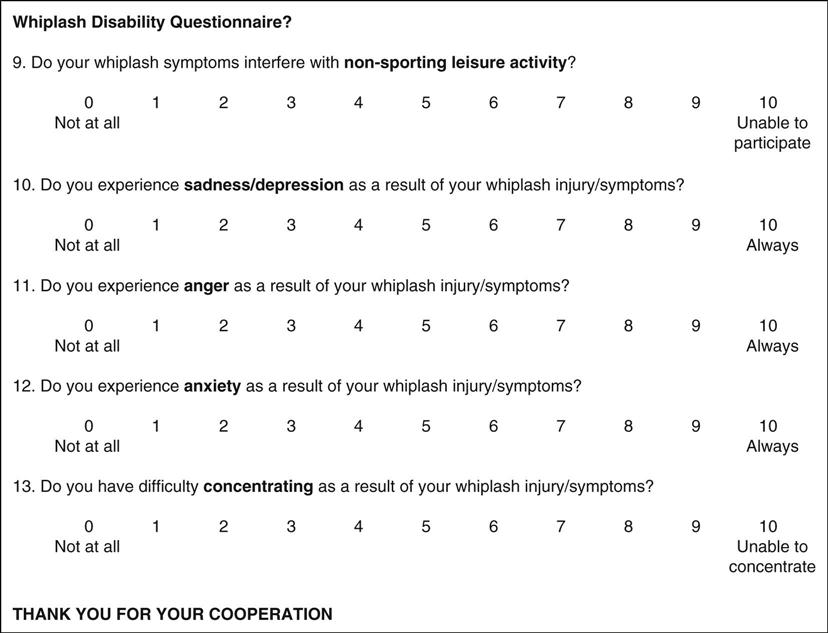
Watkins35 provided a severity scale for neurological injury in football that can be used as a guideline for injury severity involving the cervical spine, especially if one is contemplating allowing the patient to return to activity (Figure 3-9 ). A combined score (A+B) of 4 is considered a mild episode, 4 to 7 is a moderate episode, and 8 to 10 is a severe episode. This scale can be combined with radiologic information on canal size (score C) to give a general determination of the possibility of symptoms returning if the patient returns to activity. In this case, a score of 6 (A+B+C) indicates minimum risk, 6 to 10 is moderate risk, and 10 to 15 is severe risk. Watkins35 also points out that extenuating factors (such as, age of patient, level of activity, and risk) versus benefit, also play a role and, although not included in the score, must be considered. Table 3-4 outlines some of the factors that increase the chances of recovery from neck pain. Chronic post whiplash syndrome can lead to anxiety, pain catastrophizing (negative or heightened orientation toward pain), and other adverse psychosocial factors over time, and it can play a major role in the symptoms felt by the patient.36 Table 3-5 outlines yellow flags related to fear-avoidance beliefs.
3. What was the mechanism of injury? Was trauma, stretching, or overuse involved? Was the patient moving when the injury occurred? Table 3-6 outlines warning signs and symptoms (red flags) of serious cervical spine disorders. These questions help determine the type and severity of injury. For example, trauma may cause a whiplash-type (acceleration) injury or whiplash associated disorder (WAD) (Table 3-7),37 stretching may lead to “burners,” overuse or sustained postures may result in thoracic outlet symptoms, and a report of an insidious onset in someone older than 55 years of age may indicate cervical spondylosis. Was the patient hit from the side, front, or behind? Did the patient see the accident coming?38 “Burners” or “stingers” typically occur from a blow to part of the brachial plexus or from stretching or compression of the brachial plexus (Table 3-8; Figure 3-10). The answers to these questions help the examiner determine how the injury occurred, the tissues injured, and the severity of the injuries.
4. Has the patient had neck pain before? Table 3-9 outlines factors that decrease chances of a new episode of neck pain.34
5. What is the patient’s usual activity or pastime? Do any particular activities or postures bother the patient? What type of work does the patient do? Are there any positions that the patient holds for long periods (e.g., when sewing, typing, or working at a desk)? Does the patient wear glasses? If so, are they bifocals or trifocals? Upper cervical symptoms may result from excessive nodding as the patient tries to focus through the correct part of the glasses. Cervicothoracic (lower cervical/upper thoracic spine) joint problems are often painful when activities that require push-and-pull motion (such as, lawn mowing, sawing, and cleaning windows) are performed. What movements bother the patient? For example, extension can aggravate symptoms in patients with radicular signs and symptoms.39
6. Did the head strike anything, or did the patient lose consciousness? If the injury was caused by a motor vehicle accident, it is important to know whether the patient was wearing a seat belt, the type of seat belt (lap or shoulder), and whether the patient saw the accident coming. These questions give some idea of the severity and mechanisms of injury. If the patient was unconscious or unsteady, the character of each episode of altered consciousness should be noted (see Chapter 2).
7. Did the symptoms come on right away? Bone pain usually occurs immediately, but muscle or ligamentous pain can either come on immediately (e.g., a tear) or occur several hours or days later (e.g., stretching caused by a motor vehicle accident). Seventy percent of whiplash patients reported immediate symptom occurrence while the rest reported delayed symptoms.32,40–44 How long have the symptoms been present? Myofascial pain syndromes demonstrate generalized aching and at least three trigger points, which have lasted for at least 3 months with no history of trauma.45
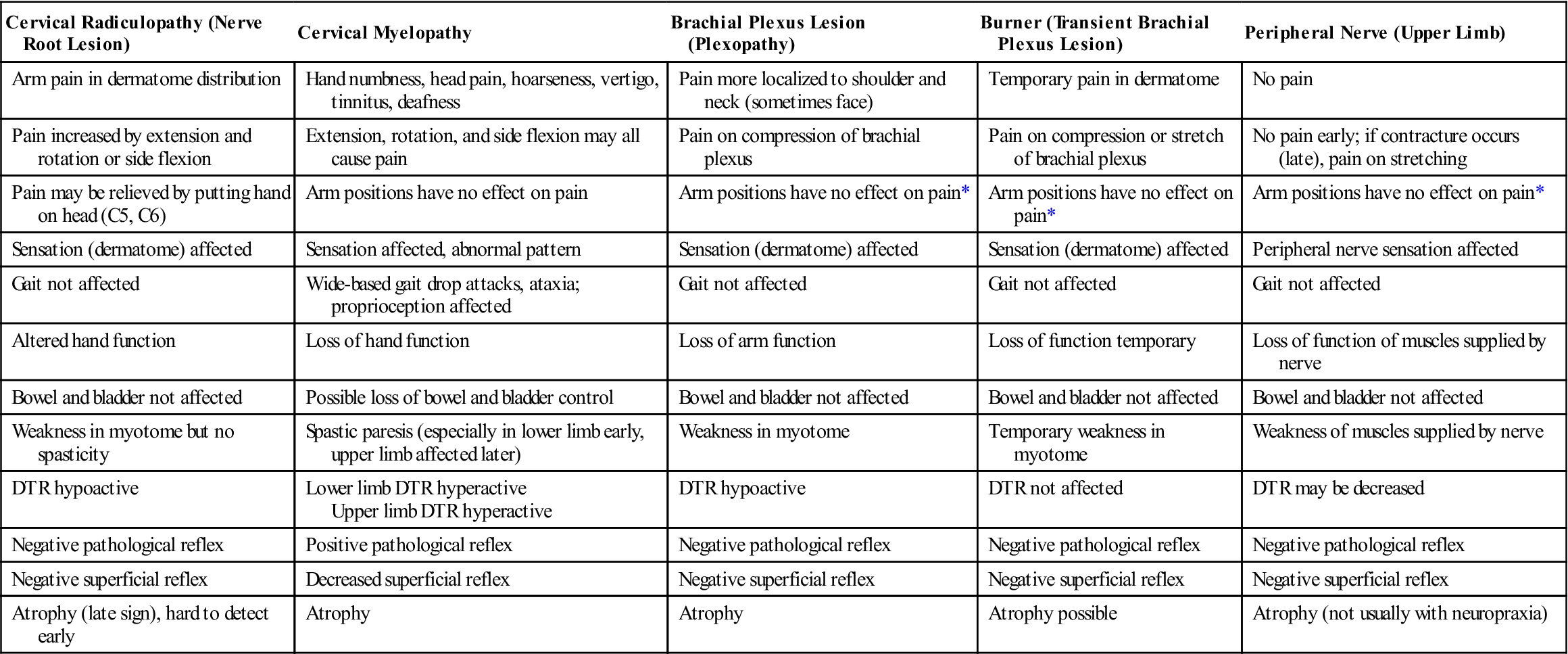
8. What are the sites and boundaries of the pain? Have the patient point to the location or locations of the pain. Symptoms do not go down the arm for a C4 nerve root injury or for nerve roots above that level. Cervical radiculopathy, or injury to the nerve roots in the cervical spine, presents primarily with unilateral motor and sensory symptoms into the upper limb, with muscle weakness (myotome), sensory alteration (dermatome), reflex hypoactivity, and sometimes focal activity being the primary signs.46–49 Acute radiculopathies are commonly associated with disc herniations, whereas chronic types are more related to spondylosis.47 Disc herniations in the cervical spine commonly cause severe neck pain that may radiate into the shoulder, scapula and/or arm, limit ROM, and an increase in pain on coughing, sneezing, jarring, or straining.44 Cervical myelopathy, or injury to the spinal cord itself, is more likely to present with spastic weakness, paresthesia, and possible incoordination in one or both lower limbs, as well as proprioceptive and/or sphincter dysfunction (Tables 3-10 and 3-11).50
9. Is there any radiation of pain? It is helpful to correlate this answer with dermatome and sensory peripheral nerve findings when performing sensation testing and palpation later in the examination. Is the pain deep, superficial, shooting, burning, or aching? For example, when an athlete experiences a “burner,” the sensation is a lightning-like, burning pain into the shoulder and arm, followed by a period of heaviness or loss of function in the arm. Figure 3-11 shows the radiation of pain with facet (apophyseal) joint pathology.51
11. Does the patient have any headaches? If so, where? How frequently do they occur? For example, do they occur every day, two times per day, two days per week, or one day per month?52 How intense are they? How long do they last? Are they affected by medication and, if so, by how much medication, and what kind? Are there any precipitating factors (e.g., food, stress, posture)? See Tables 2-11, 2-12, and 2-13, which indicate the influence of time of day, body position, headache location, and type of pain on diagnosis of the type of headache that the patient may have. Table 2-14 outlines the salient features of some of the more common headaches. Craniovertebral joint dysfunction commonly is accompanied by headaches. For example, C1 headaches occur at the base and top of the head, whereas C2 headaches are referred to the temporal area.
12. Does a position change alter the headache or pain? If so, which positions increase or decrease the pain? The patient may state that the pain and referred symptoms are decreased or relieved by placing the hand or arm of the affected side on top of the head. This is called Bakody’s sign, and it is usually indicative of problems in the C4 or C5 area.53,54
13. Is paresthesia (a “pins and needles” feeling) present? This sensation occurs if pressure is applied to the nerve root. It may become evident if pressure is relieved from a nerve trunk. Numbness and/or paresthesia in the hands or legs and deteriorating hand function all may relate to cervical myelopathy (see Table 3-10).
15. Are there any lower limb symptoms? This finding may indicate a severe problem affecting the spinal cord (myelopathy; see Table 3-10). These symptoms may include numbness, paresthesia, stumbling, difficulty walking, and lack of balance or agility. All of these symptoms could indicate cervical myelopathy. Likewise, signs of sphincter (bowel or bladder) or sexual dysfunction may be related to cervical myelopathy.
16. Does the patient have any difficulty walking? Does the patient have problems with balance? Does the patient stumble when walking, have trouble walking in the dark, or walk with feet wide apart? Positive responses may indicate a cervical myelopathy. Abnormality of the cranial nerves combined with gait alterations may indicate systemic neurological dysfunction.55
17. Does the patient experience dizziness, faintness, or seizures? What is the degree, frequency, and duration of the dizziness? Is it associated with certain head positions or body positions? Semicircular canal problems or vertebral artery problems (Table 3-12) can lead to dizziness. Dizziness from a vertebral artery problem is commonly associated with other symptoms. Falling with no provocation while remaining conscious is sometimes called a drop attack.56 Has the patient experienced any visual disturbances? Disturbances such as diplopia (double vision), nystagmus (“dancing eyes”), scotomas (depressed visual field), and loss of acuity may indicate severity of injury, neurological injury, and sometimes increased intracranial pressure (see Chapter 2).53
18. Does the patient exhibit or complain of any sympathetic symptoms? There may be injury to the cranial nerves or the sympathetic nervous system, which lies in the soft tissues of the neck anterior and lateral to the cervical vertebrae. The cranial nerves and their functions are shown in Table 2-1. Severe injuries (e.g., acceleration/whiplash type) can lead to hypertonia of the sympathetic nervous system.2 Some of the sympathetic signs and symptoms the examiner may elicit are “ringing” in the ears (tinnitus), dizziness, blurred vision, photophobia, rhinorrhea, sweating, lacrimation, and loss of strength.
25. Does the patient display any cognitive dysfunction? If a possible head injury is suspected, the clinician should also consider testing for mental status (see Chapter 2).
