Chapter 45 Cervical Skip Corpectomy
The ventral approach to the cervical spine was first suggested by Dr. Leroy Abbott in 1952. The approach was used and subsequently described by Bailey and Badgley.1 During the late 1950s and 1960s many approaches and techniques were defined to obtain a successful neural decompression and cervical spine arthrodesis.2 All these frontier studies focused on anterior cervical discectomy and arthrodesis.
Evolution of new techniques facilitated the complex surgical procedures, leading surgeons to use more aggressive techniques in cases with traumatic, degenerative, infectious, and neoplastic disorders. As a result, the first cervical corpectomy procedures were performed in 1970s. With time cervical ventral and dorsal plating techniques were developed.3
Cervical corpectomy is an effective procedure decompressing the ventral spinal cord. The existing literature indicates that the success rate usually is good for single-level or two-level cervical corpectomy, but not for multilevel corpectomy.4–15 On the other hand, although this surgery is associated with good results in terms of neurologic recovery, many complications, such as strut graft fracture, graft pistoning, graft dislodgement, hardware failure, and pseudoarthrosis, are also part of its history.
Vaccaro et al. demonstrated high rates of early construct failure in multilevel fusions: 9% for two-level corpectomy, and 50% for three-level corpectomy.15 A similar high rate of construct failure after multilevel corpectomy was reported by others as well.6,7,10,11,15–19 The reported high rate of failure indicates that reconstruction of a multilevel corpectomy defect in the cervical spine remains a challenge.
Biomechanics of Cervical Corpectomy
The evidence of failure of long constructs has been investigated in biomechanical studies.20–22 Cadaveric biomechanical studies showed that the longer plate generates greater motions at the fusion sites under physiologic loads because of its longer lever arm,23 and that the stabilizing potential indices significantly decrease after fatigue for the three-level corpectomy, but not for the one-level corpectomy.16,17,23–25 This explains the lesser rate of construct failure in one-level cervical corpectomies.
Cervical corpectomy results in a posterior shift of the center of rotation, as the anterior aspect of the spine is cut. Addition of an anterior cervical plate shifts the center of rotation to the anterior, thus changing the loading pattern.16,17,24 In other words, whereas the stand-alone strut graft is loaded in flexion and unloaded in extension,16,17 the addition of a plate completely reverses the loading pattern. The outcome is reversal of the loading pattern in anterior-plated long-strut grafts so that loading of the graft does not occur under flexion moments, and excessive compression of the graft occurs under extension loads, resulting in the graft pistoning into the caudal vertebral end plate and, subsequently, in plate kicking.16,17
Alternative Solutions
Based on clinical experiences and biomechanical facts, many alternative techniques have been developed to avoid graft plate-related problems in cases of multilevel corpectomy.4,6,8,13,26–30
Based on the evidence of the high stress in the lower end of the construct, the use of a buttress (junctional) plate alone was recommended. However, Riew et al.27 and MacDonald et al.8 reported high rates of complication after the use of a buttress plate alone in multilevel corpectomy. They recommended that the buttress plate be supplemented with posterior fixation.8,27,30
Others focused on the 360-degree fixation using long plates.4,6,13,26 However, the 360-degree procedure is a lengthy, sometimes staged procedure.
