Care of the Term Infant
Given that infants born before 37 weeks have even greater liability for problems, the recognition that true term status begins at about 39 weeks’ gestation has led the American College of Obstetrics and Gynecology (ACOG) and the American Academy of Pediatrics (AAP) to recommend that no infants be delivered electively before 39 weeks. ∗†
The mean birth weight of a term infant is approximately 3400 grams, or approximately 7 pounds, 7 ½ ounces. Mean length, which is sometimes difficult to measure accurately, is approximately 52 to 53 centimeters, or 20 inches, and head circumference averages 34 centimeters, or approximately 13.5 inches. Of note is the fact that birth weight in recent years has declined slightly, even though premature births have been declining. ∗
Approximately 10% of all infants need some assistance at birth (e.g., stimulation, oxygen), and approximately 1% need extensive assistance (e.g., positive pressure ventilation, fluids, drugs) at the time of birth. ∗
4. What are the critical skills needed by any individual called upon to resuscitate a neonate?
 The ability to rapidly and accurately evaluate the newborn’s condition
The ability to rapidly and accurately evaluate the newborn’s condition
 Knowledge of the risk factors that may predispose the neonate to resuscitation
Knowledge of the risk factors that may predispose the neonate to resuscitation
 Indications for neonatal resuscitation
Indications for neonatal resuscitation
 Skill in umbilical catheter placement
Skill in umbilical catheter placement
 Skill in insertion of chest tubes
Skill in insertion of chest tubes
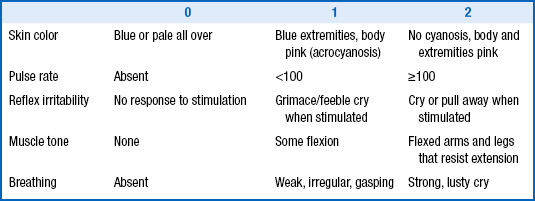
The Apgar score is determined at 1 and 5 minutes of life and consists of the measures listed in Table 1-1. These measures are scored 0, 1, or 2, then totaled.
It is rare for an infant to have an Apgar score of 10 (the highest possible score) in the absence of oxygen administration because the exposure of most newborn infants to the environmental temperature of the delivery room will cause some acrocyanosis of the hands and feet, reducing the potential score to 9. An Apgar score above 7 is considered good, one between 4 and 7 demands close observation, and one that is 3 or lower usually requires some intervention. Even with the changes that have occurred in modern medicine, the Apgar score has retained its value. ∗
When called to the delivery of a term infant, the clinician should first make sure that all possible tools that might be needed for resuscitation and maintenance of a thermal neutral environment are ready. Although the great majority of term infants in an uncomplicated pregnancy do not require any intervention, it is important to be prepared for any possibility. In addition, a number of other routine items are necessary. On arrival in the delivery room the following items should be checked:
 The radiant warmer should be turned on, and a temperature probe that can be attached to the skin should be available.
The radiant warmer should be turned on, and a temperature probe that can be attached to the skin should be available.
 Several dry towels and blankets should be heated under the radiant warmer for the infant.
Several dry towels and blankets should be heated under the radiant warmer for the infant.
 A resuscitation bag or a T-piece device should be available with masks of several sizes. If the gestational age of the infant is known, the most appropriate mask size can be chosen (typically a size 1 for term infants).
A resuscitation bag or a T-piece device should be available with masks of several sizes. If the gestational age of the infant is known, the most appropriate mask size can be chosen (typically a size 1 for term infants).
 An oxygen source should be available. In most instances resuscitation with 21% oxygen can be used initially if respiratory intervention is required.
An oxygen source should be available. In most instances resuscitation with 21% oxygen can be used initially if respiratory intervention is required.
 A laryngoscope and endotracheal (ET) tubes should be available. For the term infant, a 0 or 1 laryngoscope blade is appropriate, and a 3.5 FR ET tube should be used. Note: Although it may be easier to insert a smaller ET tube, this approach ignores the fact that work of breathing will be dramatically increased with a tube that is too small for the size of the infant.
A laryngoscope and endotracheal (ET) tubes should be available. For the term infant, a 0 or 1 laryngoscope blade is appropriate, and a 3.5 FR ET tube should be used. Note: Although it may be easier to insert a smaller ET tube, this approach ignores the fact that work of breathing will be dramatically increased with a tube that is too small for the size of the infant.