TABLE 3-1
Differential Diagnosis of Cervical Spondylosis, Spinal Stenosis, and Disc Herniation
| Cervical Spondylosis | Cervical Spinal Stenosis | Cervical Disc Herniation* | |
| Pain | Unilateral | May be unilateral or bilateral | May be unilateral (most common) or bilateral |
| Distribution of pain | Into affected dermatomes | Usually several dermatomes affected | Into affected dermatomes |
| Pain on extension | Increases | Increases | May increase (most common) |
| Pain on flexion | Decreases | Decreases | May increase or decrease (most common) |
| Pain relieved by rest | No | Yes | No |
| Age group affected | 60% of those older than 45 years 85% of those older than 65 years |
11 to 70 years Most common: 30 to 60 years |
17 to 60 years |
| Instability | Possible | No | No |
| Levels commonly affected | C5–C6, C6–C7 | Varies | C5–C6 |
| Onset | Slow | Slow (may be combined with spondylosis or disc herniation) | Sudden |
| Diagnostic imaging | Diagnostic | Diagnostic | Diagnostic (be sure clinical signs support) |
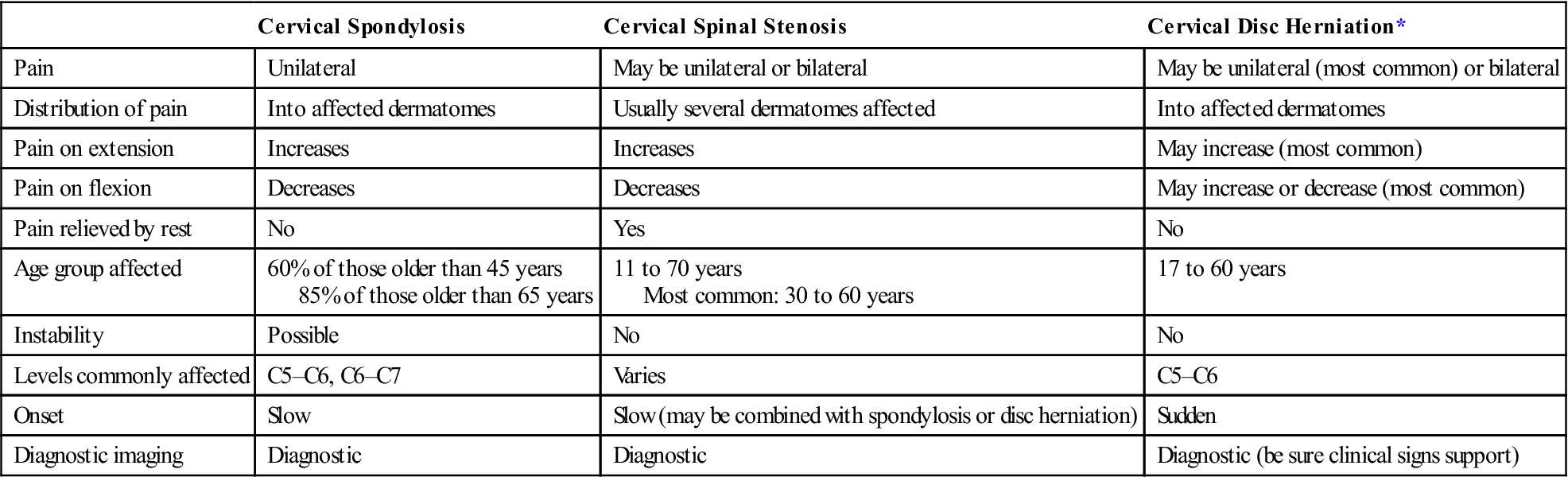
TABLE 3-2
Signs and Symptoms Arising from Cervical Spine Pathology
| Signs | Symptoms |
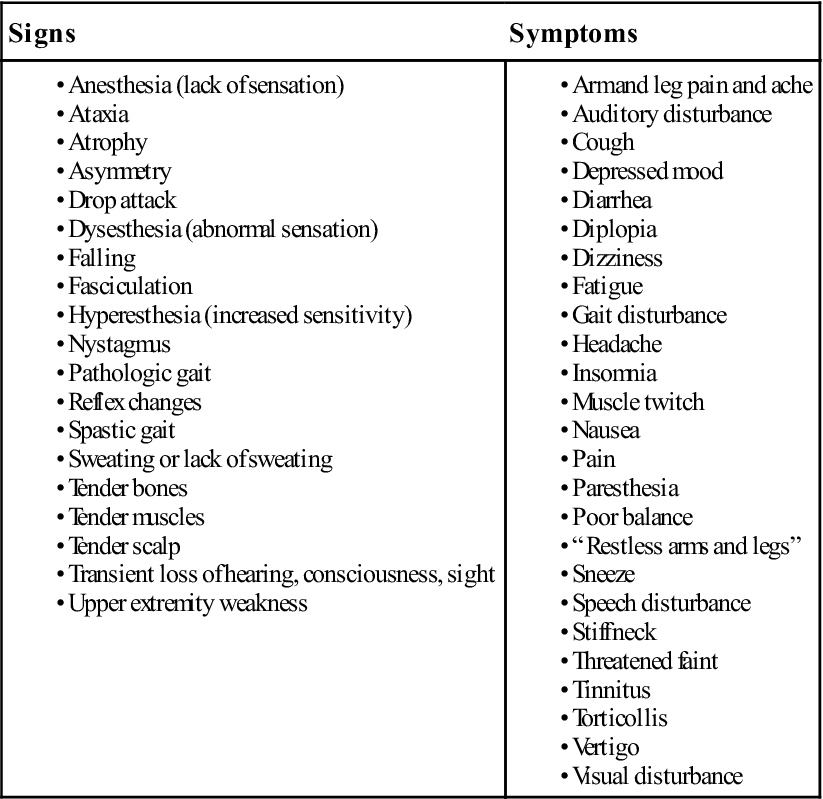
Modified from Bland JH: Disorders of the cervical spine, Philadelphia, 1994, W.B. Saunders Co., p. 161.
TABLE 3-3
Grading of Patients Suffering from Neck Pain
| Grade | Clinical Presentation |
| 1 | No signs of major pathology |
| Little or no interference with daily activity (ADL) | |
| 2 | No signs of major pathology |
| Interference with daily activity (ADL) | |
| 3 | Pain with neurological signs of nerve compression (radiculopathy) |
| 4 | Signs of major pathology (e.g., instability, infection) |
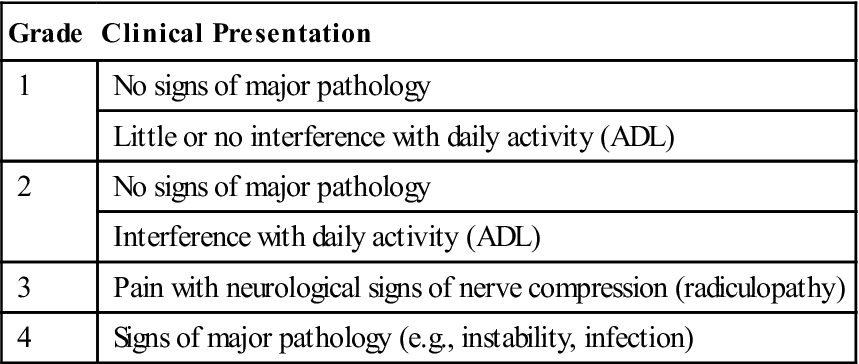
ADL, Activity of daily living.
Adapted from Guzman J, Haldeman S, Carroll LJ, et al: Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. J Manipulative Physiol Ther 32(2 Suppl):235, 2009.
TABLE 3-4
Factors That Increase Chances of Recovery from an Episode of Neck Pain
| Scenario and Grade of Neck Pain | Likely Increase | Might Increase | No Effect | Not Enough Evidence to Make Determination |
| General population | Younger age, no previous neck pain, good physical and psychological health, good coping, good social support | Being employed | — | Gender, general exercise or fitness prior to pain episode, cervical disc changes |
| At work | Exercise and sports, no prior pain or prior sick leave | Changing jobs (for certain job types), white collar job, greater influence over work | Age, ergonomics/ physical job demands, work-related psychosocial factors (but many such factors not studied) | Gender, compensation, litigation, obesity, smoking, cervical disc changes |
| After a traffic collision | No prior pain or sick leave, fewer initial symptoms, less symptom severity, Grade I WAD, good psychological health (e.g., not coping passively, no fear of movement, no post-injury anxiety), no early “overtreatment” | No prior pain problems, good prior health, non-tort insurance, no lawyer involvement, lower collision speed | Collision specific factors (such as, head position when struck, position in vehicle, direction of collision) | Age, gender, culture, prior physical fitness, cervical disc changes |
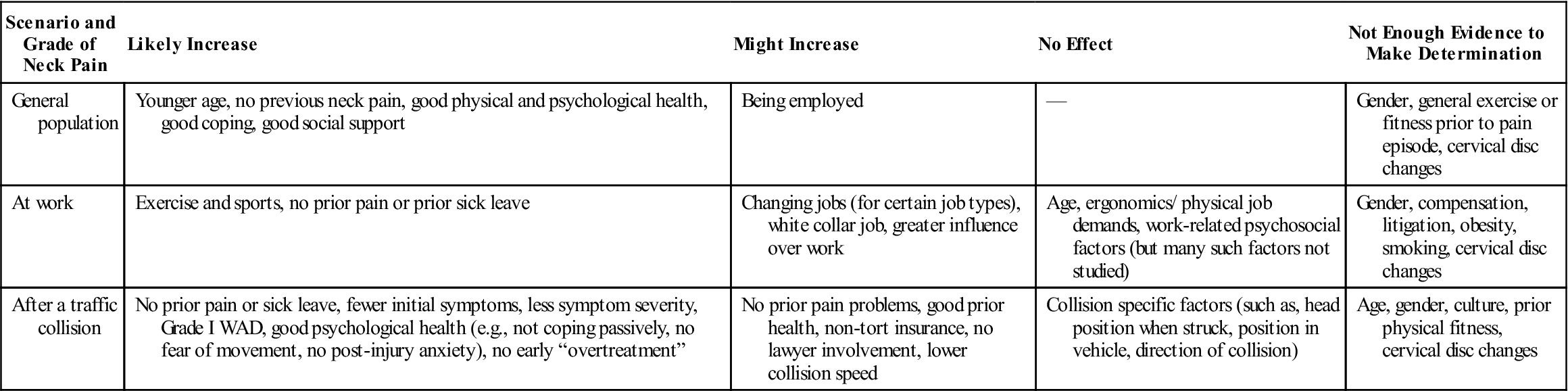
WAD, Whiplash-associated disorder.
From Guzman J, Haldeman S, Carroll LJ, et al: Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. J Manipulative Physiol Ther 32(2 Suppl):234, 2009.
![]() TABLE 3-5
TABLE 3-5
Clinical Yellow Flags Indicating Heightened Fear-Avoidance Beliefs
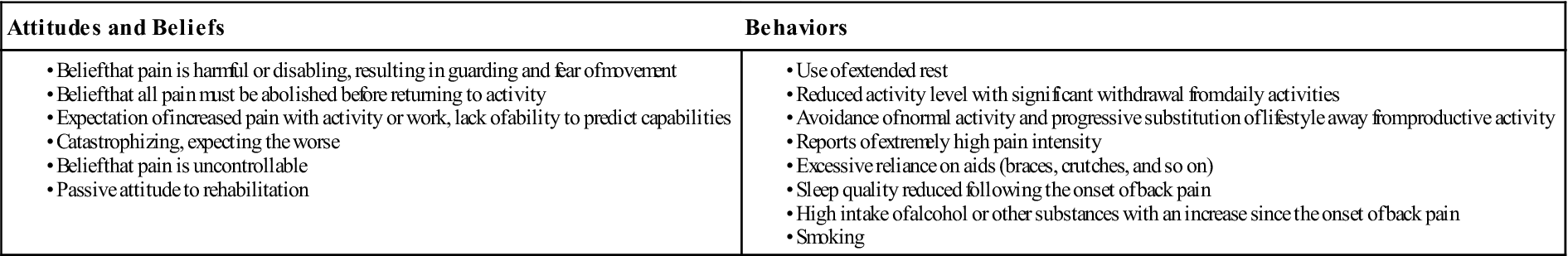
From Childs JD, Fritz JM, Piva SR, et al: Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther 34:686–700, 2004. Data from Kendall, et al: Guide to assessing psychosocial yellow flags in acute low back pain: risk factors for long-term disability and work loss, Wellington, New Zealand, 2002, Accident Rehabilitation and Compensation Insurance Corporation of New Zealand and the National Health Committee.
![]() TABLE 3-6
TABLE 3-6
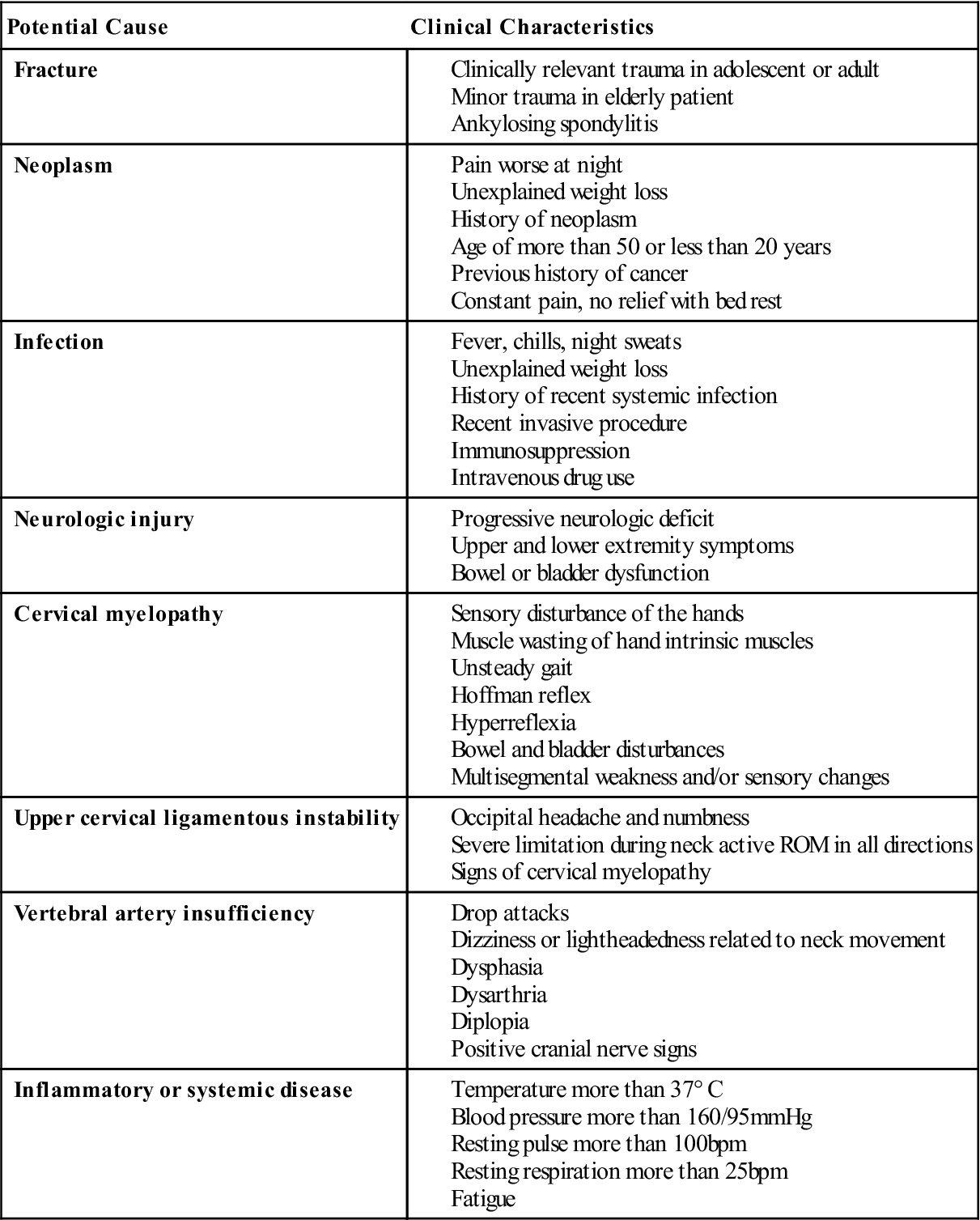
Modified from Rao RD, Currier BL, Albert TJ, et al: Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management. J Bone Joint Surg Am 89(6):1360–1378, 2007; Childs JD, Fritz JM, Piva SR, et al: Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther 34:688, 2004.
TABLE 3-7
The Quebec Severity Classification of Whiplash Associated Disorders
| Grade | Clinical Presentation |
| 0 | No neck symptoms, no physical sign(s) |
| 1 | No physical sign(s); neck pain; stiffness or tenderness only; neck complaints predominate; normal ROM; normal reflexes, dermatomes, and myotomes |
| 2 | Neck symptoms (pain, stiffness) and musculoskeletal sign(s)—such as, decreased ROM and point tenderness; soft tissue complaints (pain, stiffness) into shoulders and back; normal reflexes, dermatomes, and myotomes |
| 3 | Neck symptoms (pain, stiffness, restricted ROM) and neurological sign(s), such as decreased or absence of deep tendon reflexes, weakness (positive myotomes), and sensory (positive dermatome) deficits; x-ray shows no fracture; CT/MRI may show nerve involvement; possible disc lesion |
| 4 | Neck symptoms (pain, stiffness, restricted ROM) with fracture or dislocation and objective neurological signs, possible spinal cord signs |
CT, Computed tomography; MRI, magnetic resonance imaging; ROM, range of motion.
Modified from Spitzer WO, Skovron ML, Salmi LR, et al: Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine 20(8 Suppl):8S–58S, 1995.