Different combinations of multilevel anterior cervical discectomy and fusion (ACDF) with or without corpectomies are other alternatives. As ventral alternative approaches to three-level corpectomy, Rhee and Riew31 proposed (1) multilevel ACDF, (2) single corpectomy combined with additional ACDFs, and (3) two single-level corpectomies separated by an intact intervening vertebra. As another alternative, Ozer et al. described an open-window corpectomy technique.32
Indications of Skip Corpectomy
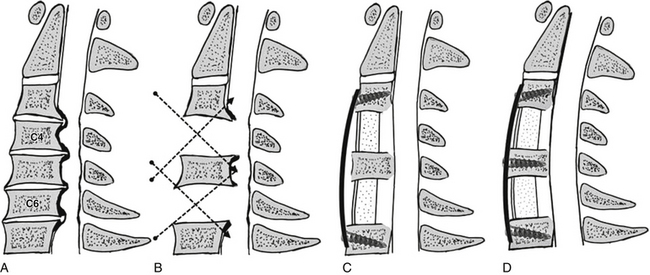
The skip corpectomy is indicated and is applicable in compressions extending from C3-4 to C6-7, particularly when the area of compression at the C5 level is confined to the adjacent disc spaces (Fig. 45-1A). This is so because skip corpectomy allows optimal decompression of the C3-4, C4-5, C5-6, and C6-7 intervertebral disc levels and C4 and C6 vertebral body levels (Fig. 45-1B). However, the limited work angle does not allow for optimum decompression of the posterior aspect of the C5 vertebral body, as seen in continuing ossification of the posterior longitudinal ligament (OPLL) cases. Note, however, that the surgeon may change strategy during the procedure and can add a C5 corpectomy if the decompression behind the C5 vertebral body is not satisfactory. Such an additional C5 corpectomy means a three-level corpectomy and should be combined with a posterior stabilization procedure.
Skip Corpectomy Technique
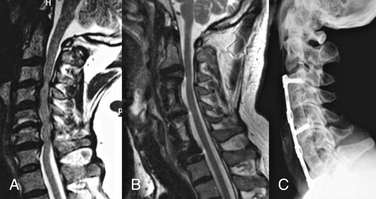
The skip corpectomy technique is exemplified by a C4 and C6 corpectomy, C5 osteophytectomy, and decompression of dorsal-rostral and dorsal-caudal aspects of the C5 vertebra. Preservation of the C5 vertebral body and the use of this vertebra for screw fixation are the most important aspects of this technique. Reconstruction can be performed using either iliac crest autograft or fibula allograft. After placement of the C3-5 and C5-7 bone grafts, a fixed rigid ventral cervical spine plate is placed (Fig. 45-1C). The plate is contoured in lordosis. The intervening vertebral body that is left after C4 and C6 decompression (i.e., the C5 vertebral body) serves as an intermediate point of construct fixation. The plate is first secured at the rostral and caudal ends (the C3 and C7 vertebral bodies). Next, screws are placed into the intervening vertebral body (the C5 vertebral body). As the C5 vertebral body screws are tightened, the spine is “brought to the cervical plate” (Figs. 45-1D and 45-2). Figure 45-3 shows preoperative and postoperative images of a patient who underwent skip corpectomy.
Advantages of Skip Corpectomy
The skip corpectomy technique achieves four healing surfaces, representing fewer than an equivalent number of multilevel ACDFs (eight surfaces), while avoiding problems with long-strut grafts. The fixation is obtained at the top, bottom, and middle of the constructs. The technique was suggested in recent years.31,33,34 Ashkenazi et al. reported results after skip corpectomy, what they called hybrid decompression, in 13 cases.34 They noted fusion in all cases and experienced mechanical failure of the construct in only one case (4%). Using this technique, Agbi and Paquette33 reported successful outcomes in four cases. The results of the current series are in line with those reported by Ashkenazi et al.34 Dalbayrak et al. reported a high fusion rate (100%) and a low graft hardware-related complication rate (3.4%) using skip corpectomy.35 The technique is biomechanically superior to ventral plating alone for three-level corpectomy.
Singh et al.36 compared the biomechanical aspects of different hybrid discectomy and corpectomy models and reported that the increased rigidity afforded by segmental fixation may significantly decrease the likelihood of plate dislodgement in the setting of anterior instrumentation alone. Addition of intermediate points of fixation also provided a better translational stability.
In a recent biomechanical study, Yüksel et al. compared the skip corpectomy with standard three-level corpectomy.37 They reported that skip corpectomy allowed a slightly smaller range of motion during lateral bending and axial rotation than did standard three-level corpectomy. However, high pull-out forces still occurred at superior and inferior vertebral screws during axial rotation. They concluded that skip corpectomy provided a better stability during lateral bending and axial rotation movements of the neck, and because of the high pull-out forces seen in the superior and caudal screws during the axial rotation, the patient’s axial rotation should be restrained.
Dalbayrak S., Yilmaz M., Naderi S. Skip corpectomy: an alternative approach to multilevel cervical spondylotic myelopathy and ossified posterior longitudinal ligament. J Neurosurg Spine. 2010;12:33-38.