 Umbilical catheters, size 3.5 and 5 FR, should be available along with D10W fluid and lactated Ringer’s solution. Feeding tubes should also be available for insertion into the stomach to drain the contents or air.
Umbilical catheters, size 3.5 and 5 FR, should be available along with D10W fluid and lactated Ringer’s solution. Feeding tubes should also be available for insertion into the stomach to drain the contents or air.
 A pulse oximeter should be available. In term infants needing resuscitation, the pulse oximeter provides valuable information (heart rate and oxygen saturation levels) regarding whether the interventions are succeeding.
A pulse oximeter should be available. In term infants needing resuscitation, the pulse oximeter provides valuable information (heart rate and oxygen saturation levels) regarding whether the interventions are succeeding.
 A medication box should be present with all medications that might be necessary for resuscitation of a neonate. Although the use of medications such as bicarbonate and calcium have fallen out of favor, there are unique situations in which these solutions may be needed as well as pressor drugs, such as epinephrine, Prostaglandin E1 for ductal dilation, and narcotic antagonists such as naloxone. Rarely are any other medications required in the delivery room.
A medication box should be present with all medications that might be necessary for resuscitation of a neonate. Although the use of medications such as bicarbonate and calcium have fallen out of favor, there are unique situations in which these solutions may be needed as well as pressor drugs, such as epinephrine, Prostaglandin E1 for ductal dilation, and narcotic antagonists such as naloxone. Rarely are any other medications required in the delivery room.
 Suction for the removal of meconium and the emptying of stomach contents must be present.
Suction for the removal of meconium and the emptying of stomach contents must be present.
 An umbilical cord clamp and scissors should be on hand.
An umbilical cord clamp and scissors should be on hand.
 Erythromycin eye ointment should be present for prevention of gonococcal ophthalmia.
Erythromycin eye ointment should be present for prevention of gonococcal ophthalmia.
 Vitamin K1 for the prevention of vitamin K–dependent hemorrhagic disease of the newborn should be on hand.
Vitamin K1 for the prevention of vitamin K–dependent hemorrhagic disease of the newborn should be on hand.
The thermal neutral environment is usually in the range of 36° to 37.5° C skin temperature. Both term and preterm infants suffer similarly when under environmental stress, but the large surface to body mass ratio of the premature infant exaggerates the adverse consequences ( Fig. 1-1).
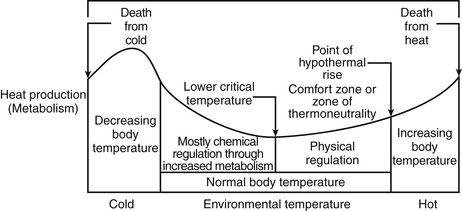
Figure 1-1 McCall EM, Alderdice F, Halliday HL, et al. Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database Syst Rev 2010 Mar 17;3:CD004210.
8. What should the first step be after the delivery of a term infant, once the baby is handed to the clinician?
Other infectious agents capable of causing an eye infection in the newborn infant include Staphylococcus, Group A and B Streptococcus, Pneumococcus, Pseudomonas aeruginosa, and herpes simplex virus. ∗
Studies from a number of investigators in recent years have contradicted the traditional concept that babies become well saturated within a few breaths after birth. In fact, the transition usually requires between 10 and 12 minutes, or longer occasionally, before a term infant’s saturation reaches approximately 93% to 95% ( Fig. 1-2).
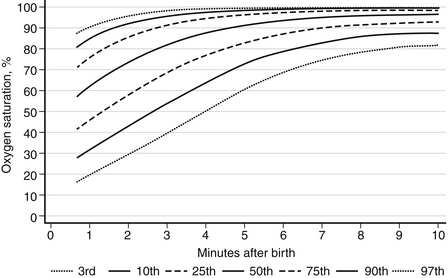
Figure 1-2 3rd, 10th, 25th, 50th, 75th, 90th, and 97th SpO2 percentiles for all infants with no medical intervention after birth.
For many years babies with congenital heart disease arrived in the delivery room with no prenatal diagnosis. Such infants commonly presented with severe cyanosis and respiratory distress, often beginning within minutes of birth. With the introduction of antenatal ultrasound screening during the early 1980s, the number of babies who were born undiagnosed dropped dramatically. It was evident, however, that some critical cardiac diagnoses could be overlooked on ultrasound examination and not manifest until some time later (even after hospital discharge of the infant), placing the baby at some jeopardy. Ductal-dependent lesions, in which the systemic circulation is oxygenated through blood flowing through a patent ductus arteriosus, may result in sudden cardiovascular collapse in affected infants as the ductus closes, with a risk of death. Lesions that can provoke this sudden deterioration include coarctation of the aorta, hypoplastic left heart syndrome, aortic stenosis, and transposition of the great vessels.