TABLE 3-8
Differential Diagnosis of Cervical Nerve Root and Brachial Plexus Lesion
| Cervical Nerve Root Lesion | Brachial Plexus Lesion | |
| Cause | Disc herniation Stenosis Osteophytes Swelling with trauma Spondylosis |
Stretching of cervical spine Compression of cervical spine Depression of shoulder |
| Contributing factors | Congenital defects | Thoracic outlet syndrome |
| Pain | Sharp, burning in affected dermatomes | Sharp, burning in all or most of arm dermatomes, pain in trapezius |
| Paresthesia | Numbness, pins and needles in affected dermatomes | Numbness, pins and needles in all or most arm dermatomes (more ambiguous distribution) |
| Tenderness | Over affected area of posterior cervical spine | Over affected area of brachial plexus or lateral to cervical spine |
| Range of motion | Decreased | Decreased but usually returns rather quickly |
| Weakness | Transient paralysis usually Myotome may be affected |
Transient muscle weakness Myotomes affected |
| Deep tendon reflexes | Affected nerve root may be depressed | May be depressed |
| Provocative test | Side flexion, rotation and extension with compression increase symptoms Cervical traction decreases symptoms Upper limb tension tests positive |
Side flexion with compression (same side) or stretch (opposite side) may increase symptoms Upper limb tension tests may be positive |
TABLE 3-9
Factors That Decrease Chances of Getting a New Episode of Neck Pain
| Scenario and Grade of Neck Pain | Likely Decrease | Might Decrease | No Effect | Not Enough Evidence to Make Determination |
| General population | No previous neck pain, no other musculoskeletal problems, good psychological health | Younger age, male gender, non-smoking, changing rules in sports (like in ice hockey) | Obesity | Weight of school bags, cervical disc changes (on imaging) |
| At work | Younger age (peak risk in fourth and fifth decades), male gender, no previous pain in the neck, back or upper limbs, little psychological job strain, good co-worker support, active work (nonsedentary), less repetitive or precision work | Not being an immigrant or a visible minority, higher strength or endurance of the neck, not working with the neck bend for prolonged periods, non-smoking, no previous headaches, good physical health, “non-type A” personality, not working in awkward positions, light physical work, adequate keyboard position, no awkward head elbow and shoulder posture, no screen glare | Physical or sports activity during leisure, sleep quality, time spent on domestic activities, time spent on hobbies | Marital status, education, occupational class duration of employment, obesity, self-assessed health status, mental stress, job satisfaction, working with hands above the shoulder level, height of computer screen, cervical disc changes |
| After a traffic collision | — | Male gender, no previous neck pain, riding in back seat, side collision, no compensation for pain and suffering, specially engineered car seats and headrests | Tow bars in the car, age, type of child seat restraint | Awareness of collision, head position at time of collision, severity of collision impact, cervical disc changes (on imaging) |
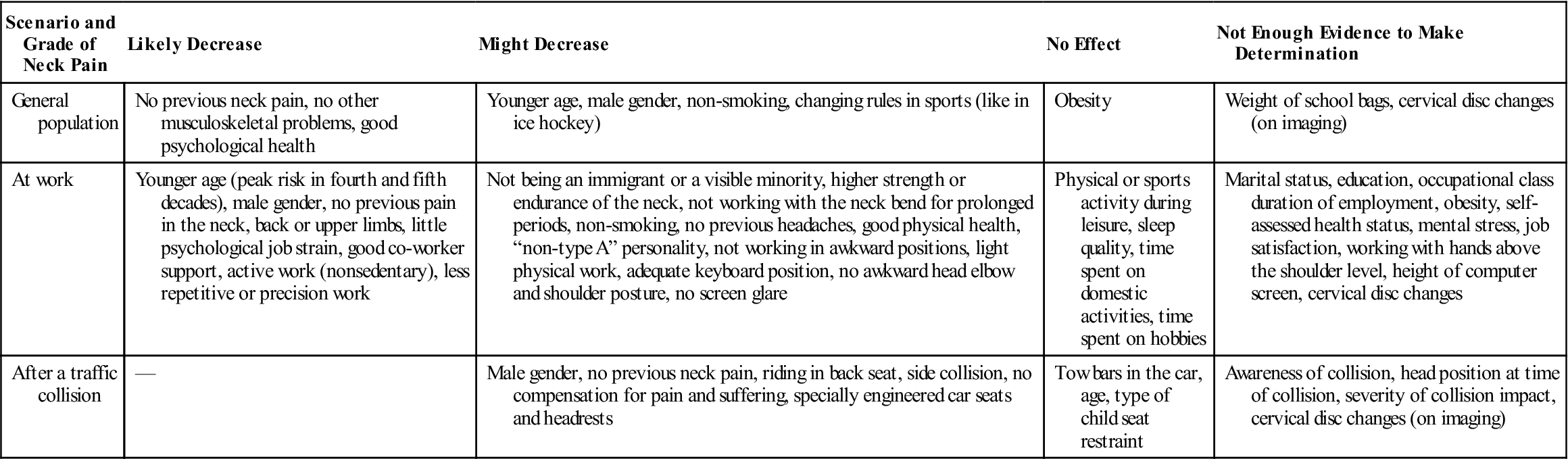
From Guzman J, Haldeman S, Carroll LJ, et al: Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. J Manipulative Physiol Ther 32(2 Suppl):233, 2009.
TABLE 3-10
Signs and Symptoms in Cervical Myelopathy
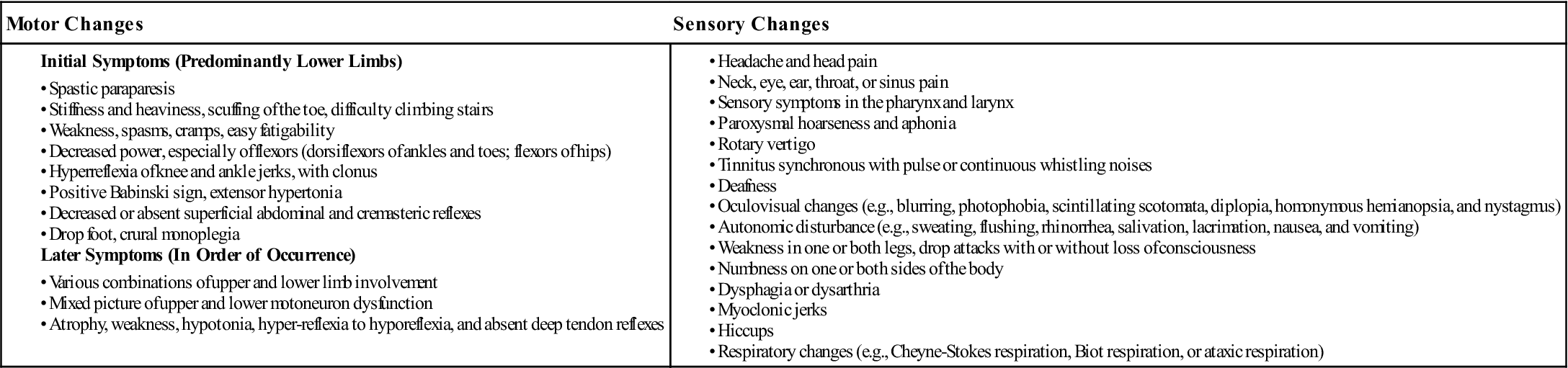
Modified from Bland JH: Disorders of the cervical spine, Philadelphia, 1994, WB Saunders, pp. 215–216.
TABLE 3-11
Differential Diagnosis of Neurological Disorders of the Cervical Spine and Upper Limb
| Cervical Radiculopathy (Nerve Root Lesion) | Cervical Myelopathy | Brachial Plexus Lesion (Plexopathy) | Burner (Transient Brachial Plexus Lesion) | Peripheral Nerve (Upper Limb) |
| Arm pain in dermatome distribution | Hand numbness, head pain, hoarseness, vertigo, tinnitus, deafness | Pain more localized to shoulder and neck (sometimes face) | Temporary pain in dermatome | No pain |
| Pain increased by extension and rotation or side flexion | Extension, rotation, and side flexion may all cause pain | Pain on compression of brachial plexus | Pain on compression or stretch of brachial plexus | No pain early; if contracture occurs (late), pain on stretching |
| Pain may be relieved by putting hand on head (C5, C6) | Arm positions have no effect on pain | Arm positions have no effect on pain* | Arm positions have no effect on pain* | Arm positions have no effect on pain* |
| Sensation (dermatome) affected | Sensation affected, abnormal pattern | Sensation (dermatome) affected | Sensation (dermatome) affected | Peripheral nerve sensation affected |
| Gait not affected | Wide-based gait drop attacks, ataxia; proprioception affected | Gait not affected | Gait not affected | Gait not affected |
| Altered hand function | Loss of hand function | Loss of arm function | Loss of function temporary | Loss of function of muscles supplied by nerve |
| Bowel and bladder not affected | Possible loss of bowel and bladder control | Bowel and bladder not affected | Bowel and bladder not affected | Bowel and bladder not affected |
| Weakness in myotome but no spasticity | Spastic paresis (especially in lower limb early, upper limb affected later) | Weakness in myotome | Temporary weakness in myotome | Weakness of muscles supplied by nerve |
| DTR hypoactive | Lower limb DTR hyperactive Upper limb DTR hyperactive |
DTR hypoactive | DTR not affected | DTR may be decreased |
| Negative pathological reflex | Positive pathological reflex | Negative pathological reflex | Negative pathological reflex | Negative pathological reflex |
| Negative superficial reflex | Decreased superficial reflex | Negative superficial reflex | Negative superficial reflex | Negative superficial reflex |
| Atrophy (late sign), hard to detect early | Atrophy | Atrophy | Atrophy possible | Atrophy (not usually with neuropraxia) |
TABLE![]() 3-12
3-12
Signs and Symptoms of Vertebrobasilar Artery Insufficiency*
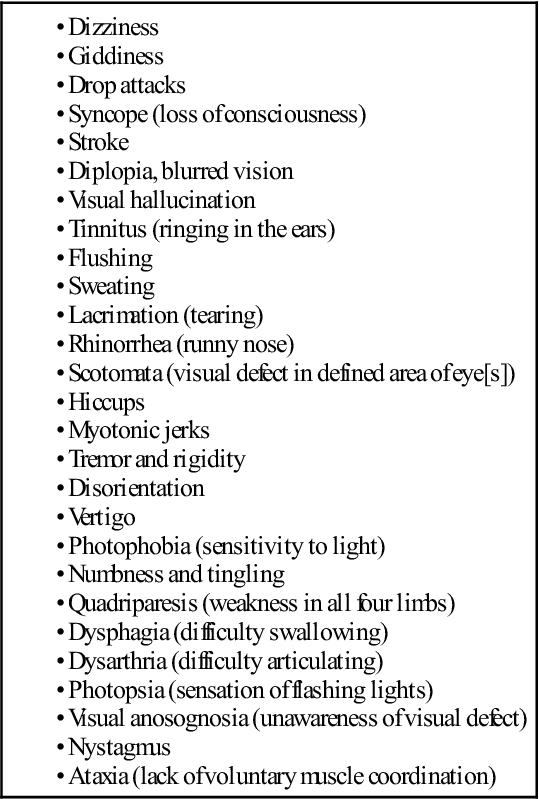
*These paraspinal symptoms result mainly from rotation and extension of the neck, although they sometimes occur during flexion. The spectrum of neurologic symptoms and signs is as broad as that of the structures potentially involved. In a complex, bizarre, and poorly explained neurologic syndrome, vertebrobasilar artery insufficiency should be suspected.
Modified from Bland JH: Disorders of the cervical spine, Philadelphia, 1994, W.B. Saunders Co., p. 217.
Observation
For a proper observation, the patient must be suitably undressed. However, the examiner should also watch the patient as he or she enters the examination room, and before or while he or she undresses. The spontaneous movements of these activities can be very helpful in determining the patient’s problems. For example, can the patient easily move the head when undressing? A male patient should wear only shorts, and a female patient should wear a bra and shorts for this part of the assessment. In some cases, the bra may have to be removed to determine whether there are any problems, such as thoracic outlet syndrome, thoracic symptoms being referred to the cervical spine, or functional restriction of movement of the ribs. The examiner should note the willingness of the patient to move and the patterns of movement demonstrated. Facial expression of the patient can often give the examiner an indication of the amount of pain the patient is experiencing.
The patient may be seated or standing. Usually, a standing posture is best because the posture of the whole body can be observed (see Chapter 15). Abnormalities in one area frequently affect another area. For example, excessive lumbar lordosis may cause a “poking” chin to compensate for the lumbar deformity and to maintain the body’s center of gravity. In the cervical spine region, the examiner should note the following:
Head and Neck Posture.
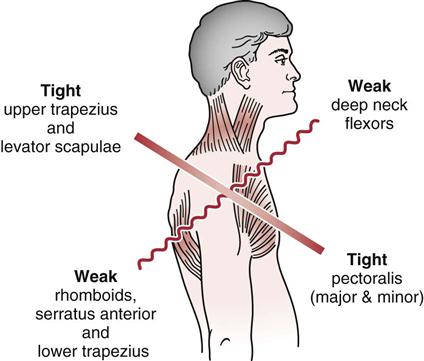
Is the head in the midline, and does the patient have a normal lordotic curvature (30° to 40°) (see Figure 3-7; Figure 3-12)? This curvature along with the other spinal curvatures in the lower spine provides a shock absorption mechanism for the spine and helps the body maintain its center of gravity.57 From the front, the chin should be in line with the sternum (manubrium) and from the side, the ears should be in line with the shoulder and the forehead vertical. Is there evidence of torticollis (congenital or acquired) (Figure 3-13), Klippel-Feil syndrome (congenital fusion of some cervical vertebra, usually C3 to C5) (Figure 3-14), or other neck deformity? Does the patient exhibit a poking chin or a “military posture?” A habitual poking chin can result in adaptive shortening of the occipital muscles. It also causes the cervical spine to change alignment resulting in increased stress of the facet joints and posterior discs and other posterior elements (Figure 3-15). The position may also lead to weaknesses of the deep neck flexors.58 Janda59 described a cervical “upper crossed syndrome” to show the effect of a “poking chin” posture on the muscles. With this syndrome, the deep neck flexors are weak, as are the rhomboids, serratus anterior, and often the lower trapezius. Opposite these weak muscles are tight pectoralis major and minor, along with upper trapezius and levator scapulae (Figure 3-16). Does the head sit in the middle of the shoulders? Is the head tilted or rotated to one side or the other, indicating possible torticollis? Does this posture appear to be habitual (in other words, does the patient always go back to this posture)? Habitual posture may result from postural compensation, weak muscles, hearing loss, temporomandibular joint problems, or wearing of bifocals or trifocals. The trapezius neck line should be equal on both sides. Head and neck posture should be checked with the patient sitting and then standing, and any differences should be noted.