DiAngelo D.J., Foley K.T., Vossel K.A., et al. Anterior cervical plating reverses load transfer through multilevel strut-grafts. Spine (Phila Pa 1976). 2000;25:783-795.
Naderi S., Alberstone C.D., Rupp F.W., et al. Cervical spondylotic myelopathy treated with corpectomy: technique and results in 44 patients. Neurosurg Focus. 1996;1(6):e5.
Ozer A.F., Oktenoğlu B.T., Sarioğlu A.C. A new surgical technique: open-window corpectomy in the treatment of ossification of the posterior longitudinal ligament and advanced cervical spondylosis: technical note. Neurosurgery. 1999;45:1481-1485.
Panjabi M.M., Isomi T., Wang J.L. Loosening at the screw-vertebra junction in multilevel anterior cervical plate constructs. Spine. 1999;24:2383-2388.
Sasso R.C., Ruggiero R.A.Jr., Reilly T.M., Hall P.V. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976). 2003;28:140-142.
Vaccaro A.R., Falatyn S.P., Scuderi G.J., et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410-415.
Wang J.L., Panjabi M.M., Isomi T. The role of bone graft force in stabilizing the multilevel anterior cervical spine plate system. Spine (Phila Pa 1976). 2000;25:1649-1654.
1. Bailey R.W., Badgley C.E. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg [Am]. 1960;42:565-594.
2. Robinson R.A., Smith G.W. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955;96:223.
3. Gonugunta V., Krishnaney A.A., Benzel E.C. Anterior cervical plating. Neurol India. 2005;53:424-432.
4. Daubs M.D. Early failures following cervical corpectomy reconstruction with titanium mesh cages and anterior plating. Spine (Phila Pa 1976). 2005;30:1402-1406.
5. Eleraky M.A., Llanos C., Sonntag V.K. Cervical corpectomy: report of 185 cases and review of the literature. J Neurosurg. 1999;90(1 Suppl):35-41.
6. Hee H.T., Majd M.E., Holt R.T., et al. Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech. 2003;16:1-8.
7. Jones J., Yoo J., Hart R. Delayed fracture of fibular strut allograft following multilevel anterior cervical spine corpectomy and fusion. Spine (Phila Pa 1976). 2006;31:E595-E599.
8. Macdonald R.L., Fehlings M.G., Tator C.H., et al. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg. 1997;86:990-997.
9. Mayr M.T., Subach B.R., Comey C.H., et al. Cervical spinal stenosis: outcome after anterior corpectomy, allograft reconstruction, and instrumentation. J Neurosurg. 2002;96(1 Suppl):10-16.
10. Naderi S., Alberstone C.D., Rupp F.W., et al. Cervical spondylotic myelopathy treated with corpectomy: technique and results in 44 patients. Neurosurg Focus. 1996;1(6):e5.
11. Sasso R.C., Ruggiero R.A.Jr., Reilly T.M., Hall P.V. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976). 2003;28:140-142.
12. Swank M.L., Lowery G.L., Bhat A.L., McDonough R.F. Anterior cervical allograft arthrodesis and instrumentation: multilevel interbody grafting or strut graft reconstruction. Eur Spine J. 1997;6:138-143.
13. Thalgott J.S., Xiongsheng C., Giuffre J.M. Single stage anterior cervical reconstruction with titanium mesh cages, local bone graft, and anterior plating. Spine (Phila Pa 1976). 2003;3:294-300.
14. Thongtrangan I., Balabhadra R.S., Kim D.H. Management of strut graft failure in anterior cervical spine surgery. Neurosurg Focus. 2003;15:E4.
15. Vaccaro A.R., Falatyn S.P., Scuderi G.J., et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410-415.
16. Foley K.T., Smith M.M., Wiles D.A. Anterior cervical plating does not prevent strut graft displacement in multilevel cervical corpectomy. Presented at the 25th Annual Meeting of the Cervical Spine Research Society. CA: Rancho Mirage; December 4–6, 1997.
17. Foley K.T., DiAngelo D.J., Rampersaud Y.R., et al. The in vitro effects of instrumentation on multilevel cervical strut-graft mechanics. Spine (Phila Pa 1976). 1999;24:2366-2376.