Oxygen saturation screening, in which oxygen saturation is less than 95% on day 2 of life, has been demonstrated to identify many of the infants who are not diagnosed during physical examination. Because of the apparent value of this screening, in 2011 the Secretary of Health and Human Services, Kathleen Sebelius, recommended the use of oxygen saturation screening in newborn infants before hospital discharge. ∗†
A number of infants will not consistently demonstrate saturation levels at 95% or above in the 2 days before discharge from the nursery for a variety of reasons, most of which are not reflective of congenital heart disease. Preliminary data collected by Pediatrix Medical Group suggest that approximately 0.5% of all infants will fail initial screening. According to some observations, infants born at higher altitudes (>4000 feet) appear to have a false-positive rate of nearly 50% during initial screening. All infants who screen positive should be followed up with the currently recommended cardiac echocardiogram. This requirement presents substantial difficulties for many nurseries. In addition, many of the community hospitals around the country that offer maternity services do not have ready access to a cardiologist who can perform this study. It may become necessary to modify the screening procedure in the near future to prevent a prohibitive increase in the cost of care. ∗
With the increased enthusiasm for breastfeeding of newborn infants, babies are often placed at the mother’s breast within minutes of delivery. Although mother’s milk is scanty at this time and it takes approximately 2 to 3 days for full milk flow to appear, the provision of the high fatty content of colostrum (the earliest milk that is secreted from the breast), together with the immunoprotective characteristics (e.g., white blood cells, antibodies) of colostrum, appears to be very advantageous for newborns and greatly reduces the incidence of hypoglycemia. ∗
Although breastfeeding is clearly best, it is not always possible. Infants with galactosemia should not nurse; instead, they must be fed a lactose-free formula. In the United States mothers with human immundeficiency virus (HIV) should also not nurse or provide expressed milk because they may pass on the virus to the infant. Mothers with active untreated tuberculosis or active herpes simplex lesions on the breast should also not breastfeed, but they may use expressed milk because these organisms are not transmitted through the milk. Mothers who require antimetabolites or chemotherapy should not breastfeed as long as they are receiving those medications. Radioactive materials acquired during the performance of a medical study are temporary contraindications to nursing. Whereas most drugs are secreted into breast milk, they rarely form an absolute contraindication to nursing. Drug effects, however, should be carefully checked using a reliable resource to ensure that the infant is not unnecessarily exposed to a potentially hazardous medication. ∗†‡
Manufacturers of formula have long established that infants grow quite satisfactorily on any of the commercially available infant formulas. Nevertheless, it is evident that breast milk and formula are different in terms of their appearance and their composition. The most striking difference is the immunoprotective aspect of breast milk, which contains white cells and antibodies that appear to be quite valuable in preventing neonatal infections of a variety of types, especially in the respiratory system and the gastrointestinal tract. ∗
Variations in the composition of breast milk among individual mothers can be quite dramatic. Some women will have relatively modest fat content in their milk, resulting in a caloric content as low as 9 to 10 calories per ounce. In contrast, other mothers produce rich, creamy breast milk, with a high fat content and a caloric density that may reach 30 calories per ounce. ∗
Similarly, protein in breast milk is more bioavailable than protein in formula, and the concentration of protein in formula is correspondingly higher than the amount of protein in breast milk (formula contains approximately 2 to 2.1 g protein/100 kcal versus 1.5 g protein/100 kcal of breast milk). Similar differences between formula and breast milk exist for other vitamins and minerals, as well, to overcome the reduced bioavailability in formula.
23. A 3-week-old baby who is nursing falls asleep after approximately 10 minutes at the breast. Has this baby nursed long enough?
26. “I enjoy nursing my baby, but she wakes up for feeding every 1½ to 2 hours. I am getting exhausted. What do I do?”
Many neonates, both from a nutritional and a comfort perspective, derive great pleasure from nursing. As a result, they often become avid feeders and want to nurse around the clock. This behavior may be especially true for infants whose mothers have breast milk with lower fat content because these babies need to nurse more often to feel satiated. For those mothers, however, the joy of nursing soon gives way to chronic fatigue caused by awakening throughout the night to nurse.