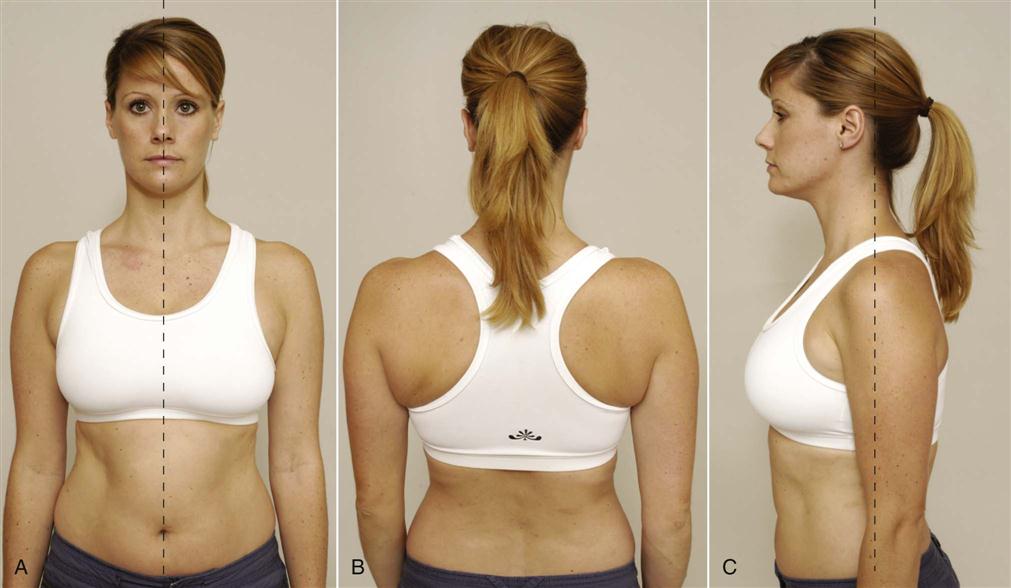
A, Anterior view. B, Posterior view. C, Lateral or side view. With normal posture, the ear should be in line with the shoulder and the forehead vertical. Note that this model is a “chin poker” with the head sitting anteriorly, which leads to a decrease in the lordotic curve.
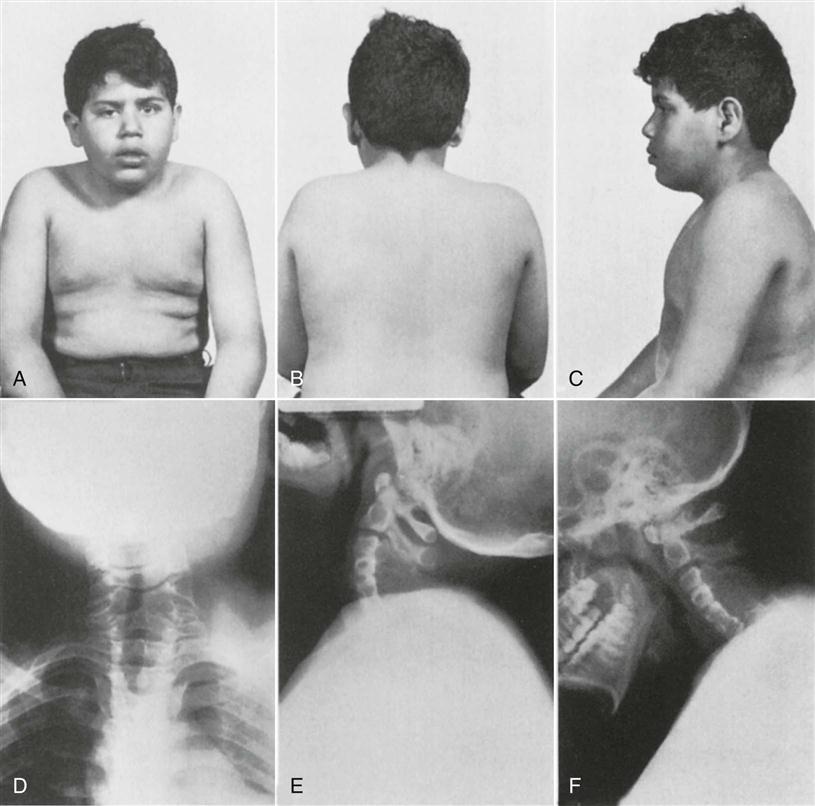
Clinical appearance of the patient. A, Anterior view. B, Posterior view. C, Lateral view. Note the short neck with the head appearing to sit directly on the thorax. Anteroposterior (D) and lateral (E, extension; F, flexion) roentgenograms of the cervical spine. Note the failure of segmentation and the fusion into a homogeneous mass of bone of the four lower cervical vertebrae. (From Tachdjian MO: Pediatric orthopedics, Philadelphia, 1972, WB Saunders, p. 77.)
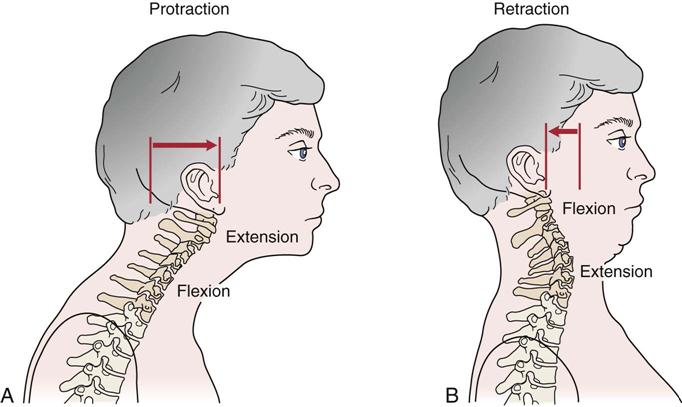
A, During protraction of the cranium, the lower-to-mid cervical spine flexes as the upper craniocervical region extends. B, During retraction of the cranium, in contract, the lower-to-mid cervical spine extends as the upper craniocervical region flexes. Note the change in distance between the C1–C2 spinous processes during the two movements. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 284.)
Shoulder Levels.
Usually the shoulder on the dominant side will be slightly lower than that on the nondominant side. With injury, the injured side may be elevated to provide protection (e.g., upper trapezius and/or levator scapulae) or because of muscle spasm. Rounded shoulders may be the result of or the cause of a poking chin. Rounding also causes the scapulae to protract, the humerus to medially rotate, and the anterior structures of the shoulder to tighten.
Muscle Spasm or Any Asymmetry.
Is there any atrophy of the deltoid muscle (axillary nerve palsy) or torticollis (muscle spasm, tightness, or prominence of the sternocleidomastoid muscle) (see Figure 3-13)?
Facial Expression.
The examiner should observe the patient’s facial expression as the patient moves from position to position, makes different movements, and explains the problem. Such observation should give the examiner an idea of how much the patient is subjectively suffering.
Bony and Soft-Tissue Contours.
If the cervical spine is injured, the head tends to be tilted and rotated away from the pain, and the face is tilted upward. If the patient is hysterical, the head tends to be tilted and rotated toward the pain, and the face is tilted down.
Evidence of Ischemia in Either Upper Limb.
The examiner should note any altered coloration of the skin, ulcers, or vein distention as evidence of upper limb ischemia.
Normal Sitting Posture.
The nose should be in line with the manubrium and xiphoid process of the sternum. From the side, the ear lobe should be in line with the acromion process and the high point on the iliac crest for proper postural alignment. The normal curve of the cervical spine is a lordotic type of curve. Referred pain from conditions, such as spondylosis, tends to occur in the shoulder and arm rather than the neck.
Examination
A complete examination of the cervical spine must be performed, including the neck and both upper limbs. Many of the symptoms that occur in an upper limb originate from the neck. Unless there is a history of definite trauma to a peripheral joint, an upper limb scanning examination must be performed to rule out problems within the neck.
Active Movements
The first movements that are carried out are the active movements of the cervical spine with the patient in the sitting position. The examiner is looking for differences in range of movement and in the patient’s willingness to do the movement.60 The ROM taking place in this phase is the summation of all movements of the entire cervical spine, not just at one level. This combined movement allows for greater mobility in the cervical spine while still providing a firm support for the trunk and appendages. The ROM available in the cervical spine is the result of many factors, such as the flexibility of the intervertebral discs, the shape and inclination of the articular processes of the facet joints, and the slight laxity of the ligaments and joint capsules. Female patients tend to have a greater active range of motion than males, except in flexion, but the differences are not great. The range available decreases with age, except rotation at C1 to C2, which may increase.61,62
The movements should be done in a particular order so that the most painful movements are done last, and no residual pain is carried over from the previous movement.1 If the patient has complained of pain on specific movements in the history, these movements are done last. In the very acute cervical spine, only some movements—those that give the most information—are performed in order to avoid undue exacerbation of symptoms.
While the patient performs the active movements, the examiner looks for limitation of movement and possible reasons for pain, spasm, stiffness, or blocking. As the patient reaches the full range of active movement, passive overpressure may be applied very carefully, but only if the movement appears to be full and not too painful (see passive movement in a later discussion). The overpressure helps the examiner to test the end feel of the movement as well as differentiating between physiological (active) end range and anatomical (passive) end range. The examiner must be careful when applying overpressure to rotation or any combination of rotation, side flexion, and extension.8 In these positions, the vertebral artery is often compressed, which can lead to a decrease in blood supply to the brain. Should this occur, the patient may complain of dizziness or feel faint. If the patient exhibits these symptoms, the examiner must use extreme care during these movements, the rest of the assessment, and treatment.
The examiner can differentiate between movement in the upper and lower cervical spine. During flexion, nodding occurs in the upper cervical spine, whereas flexion occurs in the lower cervical spine. If the nodding movement does not occur, it indicates restriction of movement in the upper cervical spine; if flexion does not occur, it indicates restriction of motion in the lower cervical spine. Movement can occur between C1 and C2 without affecting the other vertebrae, but this is not true with other cervical vertebrae. In other words, for C2 to C7, if one vertebra moves, the ones adjacent to it will also move. Thus, the active movements in the cervical spine can be divided into two parts: those testing the upper cervical spine (C0 to C2) and those involving the rest of the cervical spine (C2 to C7) (Figure 3-17). Table 3-13 gives the approximate ROMs in the different parts of the cervical spine.63
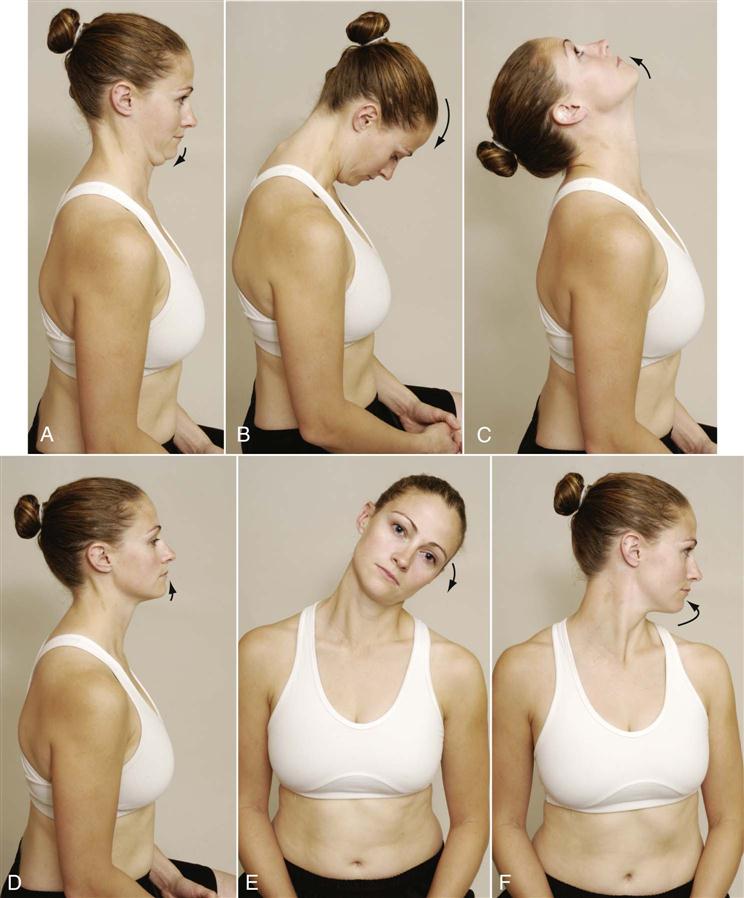
 Figure 3-17 Active movements of the cervical spine.
Figure 3-17 Active movements of the cervical spine.A, Anterior nodding (upper cervical spine). B, Flexion. C, Extension. D, Posterior nodding (upper cervical spine). E, Side flexion. F, Rotation.
TABLE 3-13
Approximate Range of Motion for the Three Planes of Movement for the Joints of the Craniocervical Region*
| Joint or Region | Flexion and Extension (Sagittal Plane, Degrees) | Axial Rotation (Horizontal Plane, Degrees) | Lateral Flexion (Frontal Plane, Degrees) |
| Atlanto-occipital joint | Flexion: 5 Extension: 10 Total: 15 |
Negligible | About 5 |
| Atlanto-axial joint complex | Flexion: 5 Extension: 10 Total: 15 |
40–45 | Negligible |
| Intracervical region (C2–C7) | Flexion: 35 Extension: 70 Total: 105 |
45 | 35 |
| Total across craniocervical region | Flexion: 45–50 Extension: 85 Total: 130–135 |
90 | About 40 |
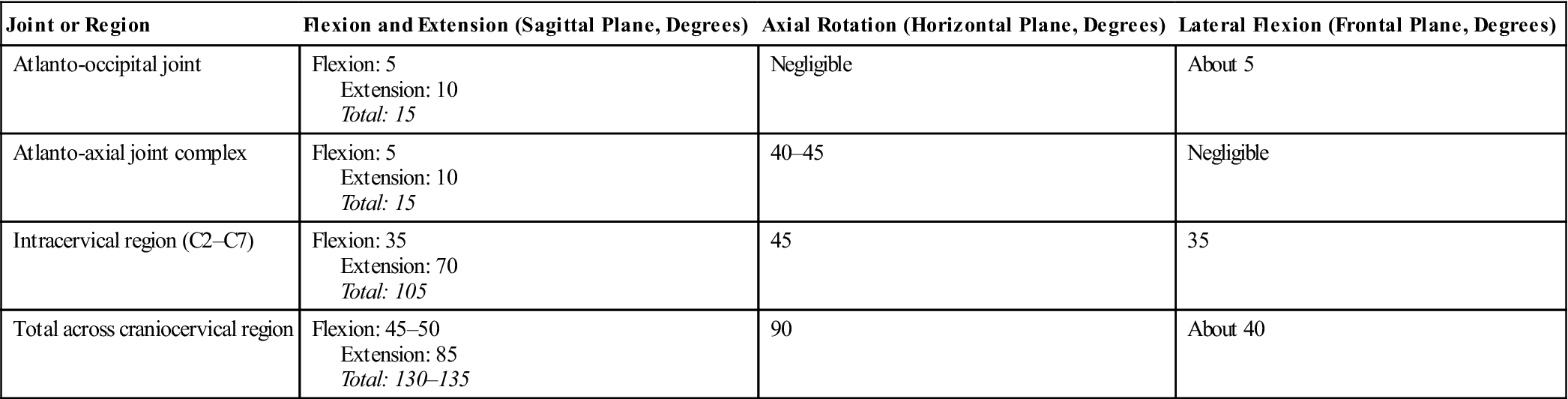
*The horizontal and frontal plane motions are to one side only. Data are compiled from multiple sources and subject to large intersubject variations.
From Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 278.