18. Wang J.C., Hart R.A., Emery S.E., Bohlman H.H. Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine (Phila Pa 1976). 2003;28:1016-1021.
19. Zdeblick T., Bohlman H. Cervical kyphosis and myelopathy. Treatment by anterior corpectomy and strut-grafting. J Bone Joint Surg [Am]. 1989;71:170-182.
20. Kirkpatrick J.S., Levy J.A., Carillo J., Moeini S.R. Reconstruction after multilevel corpectomy in the cervical spine. A sagittal plane biomechanical study. Spine (Phila Pa 1976). 1999;24:1186-1190.
21. Porter R.W., Crawford N.R., Chamberlain R.H., et al. Biomechanical analysis of multilevel cervical corpectomy and plate constructs. J Neurosurg. 2003;99(1 Suppl):98-103.
22. Wang J.L., Panjabi M.M., Isomi T. The role of bone graft force in stabilizing the multilevel anterior cervical spine plate system. Spine (Phila Pa 1976). 2000;25:1649-1654.
23. Isomi T., Panjabi M.M., Wang J.L., et al. Stabilizing potential of anterior cervical plates in multilevel corpectomies. Spine (Phila Pa 1976). 1999;24:2219-2223.
24. DiAngelo D.J., Foley K.T., Vossel K.A., et al. Anterior cervical plating reverses load transfer through multilevel strut-grafts. Spine (Phila Pa 1976). 2000;25:783-795.
25. Panjabi M.M., Isomi T., Wang J.L. Loosening at the screw-vertebra junction in multilevel anterior cervical plate constructs. Spine (Phila Pa 1976). 1999;24:2383-2388.
26. Edwards C.C., Riew K.D., Anderson P.A., et al. Cervical myelopathy: current diagnostic and treatment strategies. Spine J. 2003;3:68-81.
27. Riew K.D., Sethi N.S., Devney J., et al. Complications of buttress plate stabilization of cervical corpectomy. Spine (Phila Pa 1976). 1999;24:2404-2410.
28. Stewart T.J., Steinmetz M.P., Benzel E.C. Techniques for the ventral correction of postsurgical cervical kyphotic deformity. Neurosurgery. 2005;56(Suppl 1):191-195.
29. Stewart T.J., Schlenk R.P., Benzel E.C. Multiple level discectomy and fusion. Neurosurgery. 2007;60(Supp1 1):S143-S148.
30. Vanichkachorn J.S., Vaccaro A.R., Silveri C.P., Albert T.J. Anterior junctional plate in the cervical spine. Spine (Phila Pa 1976). 1998;23:2462-2467.
31. Rhee J.M., Riew K.D. Surgical management of cervical myelopathy. J Neurol Sci (Turkish). 2005;22:359-373.
32. Ozer A.F. Oktenoğlu BT, Sarioğlu AC: A new surgical technique: open-window corpectomy in the treatment of ossification of the posterior longitudinal ligament and advanced cervical spondylosis: technical note. Neurosurgery. 1999;45:1481-1485.
33. Agbi C.B., Paquette S. Skip Corpectomies for Anterior Cervical Decompression: Technical Note. spineuniverse.com/displayarticle.php/article570.html. 02.07.2008
34. Ashkenazi E., Smorgick Y., Rand N., et al. Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosurg Spine. 2005;3:205-209.
35. Dalbayrak S., Yilmaz M., Naderi S. Skip corpectomy: an alternative approach to multilevel cervical spondylotic myelopathy and ossified posterior longitudinal ligament. J Neurosurg Spine. 2010;12:33-38.
36. Singh K., Vaccaro A.R., Kim J., et al. Enhancement of stability following anterior cervical corpectomy: a biomechanical study. Spine (Phila Pa 1976). 2004;29:845-849.
37. Yüksel Z, Yilmaz M, Baek S, et al: Biomechanics of cervical “skip” corpectomy versus standard multilevel corpectomy. Presented at 34th Annual Meeting of Cervical Spine Research Society, The Breakers, Palm Beach, FL, November 30–December 2, 2006.