The umbilical cord usually takes approximately 10 to 14 days to separate and fall off. Infants whose cords remain on longer may, in rare cases, have an immune deficiency that interferes with and delays this process. Until it falls off, the umbilical cord should simply be kept clean. In the past parents were told to clean the cord with alcohol frequently, but some evidence suggests that this may actually delay cord separation and offers no real advantage. Therefore the cord should be gently cleaned with warm water once or twice a day. Diapers should be folded down below the cord level so that the rough cord edges do not irritate or scrape the periumbilical area. If the cord becomes contaminated with urine or stool, it should be washed carefully with warm water and then dried well. Parents should avoid the tendency to pull the cord off, even when it appears to be hanging by a thin thread because doing so may result in omphalitis. ∗
In the majority of cases, continued oozing from an umbilical cord is caused by an umbilical granuloma ( Fig. 1-3).
The granuloma represents a cord remnant but does not appear to be associated with any known disease states. It is pinkish-white and secretes a thin, watery mucous discharge. It is easily treated by application of silver nitrate to the granuloma. It is important to avoid the surrounding umbilical area when applying the silver nitrate.
Omphalitis is cellulitis of the umbilicus or periumbilical area. It is marked by a red, indurated area around the umbilicus; fever; irritability; and a generally ill-appearing neonate. It typically appears during the latter part of the first or second week of life, just before cord separation. In addition to generalized sepsis, the greatest risk to the infant is spread to the abdominal fascial plane or penetration into the connecting vascular system (causing portal vein thrombosis). Omphalitis can be life-threatening and is usually caused by gram-positive organisms, especially Staphylococcus aureus.∗
Circumcision refers to the removal of the foreskin of the penis. The most recent recommendations of the AAP state that “the preventive health benefits of elective circumcision of newborn males outweigh the risks of this procedure. Benefits include significant reductions in the risk of urinary tract infection in the first year of life and, subsequently, in the heterosexual risk of HIV and other sexually transmitted infections. Although health benefits are not great enough to recommend routine circumcision for all newborn males, the benefits of circumcision are sufficient to justify access to this procedure for families choosing it and to warrant third-party payment for circumcision of newborn males.” (Guidelines for Perinatal Care, 7th Edition, 2012, American Academy of Pediatrics, and the American College of Obstetrics and Gynecology, p. 286). Ritual circumcision is part of a number of religions, and cultural differences should be respected. ∗
If you practice pediatric medicine for any length of time, you have received a call from a nurse informing you that a baby has not voided for ____ hours (the number of hours varies). The problem with voiding in the neonatal period is that it is a complex phenomenon that depends on fluid volume at the time of birth and a variety of other factors, many of which are not easily measurable. Furthermore, it is not uncommon for an infant to void in the delivery room without anyone noticing. As a result, many newborn infants will not void during the first 24 hours of life. If a baby goes beyond 24 hours without voiding, however, it is reasonable to determine why the infant is failing to pass urine. As a first step, the clinician should attempt to palpate the bladder. If the bladder is obstructed (the posterior urethral valves in a male infant is the most common site), the bladder will be easily felt and sometimes observed as a bulge above the symphysis pubis. If there is a concern about a urinary tract anomaly or renal failure, laboratory studies (blood urea nitrogen, creatinine, and electrolyte concentrations) and an ultrasound of the urinary tract should be obtained. The management of neonates with suspected renal failure is complex and should always include consultation with a pediatric nephrologist and, when appropriate, a urologist.
36. Why do babies need to be tested immediately after birth for certain metabolic and genetic diseases?
There are three primary goals that otherwise healthy infants must meet to be discharged from the hospital after birth: (1) the ability to feed adequately; (2) the ability to maintain body temperature in a room air temperature environment; and (3) absence of any cardiorespiratory abnormality that may place an infant at risk. The infant must also have passed stool and voided. Although the preceding goals are relatively easy for the term infant to meet, a variety of common issues may delay discharge. These include hyperbilirubinemia, hypoglycemia, suspected septicemia, infant apnea, anemia, and signs of substance withdrawal. Because many of these topics are discussed in depth elsewhere in this book, they will not be presented in detail here. Although parents whose infants cannot be discharged at 48 hours are often greatly distressed, a clear and sympathetic explanation of the reasons this is necessary usually alleviates their concerns. Providing a comfortable place for the mother to visit during the delayed discharge should also be a high priority of care.