Flexion
To test flexion movement in the upper cervical spine, the patient is asked to nod or place the chin on the Adam’s apple. Normally this movement is pain free. Positive symptoms (e.g., tingling in feet, electric shock sensation down the neck [Lhermitte sign], severe pain, nausea, cord signs) all indicate severe pathology (e.g., meningitis, tumor, dens fracture).13 While the patient is flexing (nodding) the head, the examiner can palpate the relative movement between the mastoid and transverse process of C1 on each side comparing both sides for hypomobility or hypermobility between C0 and C1.13 Likewise, the examiner can palpate the posterior arch of C1 and the lamina of C2 during the nodding movement to compare the relative movement.13 For flexion, or forward bending, of the lower cervical spine, the maximum ROM is 80° to 90°. The extreme of ROM is normally found when the chin is able to reach the chest with the mouth closed; however, up to two finger widths between chin and chest is considered normal. If the deep neck flexors are weak, the sternocleidomastoid muscles will initiate the flexion movement, causing the jaw to lead the movement, not the nose, since the sternocleidomastoid muscles will cause the chin to initially elevate before flexion occurs.52,64,65 In flexion, the intervertebral disc widens posteriorly and narrows anteriorly. The intervertebral foramen is 20% to 30% larger on flexion than on extension. The vertebrae shift forward in flexion and backward in extension (Figures 3-18 and 3-19). Also, the mastoid process moves away from the C1 transverse process on flexion and extension. As the patient forward flexes, the examiner should look for a posterior bulging of the spinous process of the axis (C2). This bulging may result from forward subluxation of the atlas, which allows the spinous process of the axis to become more prominent. If this sign appears, the examiner should exercise extreme caution during the remainder of the cervical assessment. To verify the subluxation, the Sharp-Purser test (see under Special Tests) may be performed, but only with extreme care.
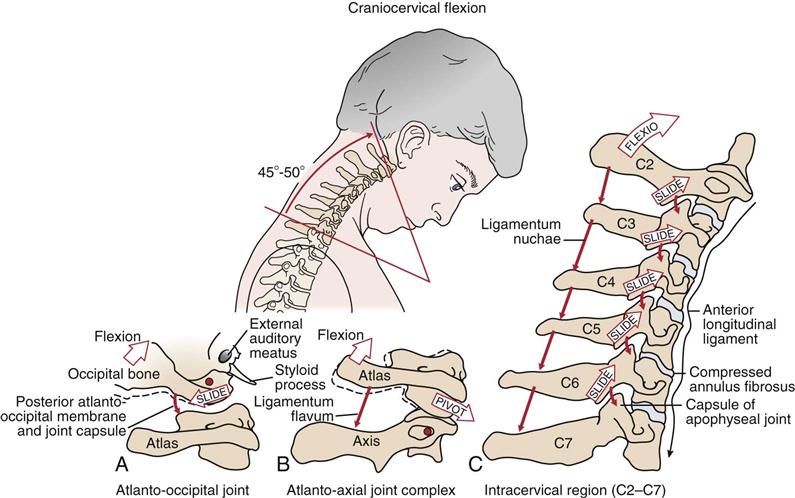
A, Atlanto-occipital joint. B, Atlanto-axial joint complex. C, Intracervical region (C2–C7). Note in C that flexion slackens the anterior longitudinal ligament and increases the space between the adjacent laminae and spinous processes. Elongated and taut tissues are indicated by thin black arrows; slackened tissue is indicated by a wavy black arrow. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 281.)
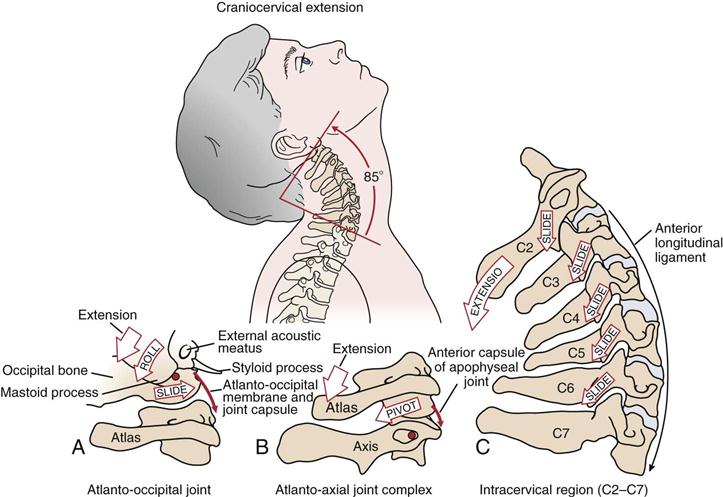
A, Atlanto-occipital joint. B, Atlanto-axial joint complex. C, Intracervical region (C2–C7). Elongated and taut tissues are indicated by thin black arrows. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 280.)
Extension
To test extension in the upper cervical spine, the patient is asked to lift the chin up without moving the neck. The examiner can lift the occiput at the same time. If serious symptoms arise (e.g., tingling in the feet, loss of balance, drop attack), it is suggestive of spinal cord compression or vertebrobasilar dysfunction.13 Extension, or backward bending of the cervical spine, is normally limited to 70°. Because there is no anatomic block to stop movement going past this position, problems often result from whiplash or cervical strain. Normally, there is sufficient extension to allow the plane of the nose and forehead to be nearly horizontal. When the head is held in extension, the atlas tilts upward, resulting in posterior compression between the atlas and occiput.
Side Flexion
Side, or lateral, flexion is approximately 20° to 45° to the right and left (Figure 3-20). As the patient does the movement, the examiner can palpate adjacent transverse processes on the convex side to determine relative movement at each level. When the patient does the movement, the examiner should ensure that the ear moves toward the shoulder and not the shoulder toward the ear.
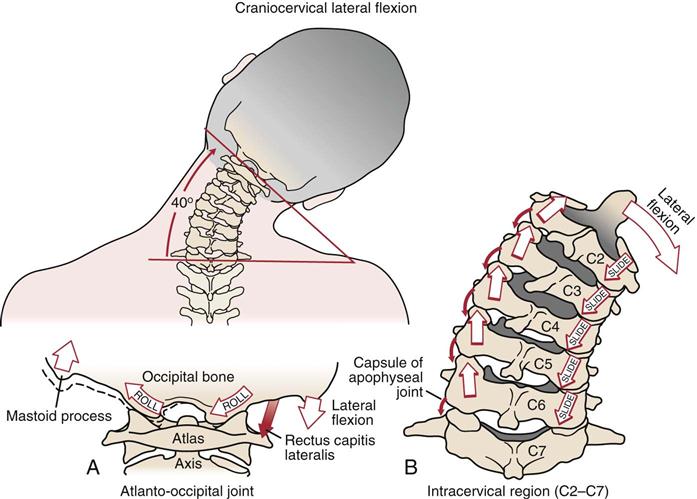
A, Atlanto-occipital joint. The primary function of the rectus capitis lateralis is to laterally flex this joint. Note the slight compression and distraction of the joint surfaces. B, Intracervical region (C2–C7). Note the ipsilateral coupling pattern between axial rotation and lateral flexion. Elongated and taut tissue is indicated by thin black arrows. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 286.)
Rotation
Normally, rotation is 70° to 90° right and left, and the chin does not quite reach the plane of the shoulder (Figure 3-21 ). Rotation and side flexion always occur together (coupled movement) but not necessarily in the same direction.20,21 This combined movement, which may or may not be visible in a given patient, occurs because of the shape of the articular surfaces of the facet joints; this shape is coronally oblique. Most of the rotation occurs between C1 and C2. If the patient can rotate 40° to 50°, then it is unlikely that the C1/C2 articulation is at fault.13 If, however, side flexion occurs early to allow full motion, C1–C2 is probably involved.13
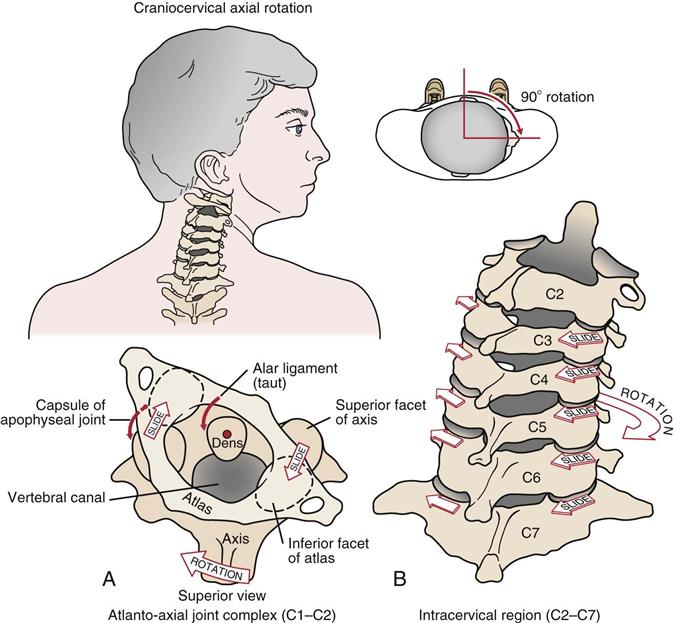
A, Atlanto-axial joint complex. B, Intracervical region (C2–C7). (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 285.)
If, in the history, the patient has complained that repetitive movements or sustained postures have caused problems, not only should the specific movements be performed, but they should be either repeated several times or sustained to see if the symptoms are exacerbated. If a patient has complained in the history that a movement in other than a cardinal plane or a combined movement (e.g., side flexion, rotation, and extension combined) exacerbates the symptoms, then these movements should be performed as well. For example, the cervical flexion-rotation test ![]() in which the patient flexes the cervical spine to the point of pain or discomfort and then, while holding the position, rotates the head, is considered positive for pain and dysfunction arising from the C1 to C2 segment in cervicogenic headaches if pain occurs with the rotation as well.66–68 Table 3-14 outlines examples of movement restrictions and possible causes.
in which the patient flexes the cervical spine to the point of pain or discomfort and then, while holding the position, rotates the head, is considered positive for pain and dysfunction arising from the C1 to C2 segment in cervicogenic headaches if pain occurs with the rotation as well.66–68 Table 3-14 outlines examples of movement restrictions and possible causes.
TABLE 3-14
Movement Restriction and Possible Causes
| Movement Restriction | Possible Causes |
| Extension and right side bending | Right extension hypomobility |
| Left flexor muscle tightness | |
| Anterior capsular adhesions | |
| Right subluxation | |
| Right small disc protrusion | |
| Flexion and right side bending | Left flexion hypomobility |
| Left extensor muscle tightness | |
| Extension and right side bending restriction greater than extension and left side bending | Left posterior capsular adhesions |
| Left subluxation | |
| Left capsular pattern (arthritis, arthrosis) | |
| Flexion and right side bending restriction equal to extension and left side flexion | Left arthrofibrosis (very hard capsular end feel) |
| Side bending in neutral, flexion, and extension | Uncovertebral hypomobility or anomaly |
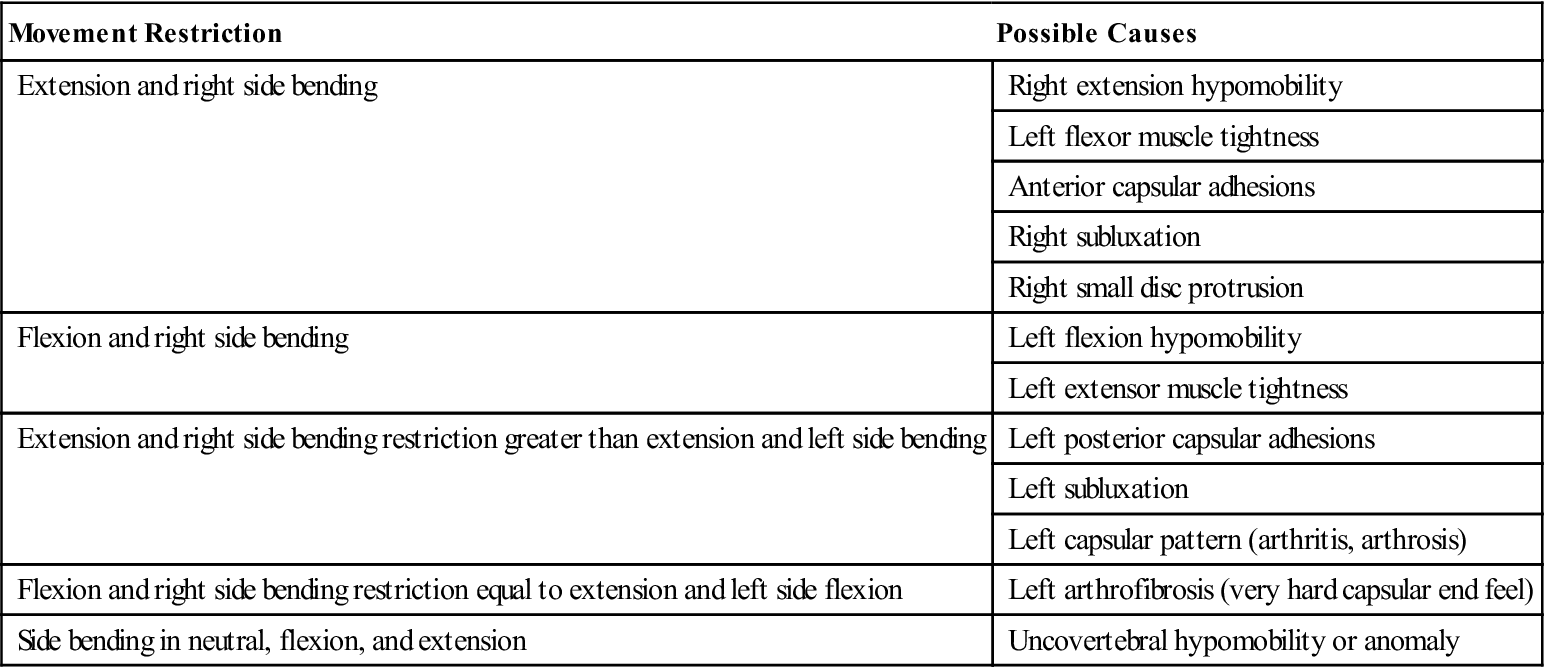
From Dutton M: Orthopedic examination, evaluation and intervention, New York, 2004, McGraw Hill, p. 1050.
Passive Movements
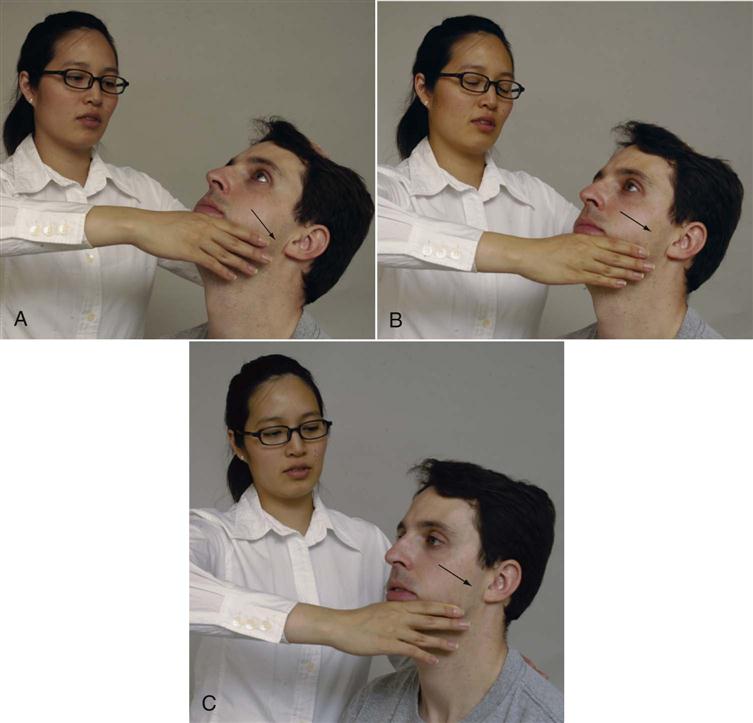
If the patient does not have full ROM or the examiner has not applied overpressure to determine the end feel of the movement, the patient should be asked to lie in a supine position. The examiner then passively tests flexion, extension, side flexion, and rotation, as in the active movements. The passive ROM with the patient supine is normally greater than the active and passive ROM with the patient sitting. For example, in sitting, active side flexion is about 45°, whereas in supine lying, passive side flexion is 75° to 80° with the examiner often able to take the ear to the shoulder. This increased range in the supine position results from relaxation of the muscles that, in sitting, are trying to hold the head up against gravity. For the cervical spine, therefore, passive movements with overpressure should be performed along with active movements. Active movements with overpressure at end of range do not give a true impression of end feel for the cervical spine. During passive movements, the examiner can palpate between adjacent vertebra to feel the relative amount of movement on each side. For flexion, the examiner palpates between the mastoid process and the transverse process for movement between C0 and C1 (Figure 3-22, A) and between the arch of C1 and spinous process of C2 for movement between C1 and C2 (Figure 3-22, B). For the rest of the cervical spine and upper thoracic spine, the examiner can palpate between the spinous processes at each level while passively and progressively flexing the spine. To feel the movement, the examiner will find that as one works down the spine from C2 to C7, more flexion is required to feel the movement (Figure 3-22, C). Movement at each segment during side flexion and rotation may be felt by palpating the adjacent transverse processes on each side while doing the movement (Figure 3-23). To test rotation between the occiput and C1, the examiner holds the patient’s head in position and palpates the transverse processes of C1 (Figure 3-24). The examiner must first find the mastoid process on each side and then move the fingers inferiorly and anteriorly until a hard bump (i.e., the transverse process of C1) is palpated on each side (usually below the ear lobe and just behind the jaw). Palpation in the area of the C1 transverse process is generally painful, so care must be taken. The examiner then rotates the patient’s head while palpating the transverse processes; the transverse process on the side to which the head is rotated will seem to disappear (bottom one) while the other side (top one) seems to be accentuated in the normal case. If this disappearance/accentuation does not occur, there is restriction of movement between C0 and C1 on that side. To test rotation at C1–C2, the examiner stands beside the seated patient and side bends the head and neck, followed by rotation to the opposite side. As the rotation is performed, the examiner palpates the relative position of the C1 and C2 transverse processes as the head is rotated. To limit side flexion to a specific segment, as the examiner side flexes the head, the examiner applies an opposing translation force in the opposite direction to the passive movement to limit movement below that being tested.13 With all of these movements, the end feel should be a solid tissue stretch.
