Central regulation of ventilation
Ventilation is regulated to maintain optimal and unchanging levels of pH, CO2, and O2 in the blood. This regulation is provided via the respiratory center, which receives afferent input from chemical stimuli and peripheral chemoreceptors. The respiratory center is composed of a group of nuclei in four major areas within the medulla and pons (Table 25-1).
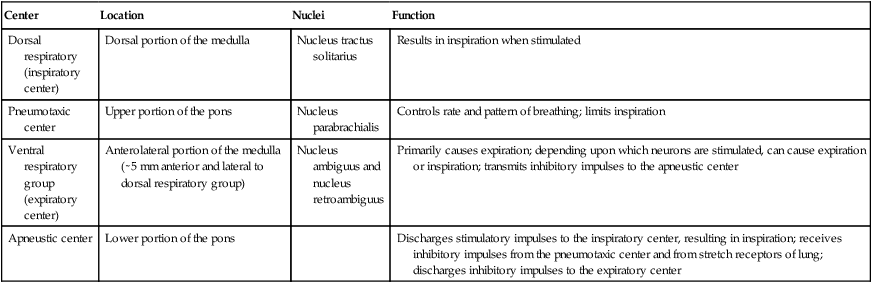
Table 25-1
Neurons within the Medulla and Pons That Constitute the Respiratory Center
| Center | Location | Nuclei | Function |
| Dorsal respiratory (inspiratory center) | Dorsal portion of the medulla | Nucleus tractus solitarius | Results in inspiration when stimulated |
| Pneumotaxic center | Upper portion of the pons | Nucleus parabrachialis | Controls rate and pattern of breathing; limits inspiration |
| Ventral respiratory group (expiratory center) | Anterolateral portion of the medulla (∼5 mm anterior and lateral to dorsal respiratory group) | Nucleus ambiguus and nucleus retroambiguus | Primarily causes expiration; depending upon which neurons are stimulated, can cause expiration or inspiration; transmits inhibitory impulses to the apneustic center |
| Apneustic center | Lower portion of the pons | Discharges stimulatory impulses to the inspiratory center, resulting in inspiration; receives inhibitory impulses from the pneumotaxic center and from stretch receptors of lung; discharges inhibitory impulses to the expiratory center |
Neural control
Inspiratory center
The inspiratory center, the site of basic respiratory drive, located dorsally in the medulla, extends the full length of the medulla (Figure 25-1). The neurons within the inspiratory center are located near the termination sites of afferent fibers from the glossopharyngeal (IX) and vagus (X) nerves. These neurons have intrinsic automaticity and normally fire for 2 sec, with a ramp effect of increasing efferent activity to the diaphragm until it abruptly ceases with a 3-sec pause before initiating a new cycle.
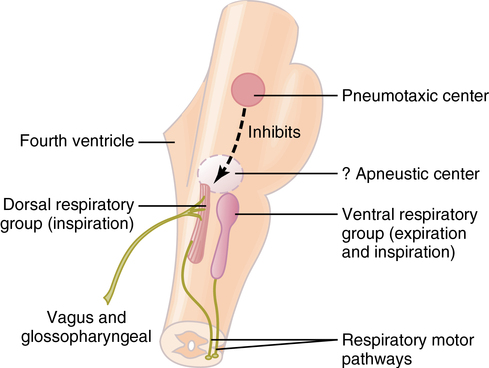
Expiratory center
The expiratory center extends the full length of the ventral medulla and stimulates the muscles of expiration (see Figure 25-1) but is normally quiescent because expiration is a passive process. With increased demand, the expiratory center sends efferent signals and stimulates the muscles of expiration (see Figure 25-1).
Apneustic center
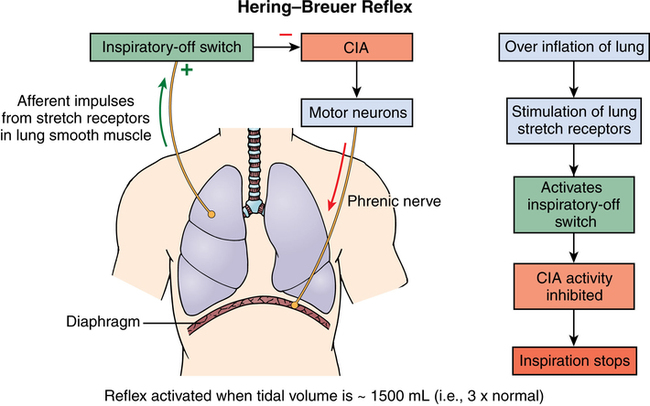
The apneustic center is located in the lower pons. Its role is to antagonize the effects of the pneumotaxic center, and it plays no role in normal respiration. In the Hering-Breuer reflex, bronchiolar stretch receptors feed back to the inspiratory center via the vagus nerve to limit lung overexpansion. This reflex plays a minimal role in normal ventilation but becomes active when tidal volume exceeds 1.5 L (Figure 25-2).
Chemical control
Central
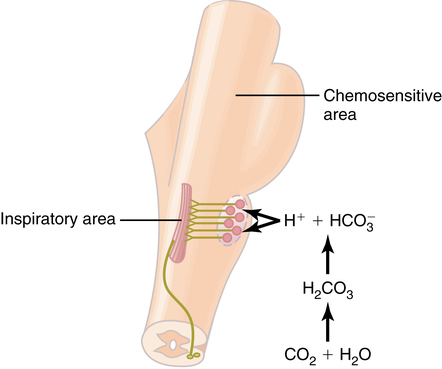
The chemosensitive area is located bilaterally in the medulla several microns beneath the ventral surface (Figure 25-3). This area is extremely sensitive to hydrogen ions (H+). However, H+ cross the blood-brain barrier poorly, and thus, CO2 indirectly controls this region through formation of carbonic acid with dissociation to H+. When stimulated, this chemosensitive area then stimulates the inspiratory center to increase the rate of rise of the ramp effect and, thus, increases the rate of respiration.
< ?xml:namespace prefix = "mml" />

Peripheral
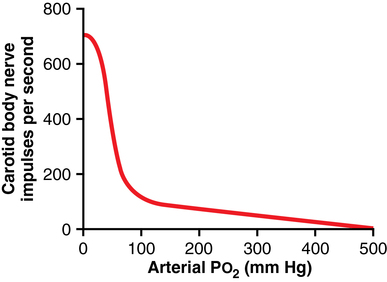
Peripheral chemoreceptors are located in the carotid bodies (cranial nerve IX) and aortic bodies (cranial nerve X). These areas of high blood flow are sensitive to changes in O2, CO2, and pH. They stimulate the inspiratory center when Pao2 decreases; the effect is greatest between 30 and 60 mm Hg (Figure 25-4).