Although breast milk is the best nutritive substance for infants, studies have demonstrated a high incidence of deficient vitamin D levels in breastfed infants. Breast milk can be low in vitamin D as a result of a lack of maternal sun exposure (particularly in the winter and in northern latitudes), increased use of sunscreen, and dress habits that prevent skin exposure. The AAP recommends that any breastfeeding infant be given 400 IU of vitamin D daily beginning within a few days of life. In breastfed infants who are receiving supplemental formula, vitamin D supplementation should still be provided unless the infant is consuming 1 liter of formula per day (the amount needed to provide 400 IU). ∗
Pacifier use has previously been discouraged in breastfed infants because studies have demonstrated an association with less successful breastfeeding. However, pacifier use has also been shown to be associated with a reduction in the incidence of sudden infant death syndrome (SIDS). Thus it is now recommended that all formula-fed infants be given a pacifier at nap or at bedtime. For breastfeeding infants the use of a pacifier is also recommended at bedtime, but its use should not begin until breastfeeding has been well-established, which is typically 3 to 4 weeks after birth. ∗†
∗American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. Guidelines for perinatal care, 6th ed. Elk Grove Village, IL and Washington, DC: AAP and ACOG; 2007.
†Clark S, Miller D, Belfort M, et al. Neonatal and maternal outcomes associated with elective delivery. Am J Obstet Gynecol 2009;200:156.e1-156.e4.
∗Donahue SM, Kleinman KP, Gillman MW, et al.Trends in birth weight and gestational length among singleton term births in the United States. 1990–2005. Obstet Gynecol 2010 Feb;115(2 Pt 1):357–64.
∗American Academy of Pediatrics, The American College of Obstetrics and Gynecology. Care of the neonate in guidelines for perinatal care, 6th ed. 2007;205.
∗Finster M, Wood M. The Apgar score has survived the test of time. Anesthesiology. 2005 Apr;102(4):855–7.
∗Zuppa AA, D’Andrea V, Catenazzi P, et al. Ophthalmia neonatorum: what kind of prophylaxis? J Matern Fetal Neonatal Med 2011 Jun;24(6):769–73.
∗Bradshaw EA, Martin GR. Screening for critical congenital heart disease: advancing detection in the newborn. Curr Opin Pediatr 2012 Oct;24(5):603–8.
†Mahle WT, Martin GR, Beekman RH 3rd, et al. Section on Cardiology and Cardiac Surgery Executive Committee. Endorsement of Health and Human Services recommendation for pulse oximetry screening for critical congenital heart disease. Pediatrics 2012 Jan;129(1):190–2.
∗Bradshaw EA, Cuzzi S, Kiernan SC, et al. Feasibility of implementing pulse oximetry screening for congenital heart disease in a community hospital. J Perinatol 2012;32:710–5.
∗Eidelman AI, Schanler RJ. American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e834.
∗Eidelman AI, Schanler RJ. American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e832.
†Schaefer C, Peters PWJ, Miller RK. Drugs during pregnancy and lactation: treatment options and risk assessment, 2nd ed. London: Academic Press; 2007.
‡Weiner CP, Buhimschi C. Drugs for pregnant and lactating women. Philadelphia: Saunders; 2009.
∗Hurley WL, Theil PK. Perspectives on immunoglobulins in colostrum and milk. Nutrients 2011;3:442–74.
∗Jacobi SK, Odle J. Nutritional factors influencing intestinal health of the neonate. Adv Nutr 2012;3:687–96.
∗Takada H, Yoshikawa H, Imaizumi M, et al. Delayed separation of the umbilical cord in two siblings with Interleukin-1 receptor–associated kinase 4 deficiency: rapid screening by flow cytometer. J Pediatr 2006;148:546–8.
∗Saleem S. Application of 4% chlorhexidine solution for cord cleansing after birth reduces neonatal mortality and omphalitis. Evid Based Med 2012. [Epub ahead of print]
∗AAP Task Force on Circumcision. Pediatrics 2012;130;e756–e785.
∗Wagner CL, Greer CR. American Academy of Pediatrics Committee on Breastfeeding; American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children and adolescents. Pediatrics 2008;122:1142–1152.
∗O’Connor NR, Tanabe KO, Siadaty MS, et al. Pacifiers and breastfeeding: a systematic review. Arch Pediatr Adolesc Med 2009;163:378–382.
†Hauck FR, Omojokun OO, Siadaty MS. Do pacifiers reduce the risk of sudden infant death syndrome? A meta-analysis. Pediatrics 2005;116:e716-e723.