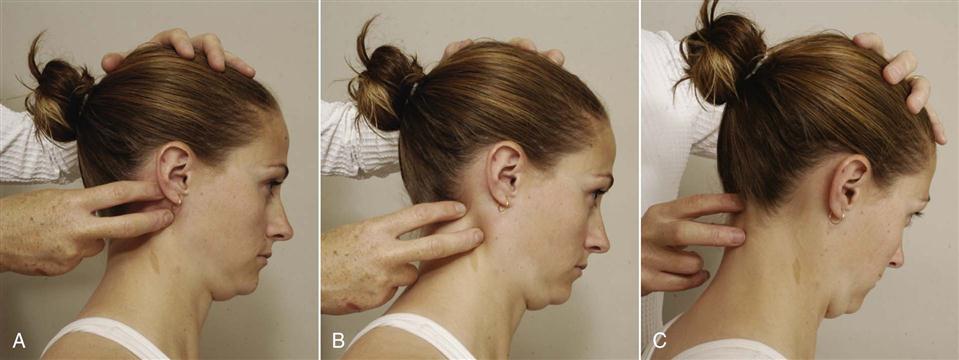
 Figure 3-22 Testing passive movement in the cervical spine.
Figure 3-22 Testing passive movement in the cervical spine.A, Position testing for occipito-atlantal joint. B, Position testing for atlanto-axial joint. C, Flexion testing of C2–T1.
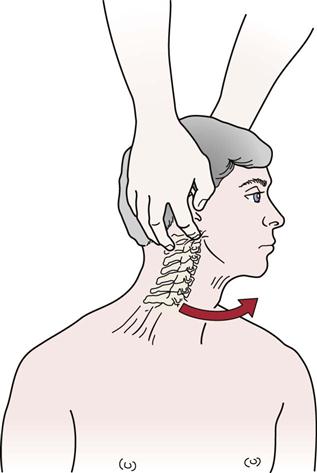
 Figure 3-24 Left rotation of the occiput on C1.
Figure 3-24 Left rotation of the occiput on C1.Note the index finger palpating the right transverse process of C1.
If the passive movements with overpressure are normal and pain free, the examiner may, with great care, test other positions. For the flexion-rotation test, the patient lies supine while the examiner flexes the neck fully and, while holding this position, passively rotates the head as far as possible within comfort limits.69 Hall and Robinson69 report significant restriction in rotation in patients complaining of cervicogenic headache indicating C1 to C2 segmental dysfunction. The quadrant position is end-range extension, side flexion, and rotation, a position that increases the vulnerability of anterior, posterior, and lateral tissues of the neck, including the vertebral artery.70 If overpressure is applied in the quadrant position and symptoms result, it is highly suggestive of nerve root pathology (radicular signs), apophyseal joint involvement (localized pain), or vertebral artery involvement (dizziness, nausea).52
In addition to the passive movements of the whole cervical spine, physiological movements between each pair of vertebrae may be performed. These are called passive physiological intervertebral movements (PPIVMs). By stabilizing or blocking the movement of one vertebra (usually the distal one) and then passively moving the head through the different physiological movements (e.g., flexion, extension, side flexion, rotation), each segment can be tested. Needless to say, the amount of movement of each segment will be considerably less than the whole.71
Passive movements are performed to determine the end feel of each movement. This may give the examiner an idea of the pathology involved. The normal end feels of the cervical spine motions are tissue stretch for all four movements. As with active movements, the most painful movements are done last. The examiner should also note whether a capsular pattern (i.e., side flexion and rotation equally limited; extension less limited) is present. Overpressure may be used to test the entire spine (Figure 3-25, A) by testing it at the end of the ROM, or proper positioning may be used to test different parts of the cervical spine.72 For example, end feel for movement of the lower cervical spine into extension is tested with minimal extension and the head pushed directly posterior (Figure 3-25, C), whereas the upper cervical spine is tested by “nodding” the head into extension and pushing posteriorly at an approximate 45° angle (Figure 3-25, B).73
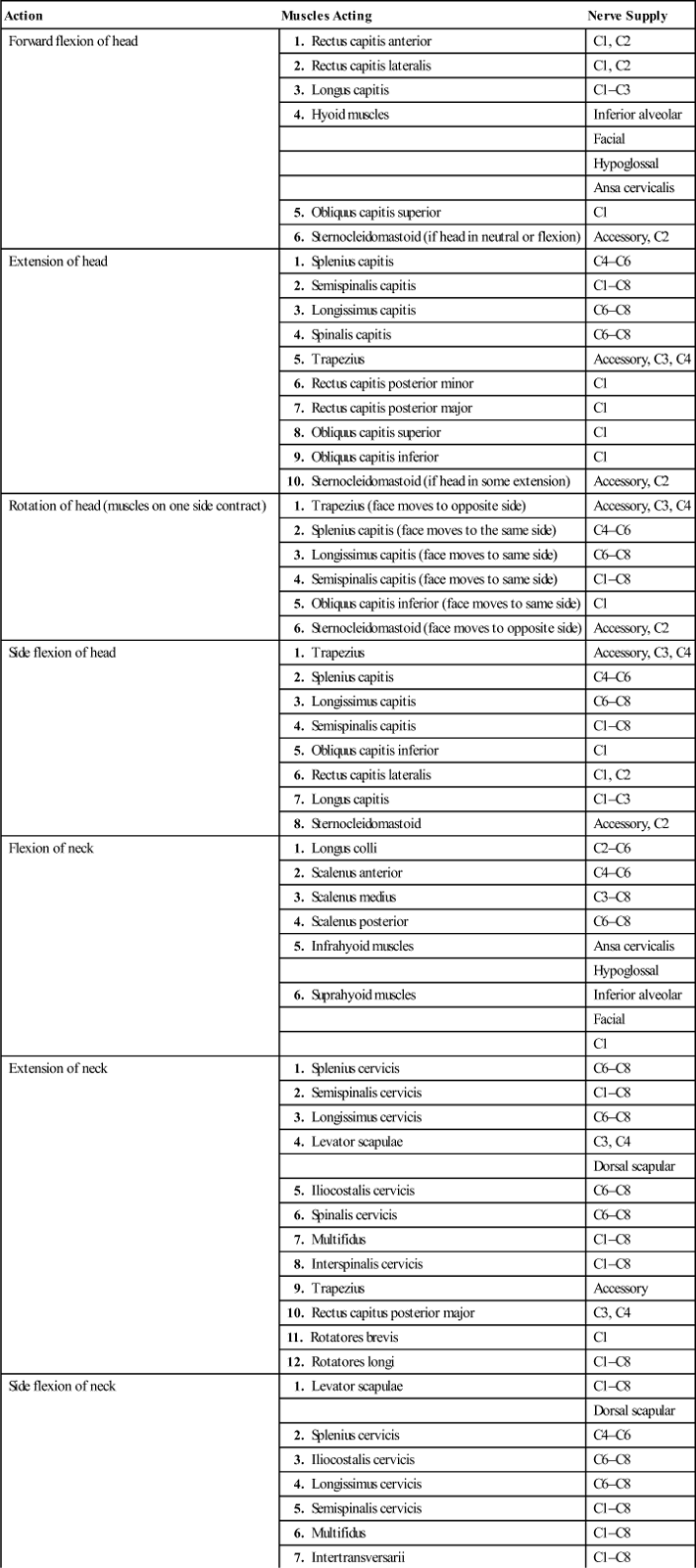
Resisted Isometric Movements
The same movements that were done actively (flexion, extension, side flexion, and rotation) are then tested isometrically to determine relative muscle strength of each movement and to compare opposite movements.74 It is better for the examiner to place the patient in the resting position and then say, “Don’t let me move you,” rather than to tell the patient, “Contract the muscle as hard as possible.” In this way, the examiner ensures that the movement is as isometric as possible and that a minimal amount of movement occurs (Figure 3-26). The examiner should ensure that these movements are done with the cervical spine in the neutral position and that painful movements are done last. Neck flexion tests cranial nerve XI and the C1 and C2 myotomes as well as muscle strength or state. By using Table 3-15 and looking at the various combinations of muscles that cause the movement (Figure 3-27), the examiner is often able to decide which muscle is at fault. If, in the history, the patient has complained that certain loaded or combined movements (those movements giving resistance other than gravity) are painful, the examiner should not hesitate to carefully test these movements isometrically to better ascertain the problem. If a neurological injury is suspected, the examiner must carefully assess for muscle weakness to determine the structures injured. If a severe neuropraxia or axonotmesis has occurred, there may be residual weakness even though muscle atrophy may not be evident.
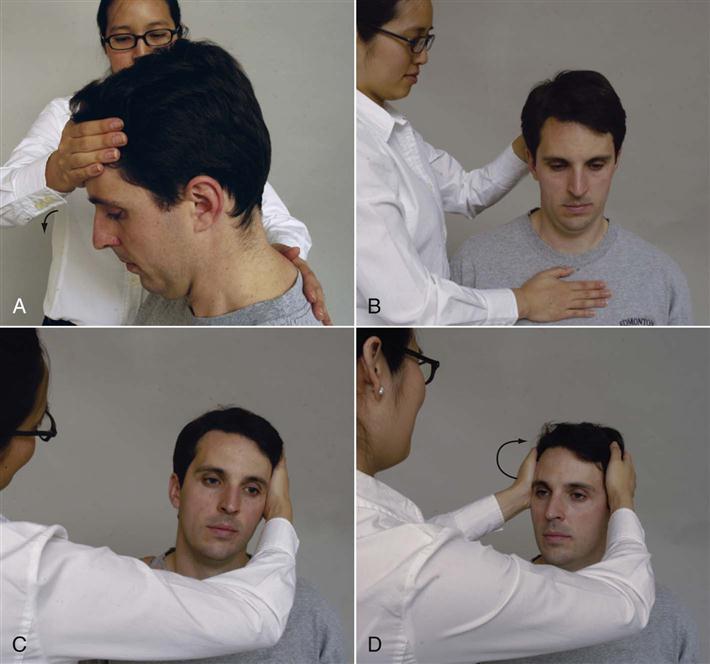
 Figure 3-26 Positioning for resisted isometric movement.
Figure 3-26 Positioning for resisted isometric movement.A, Flexion. Note slight flexion of neck before giving resistance. B, Extension. Note slight flexion of neck before giving resistance. C, Side flexion (left side flexion shown). D, Rotation (left rotation shown).
TABLE 3-15
Muscles of the Cervical Spine: Their Actions and Nerve Supply
| Action | Muscles Acting | Nerve Supply |
| Forward flexion of head | 1. Rectus capitis anterior | C1, C2 |
| 2. Rectus capitis lateralis | C1, C2 | |
| 3. Longus capitis | C1–C3 | |
| 4. Hyoid muscles | Inferior alveolar | |
| Facial | ||
| Hypoglossal | ||
| Ansa cervicalis | ||
| 5. Obliquus capitis superior | C1 | |
| 6. Sternocleidomastoid (if head in neutral or flexion) | Accessory, C2 | |
| Extension of head | 1. Splenius capitis | C4–C6 |
| 2. Semispinalis capitis | C1–C8 | |
| 3. Longissimus capitis | C6–C8 | |
| 4. Spinalis capitis | C6–C8 | |
| 5. Trapezius | Accessory, C3, C4 | |
| 6. Rectus capitis posterior minor | C1 | |
| 7. Rectus capitis posterior major | C1 | |
| 8. Obliquus capitis superior | C1 | |
| 9. Obliquus capitis inferior | C1 | |
| 10. Sternocleidomastoid (if head in some extension) | Accessory, C2 | |
| Rotation of head (muscles on one side contract) | 1. Trapezius (face moves to opposite side) | Accessory, C3, C4 |
| 2. Splenius capitis (face moves to the same side) | C4–C6 | |
| 3. Longissimus capitis (face moves to same side) | C6–C8 | |
| 4. Semispinalis capitis (face moves to same side) | C1–C8 | |
| 5. Obliquus capitis inferior (face moves to same side) | C1 | |
| 6. Sternocleidomastoid (face moves to opposite side) | Accessory, C2 | |
| Side flexion of head | 1. Trapezius | Accessory, C3, C4 |
| 2. Splenius capitis | C4–C6 | |
| 3. Longissimus capitis | C6–C8 | |
| 4. Semispinalis capitis | C1–C8 | |
| 5. Obliquus capitis inferior | C1 | |
| 6. Rectus capitis lateralis | C1, C2 | |
| 7. Longus capitis | C1–C3 | |
| 8. Sternocleidomastoid | Accessory, C2 | |
| Flexion of neck | 1. Longus colli | C2–C6 |
| 2. Scalenus anterior | C4–C6 | |
| 3. Scalenus medius | C3–C8 | |
| 4. Scalenus posterior | C6–C8 | |
| 5. Infrahyoid muscles | Ansa cervicalis | |
| Hypoglossal | ||
| 6. Suprahyoid muscles | Inferior alveolar | |
| Facial | ||
| C1 | ||
| Extension of neck | 1. Splenius cervicis | C6–C8 |
| 2. Semispinalis cervicis | C1–C8 | |
| 3. Longissimus cervicis | C6–C8 | |
| 4. Levator scapulae | C3, C4 | |
| Dorsal scapular | ||
| 5. Iliocostalis cervicis | C6–C8 | |
| 6. Spinalis cervicis | C6–C8 | |
| 7. Multifidus | C1–C8 | |
| 8. Interspinalis cervicis | C1–C8 | |
| 9. Trapezius | Accessory | |
| 10. Rectus capitus posterior major | C3, C4 | |
| 11. Rotatores brevis | C1 | |
| 12. Rotatores longi | C1–C8 | |
| Side flexion of neck | 1. Levator scapulae | C1–C8 |
| Dorsal scapular | ||
| 2. Splenius cervicis | C4–C6 | |
| 3. Iliocostalis cervicis | C6–C8 | |
| 4. Longissimus cervicis | C6–C8 | |
| 5. Semispinalis cervicis | C1–C8 | |
| 6. Multifidus | C1–C8 | |
| 7. Intertransversarii | C1–C8 | |
| 8. Scaleni | C3–C8 | |
| 9. Sternocleidomastoid | Accessory, C2 | |
| 10. Obliquus capitis inferior | C1 | |
| 11. Rotatores breves | C1–C8 | |
| 12. Rotatores longi | C1–C8 | |
| 13. Longus colli | C2–C6 | |
| Rotation* of neck (muscles on one side contract) | 1. Levator scapulae (face moves to same side) | C3, C4 |
| Dorsal scapular | ||
| 2. Splenius cervicis (face moves to same side) | C4–C6 | |
| 3. Iliocostalis cervicis (face moves to same side) | C6–C8 | |
| 4. Longissimus cervicis (face moves to same side) | C6–C8 | |
| 5. Semispinalis cervicis (face moves to same side) | C1–C8 | |
| 6. Multifidus (face moves to opposite side) | C1–C8 | |
| 7. Intertransversarii (face moves to same side) | C1–C8 | |
| 8. Scaleni (face moves to opposite side) | C3–C8 | |
| 9. Sternocleidomastoid (face moves to opposite side) | Accessory, C2 | |
| 10. Obliquus capitis inferior (face moves to same side) | C1 | |
| 11. Rotatores brevis (face moves to same side) | C1–C8 | |
| 12. Rotatores longi (face moves to same side) | C1–C8 |
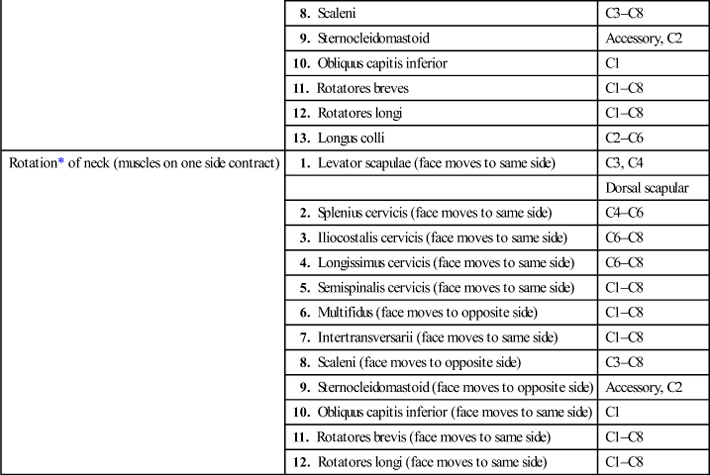
*Occurs in conjunction with side flexion owing to direction of facet joints.
1, Splenius capitis. 2, Splenius cervicis. 3, Semispinalis cervicis and capitis. 4, Multifidus and rotatores. 5, Longissimus capitis. 6, Longissimus cervicis. 7, Levator scapulae. 8, Scalenus posterior. 9, Scalenus medius. 10, Scalenus anterior. 11, Sternocleidomastoid. 12, Trapezius.
Scanning Examination
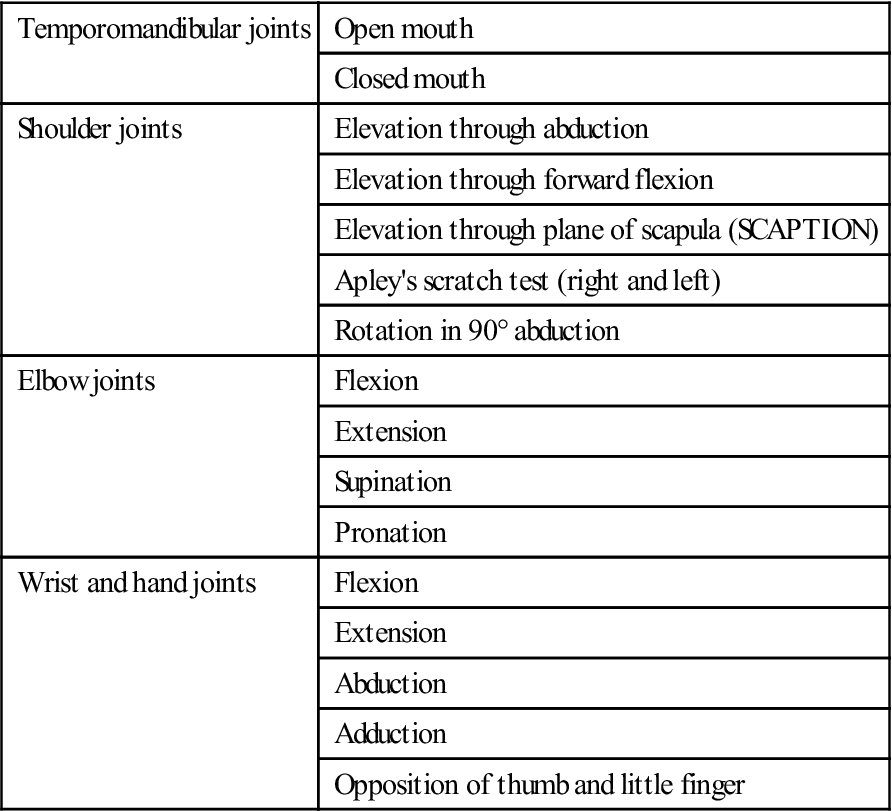
Peripheral Joint Scan
After the resisted isometric movements to the cervical spine have been completed, a peripheral joint scanning examination is performed to rule out obvious pathology in the extremities and to note areas that may need more detailed assessment.1 The following joints are scanned bilaterally:
Temporomandibular Joints.
The examiner checks the movement of the joints by placing the index or little fingers in the patient’s ears (Figure 3-28). The pulp aspect of the finger is placed forward to feel for equality of movement of the condyles of the temporomandibular joints and for clicking or grinding as well as to ensure that the ears are clear. Pain or tenderness, especially on closing the mandible, usually indicates posterior capsulitis. As the patient opens the mouth, the condyle normally moves forward. To open the mouth fully, the condyle must rotate and translate equally bilaterally. If this does not occur, mouth opening will be limited and/or deviation of the mandible will occur (see Chapter 4). The examiner should observe the patient as he or she opens and closes the mouth and should watch for any deviation during the movement.

Shoulder Girdle.
The examiner quickly scans this complex of joints (glenohumeral, acromioclavicular, sternoclavicular and “scapulothoracic” joint) by asking the patient to actively elevate each arm through abduction, followed by active elevation through forward flexion and elevation through the plane of the scapula (SCAPTION). In addition, the examiner quickly tests medial and lateral rotation of each shoulder with the arm at the side and with the arm abducted to 90°. Any pattern of restriction should be noted. If the patient is able to reach full abduction without difficulty or pain, the examiner may decide that there is no problem with the shoulder complex (see Chapter 5).
Elbow Joints.
The elbow joints are actively moved through flexion, extension, supination, and pronation. Any restriction of movement or abnormal signs and symptoms should be noted, because they may be indicative of pathology (see Chapter 6).
Wrist and Hand.
The patient actively performs flexion, extension, and radial and ulnar deviation of the wrist. Active movements (flexion, extension, abduction, adduction, and opposition) are performed for the fingers and thumb. These actions can be accomplished by having the patient make a fist and then spread the fingers and thumb wide. Again, any alteration in signs and symptoms or restriction of motion should be noted (see Chapter 7).
Myotomes
Having completed the peripheral joint scanning examination, the examiner should then determine muscle power and possible neurological weakness originating from the nerve roots in the cervical spine by testing the myotomes (Table 3-16 and Figure 3-29). Myotomes are tested by resisted isometric contractions with the joint at or near the resting position. As with the resisted isometric movements previously mentioned, the examiner should position the seated patient and say, “Don’t let me move you,” so that an isometric contraction is obtained.
TABLE 3-16
| Nerve Root | Test Action | Muscles* |
| C1–C2 | Neck flexion | Rectus lateralis, rectus capitis anterior, longus capitis, longus coli, longus cervicis, sternocleidomastoid |
| C3 | Neck side flexion | Longus capitis, longus cervicis, trapezius, scalenus medius |
| C4 | Shoulder elevation | Diaphragm, trapezius, levator scapulae, scalenus anterior, scalenus medius |
| C5 | Shoulder abduction | Rhomboid major and minor, deltoid, supraspinatus, infraspinatus, teres minor, biceps, scalenus anterior and medius |
| C6 | Elbow flexion and wrist extension | Serratus anterior, latissimus dorsi, subscapularis, teres major, pectoralis major (clavicular head), biceps, coracobrachialis, brachialis, brachioradialis, supinator, extensor carpi radialis longus, scalenus anterior, medius and posterior |
| C7 | Elbow extension and wrist flexion | Serratus anterior, latissimus dorsi, pectoralis major (sternal head), pectoralis minor, triceps, pronator teres, flexor carpi radialis, flexor digitorum superficialis, extensor carpi radialis longus, extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, scalenus medius and posterior |
| C8 | Thumb extension and ulnar deviation | Pectoralis major (sternal head), pectoralis minor, triceps, flexor digitorum superficialis, flexor digitorum profundus, flexor pollicis longus, pronator quadratus, flexor carpi ulnaris, abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, extensor indicis, abductor pollicis brevis, flexor pollicis brevis, opponens pollicis, scalenus medius and posterior |
| T1 | Hand intrinsics | Flexor digitorum profundus, intrinsic muscles of the hand (except extensor pollicis brevis), flexor pollicis brevis, opponens pollicis |
*Muscles listed may be supplied by additional nerve roots; only primary nerve root sources are listed.


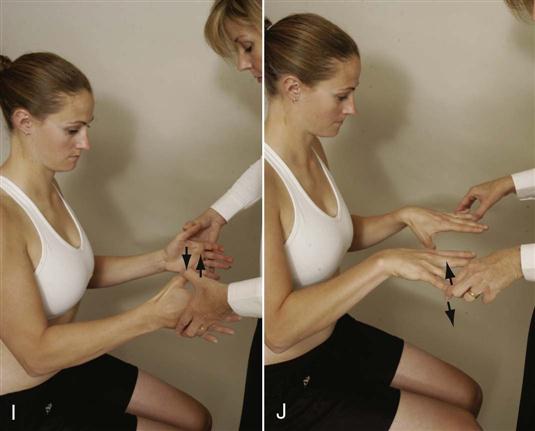
 Figure 3-29 Positioning to test myotomes.
Figure 3-29 Positioning to test myotomes.A, Neck flexion (C1, C2). B, Neck side flexion to the left (C3). C, Shoulder elevation (C4). D, Shoulder abduction (C5). E, Elbow flexion (C6). F, Wrist extension (C6). G, Elbow extension (C7). H, Wrist flexion (C7). I, Thumb extension (C8). J, Finger abduction (T1).
The contraction should be held for at least 5 seconds so that weakness, if any, can be noted. Where applicable, both sides are tested at the same time to provide a comparison. If possible, the examiner must not apply pressure over the joints, because this action may mask symptoms if the joints are tender.
To test neck flexion (C1 to C2 myotome), the patient’s head should be slightly flexed. The examiner applies pressure to the forehead while stabilizing the trunk with a hand between the scapulae (see Figure 3-29, A). The examiner should ensure the neck does not extend when applying pressure to the forehead. To test neck side flexion (C3 myotome and cranial nerve XI), the examiner places one hand above the patient’s ear and applies a side flexion force while stabilizing the trunk with the other hand on the opposite shoulder (see Figure 3-29, B). Both right and left side flexion must be tested.
The examiner then asks the patient to elevate the shoulders (C4 myotome and cranial nerve XI) to about half of full elevation. The examiner applies a downward force on both of the patient’s shoulders while the patient attempts to hold them in position (see Figure 3-29, C). The examiner should ensure that the patient is not “bracing” the arms against the thighs if testing is done while sitting.
To test shoulder abduction (C5 myotome), the examiner asks the patient to elevate the arms to about 75° to 80° in the scapular plane with the elbows flexed to 90° and the forearms pronated or in neutral (see Figure 3-29, D). The examiner applies a downward force on the humerus while the patient attempts to hold the arms in position. To prevent rotation, the examiner places his or her forearms over the patient’s forearms while applying pressure to the humerus.
To test elbow flexion and extension, the examiner asks the patient to put the arms by the sides with the elbows flexed to 90° and forearms in neutral. The examiner applies a downward isometric force (see Figure 3-29, E) to the forearms to test the elbow flexors (C6 myotome) and an upward isometric force (see Figure 3-29, G) to test the elbow extensors (C7 myotome). For testing of wrist movements (extension, flexion, ulnar deviation) the patient’s arms are by the side; elbows at 90°; forearms pronated; and wrists, hands, and fingers in neutral. The examiner applies a downward force (see Figure 3-29, F) to the hands to test wrist extension (C6 myotome), and an upward force (see Figure 3-29, H) to test wrist flexion (C7 myotome). To apply a lateral force (radial deviation) to test ulnar deviation (C8 myotome), the clinician stabilizes the patient’s forearm with one hand and applies a radial deviation force to the side of the hand.
In the test for thumb extension (C8 myotome), the patient extends the thumb just short of full range of motion (see Figure 3-29, I). The examiner applies an isometric force to bring the thumbs into flexion. To test hand intrinsics (T1 myotome), the patient squeezes a piece of paper between the fingers while the examiner tries to pull it away; the patient may squeeze the examiner’s fingers, or the patient may abduct the fingers slightly with the examiner isometrically adducting them (see Figure 3-29, J).
Sensory Scanning Examination
The examiner then tests sensation by doing a sensory scanning examination. This “sensory scan” is accomplished by running relaxed hands over the patient’s head (sides and back); down over the shoulders, upper chest, and back; and down the arms, being sure to cover all aspects of the arm. If any difference is noted between the sides in this “sensation scan,” the examiner may then use a pinwheel, pin, cotton batting, or brush (or a combination of these) to map out the exact area of sensory difference and to determine if any sensory difference is due to a nerve root (see later section on reflexes and cutaneous distribution), peripheral nerve, or some other neurological deficit. The sensory scanning examination may also include the testing of reflexes, especially the deep tendon reflexes, to test for upper and lower neuron pathology and pathological reflexes for upper motor neuron pathology, and the performance of selected neurodynamic tests (e.g., upper limb tension test, slump test) if peripheral nerve irritability is suspected.
Functional Assessment
If, in the history, the patient has complained of functional difficulties or the examiner suspects some functional impairment, a series of functional tests or movements may be performed to determine the patient’s functional capacity, keeping in mind the patient’s age and health. These tests may include activities of daily living (ADLs) such as the following:
Breathing.
Normal, unlabored breathing should be seen with the mouth closed. There should be no gulping or gasping.
Swallowing.
This is a complex movement involving muscles of the lips, tongue, jaw, soft palate, pharynx, and larynx as well as the suprahyoid and infrahyoid muscles.
Looking Up at the Ceiling.
At least 40° to 50° of neck extension is usually necessary for everyday activities. If this range is not available, the patient will bend the back or the knees, or both, to obtain the desired range.
Looking Down at Belt Buckle or Shoe Laces.
At least 60° to 70° of neck flexion is necessary. If this range is not available, the patient will flex the back to complete the task.
Shoulder Check.
At least 60° to 70° of cervical rotation is necessary. If this range is not available, the patient will rotate the trunk to accomplish this task.
Tuck Chin In.
This action produces upper cervical flexion with lower cervical extension.73
Poke Chin Out.
This action produces upper cervical extension with lower cervical flexion.73
Neck Strength.
In athletes, neck strength should be approximately 30% of body weight to decrease chance of injury.75
Paresthesia.
Paresthesia, especially referred to the hands, may make cooking and handling utensils particularly difficult or even dangerous.
Table 3-17 lists functional strength tests that can give the examiner some indication of the patient’s functional strength capacity. For flexion, if the jaw juts forward at the beginning of the movement, it indicates an imbalance pattern of strong sternocleidomastoid and weak deep neck reflexors.13
TABLE 3-17
Functional Strength Testing of the Cervical Spine
| Starting Position | Action | Functional Test* |
| Supine lying | Lift head keeping chin tucked in (neck flexion) | |
| Prone lying | Lift head backward (neck extension) | |
| Side lying (pillows under head so head is not side flexed) | Lift head sideways away from pillow (neck side flexion) (must be repeated for other side) | |
| Supine lying | Lift head off bed and rotate to one side keeping head off bed or pillow (neck rotation) (must be repeated both ways) |
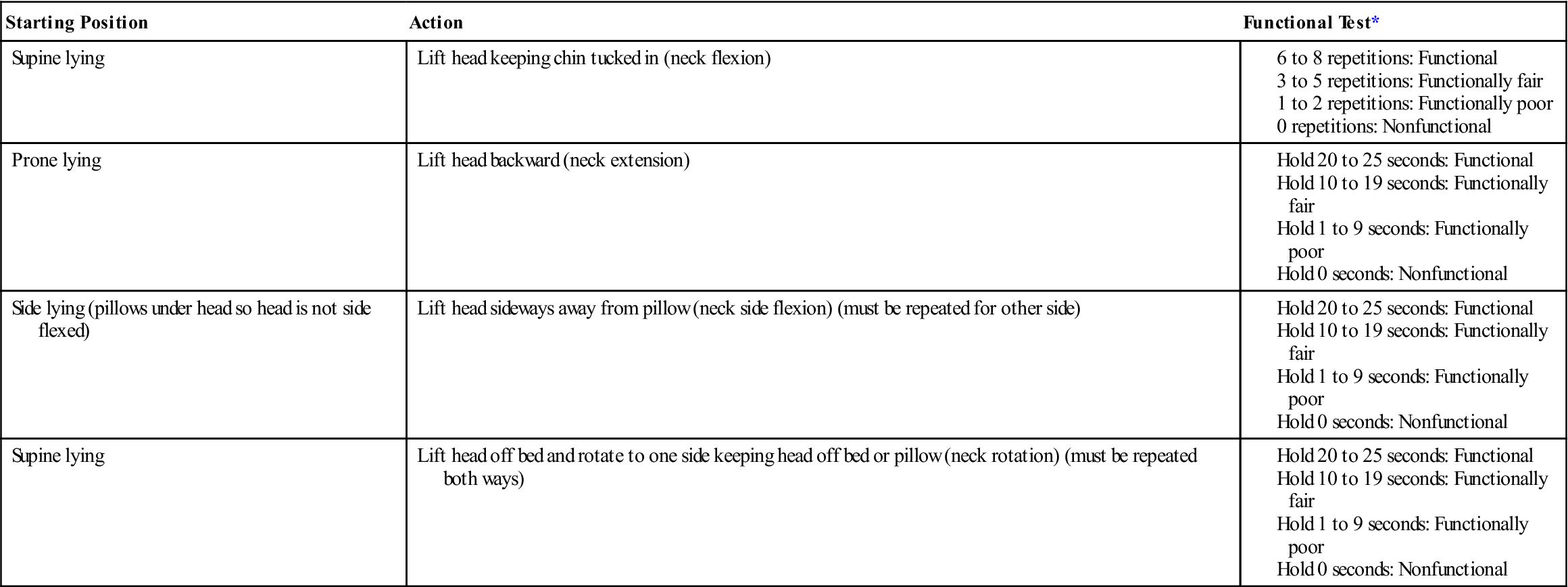
*Younger patients should be able to do the most repetitions and for the longest time; with age, time and repetitions decrease.
Adapted from Palmer ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, J.B. Lippincott, pp. 181–182.
Pinfold and others76,77 developed the Whiplash Disability Questionnaire (WDQ) (Figure 3-30) to assess the impact of whiplash associated disorders including social and emotional problems. Vernon and Mior78 have developed a numerical scoring functional test called the Neck Disability Index (NDI)79,80 (Figure 3-31), which is a modification of the Oswestry low back pain index.81 This index and similar tests (e.g., Bournemouth Questionnaire [Figure 3-32], the Copenhagen Neck Functional Disability Scale,82 and the Norwick Park Neck Pain Questionnaire83,84) can be used to detect change in patients over time.85,86
Special Tests
There are several special tests that may be performed if the examiner believes they are relevant and to help confirm a diagnosis. Some of these tests should always be performed (e.g., instability tests, vertebral artery tests), especially if treatment is to be given to the upper cervical spine; while others should be performed only if the examiner wants to use them as confirming tests. Some tests are provocative and should only be used if the examiner wants to cause symptoms. Other tests relieve symptoms and are used when the symptoms are present. The reliability of many of these tests commonly depends on the experience and skill of the examiner and whether the patient is sufficiently relaxed to allow the test to be performed.87,88
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the cervical spine are available electronically on the Evolve website (see Appendix 3-1).
APPENDIX 3-1
| BICEPS BRACHII REFLEX | ||
| Specificity | Sensitivity | Odds Ratio |
| BRACHIAL COMPRESSION TEST | ||
| Specificity | Sensitivity | Odds Ratio |
| BRACHIAL PLEXUS TENSION TEST | |
| Reliability | Validity |
| BRACHIORADIALIS REFLEX | ||
| Specificity | Sensitivity | Odds Ratio |
| CANADIAN C-SPINE RULE | |
| Specificity | Sensitivity |
| CERVICAL ROTATION LATERAL FLEXION TEST | |
| Reliability | Validity |
| DECREASED VIBRATION OF PIN PRICK | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| DISTRACTION TEST | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| EXTENSION ROTATION TEST FOR LEFT VERTEBRAL ARTERY | ||
| Specificity | Sensitivity | Odds Ratio |
| EXTENSION ROTATION TEST FOR RIGHT VERTEBRAL ARTERY | ||
| Specificity | Sensitivity | Odds Ratio |
| FORAMINAL COMPRESSION (SPURLING’S) TEST | ||
| Specificity | Sensitivity | Odds Ratio |
| MANUAL EXAMINATION | ||
| Specificity | Sensitivity | Odds Ratio |
| NECK COMPRESSION TEST | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| NECK DISABILITY INDEX | ||||
| Reliability | Validity | Specificity | Sensitivity | Odds Ratio |
| NECK FLEXOR MUSCLE ENDURANCE TEST |
| Reliability |
| NEXUS | |
| Specificity | Sensitivity |
| PALPATION OF THE CONGENITAL BLOCK | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |
| PALPATION OVER THE FACET JOINTS IN THE CERVICAL SPINE | ||
| Specificity | Sensitivity | Odds Ratio |
| PATIENT-SPECIFIC FUNCTIONAL SCALE | |||
| Reliability | Specificity | Sensitivity | Odds Ratio |

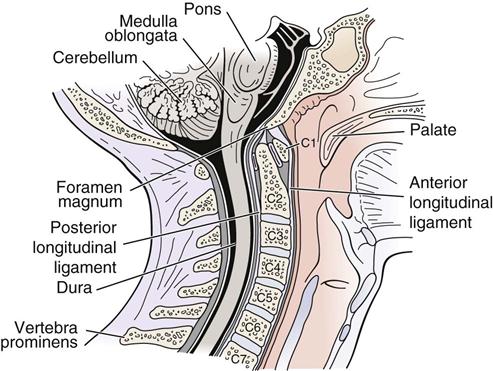
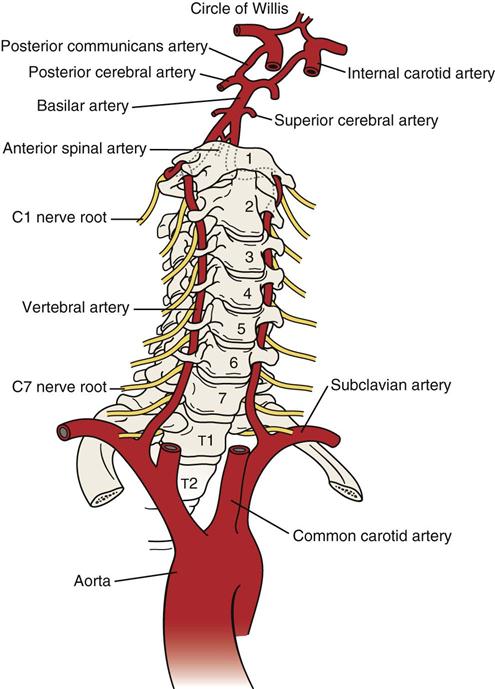
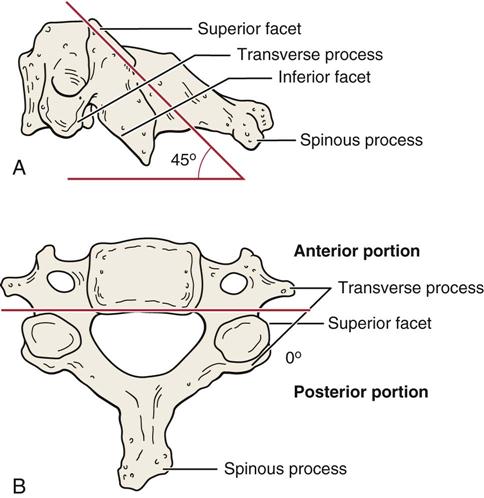
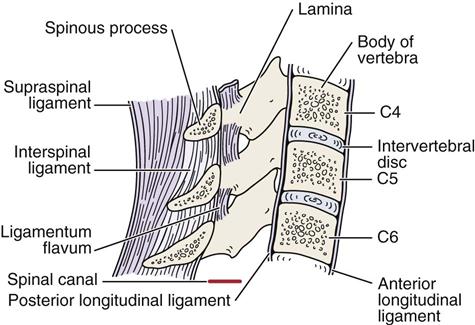
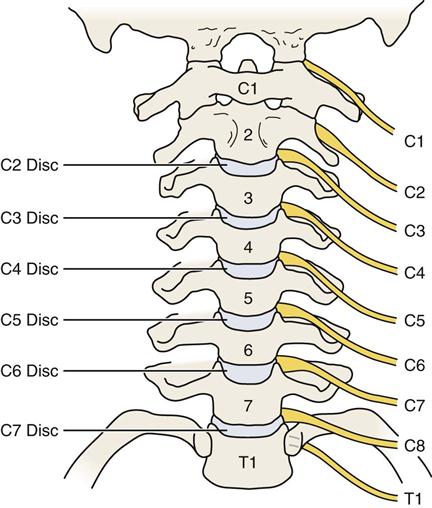
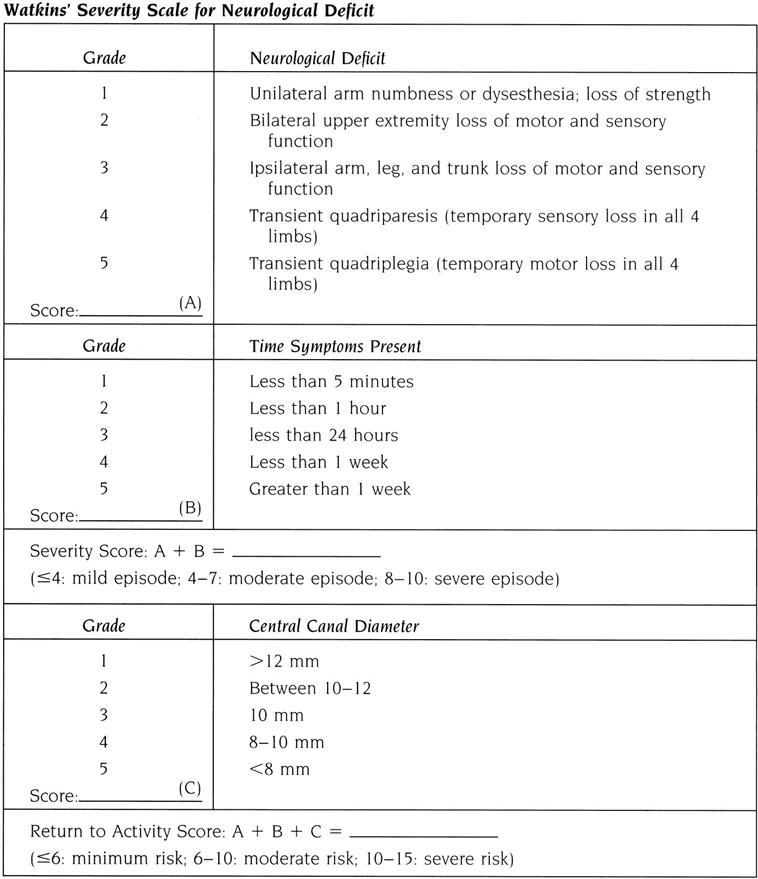
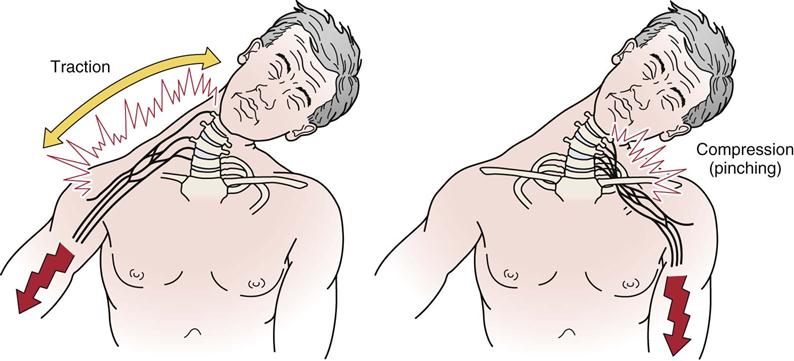
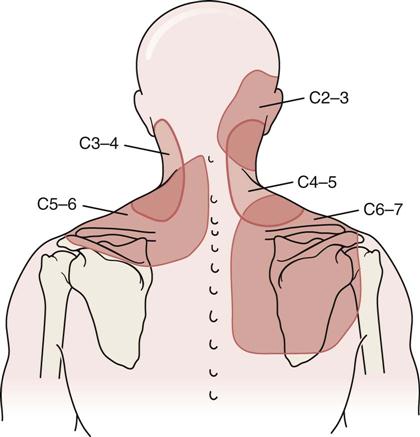
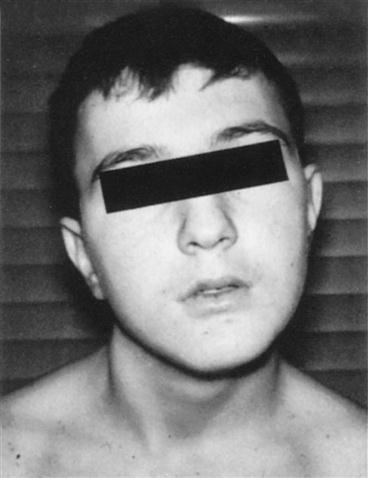

 Figure 3-23
Figure 3-23