Chapter 50B Cancer of the bile ducts
Extrahepatic biliary tumors
Incidence and Etiology
Worldwide, cholangiocarcinoma accounts for approximately 3% of all gastrointestinal cancers. In the United States, where approximately 5000 new cases (gallbladder cancers excluded) are diagnosed each year, the annual incidence of bile duct cancer is estimated at 1 to 2 per 100,000 (Carriaga & Henson, 1995; Greenlee et al, 2001; Khan et al, 2005). Over the past 3 decades, a trend has been seen toward older patient age (median range, 65 to 70 years) at the time of diagnosis and a relative increase in the ratio of intrahepatic to extrahepatic cholangiocarcinoma (see Chapter 50A; Carriaga & Henson, 1995; Endo et al, 2008a; Patel, 2001; Weber et al, 2007).
The molecular changes associated with the pathogenesis of cholangiocarcinoma are poorly characterized (see Chapter 8B). Multiple KRAS oncogene mutations at codon 12 have been identified in almost all resected specimens (Levi et al, 1991). These mutations most likely occur at some point along a stepwise progression to malignancy but probably are not the inciting genetic lesion. There are wide epidemiologic variations in the incidence of KRAS mutations (Lee et al, 1995; Levi et al, 1991; Nakamura et al, 1981). Many studies have reported differences in various genetic abnormalities according to location within the biliary tree, suggesting anatomic differences in pathogenesis. An in-depth review of the molecular biology of biliary cancer is beyond the scope of this chapter; the interested reader is referred to selected review articles (Rashid, 2002) and to Chapter 8B.
The majority of patients with cholangiocarcinoma have no obvious risk factors, although several conditions are associated with an increased incidence of cholangiocarcinoma. In the United States, the most common risk factor for cholangiocarcinoma is primary sclerosing cholangitis (PSC), an autoimmune disease characterized by periductal inflammation resulting in multifocal strictures of the intrahepatic and extrahepatic bile ducts (see Chapter 41; Broome et al, 1996; Katoh et al, 1988; Pitt et al, 1995a, 1995b). Approximately three quarters of patients with PSC have underlying ulcerative colitis (Broome et al, 1996). The natural history of PSC is quite variable, and the true incidence of cholangiocarcinoma is difficult to calculate but appears to depend on disease duration. In a Swedish series of 305 patients followed for more than 5 years, 8% of patients eventually developed cancer (Broome et al, 1996), and occult cholangiocarcinoma has been reported in 40% of autopsy specimens and 36% of liver explants from patients undergoing orthotopic liver transplantation for PSC (Broome et al, 1996; Katoh et al, 1988; Pitt et al, 1995a). Unfortunately, cholangiocarcinoma arising in the setting of PSC frequently is not amenable to operative resection because of advanced underlying hepatic parenchymal disease or multifocal malignancy. Medical or surgical treatment of coexisting ulcerative colitis in patients with PSC does not alter the subsequent risk of developing cholangiocarcinoma (Broome et al, 1996; Katoh et al, 1988; Pitt et al, 1995a).
Choledochal cysts are associated with an increased risk for cholangiocarcinoma (see Chapter 46; Hewitt et al, 1995; Vogt, 1954). The incidence of bile duct cancer in patients with congenital biliary cystic disease is substantial (15% to 20%), especially in patients who are not treated until after age 20 years and in patients previously treated by cyst drainage (Lipsett et al, 1994; Vogt, 1954). The hypothetical risk for malignant transformation of choledochal cysts may be related to an anomalous pancreatobiliary junction, which is commonly found in these patients and predisposes them to reflux of pancreatic juice into the biliary tree and chronic inflammation of the bile ducts (Lipsett et al, 1994; Jeng et al, 1994; Tanaka et al, 1998a; Vogt, 1954). By similar mechanisms, transduodenal sphincteroplasty and endoscopic sphincterotomy may be associated with an increased risk for cholangiocarcinoma (Tanaka et al, 1998b). In a series of 119 patients subjected to sphincteroplasty for benign disease (sphincter of Oddi dysfunction), Hakamada and associates (1997) found a 7.4% incidence of cholangiocarcinoma over 18 years.
Recurrent pyogenic cholangiohepatitis and hepatolithiasis resulting from chronic portal bacteremia and portal phlebitis are prevalent in Japan and parts of Southeast Asia (see Chapters 39 and 44). Although most cholangiocarcinomas in these patients arise within the intrahepatic ducts, cases of extrahepatic cholangiocarcinoma have been reported (Chen et al, 2004; Chu et al, 1997; Kubo et al, 1995; Meade et al, 1994; Winslet et al, 1990). Biliary parasites—specifically, Clonorchis sinensis and Opisthorchis viverrini—are endemic in parts of Asia and are associated with an increased risk of cholangiocarcinoma (Pitt et al, 1995a, 1995b). In Thailand, where approximately 7 million people are chronically infected with Opisthorchis, the annual incidence of cholangiocarcinoma is 87 per 100,000 (see Chapter 45; Watanapa, 1996). In addition, several radionuclides and chemical carcinogens may be associated with an increased risk of cholangiocarcinoma, including thorium, radon, nitrosamines, dioxin, and asbestos.
Tumor Location and Histopathology
Adenocarcinoma is the most common neoplasm arising from the biliary tract and accounts for more than three fourths of all bile duct tumors (Are et al, 2006; Jarnagin et al, 2001). Benign neoplasms and strictures occasionally will mimic many of the clinical, radiographic, and operative findings associated with malignant biliary strictures. Other reported tumors of the extrahepatic bile ducts include adenoma, leiomyoma, paraganglioma, lipoma, granular cell tumor, and carcinoid (Felekouras et al, 2009; Holzinger et al, 1999). Benign strictures resulting from autoimmune pancreatitis, granulomatous disease, and PSC can masquerade as biliary neoplasms and should be treated as such (see Chapter 42A; Corvera et al, 2005; Hadjis & Blumgart, 1985). Malignant strictures of the extrahepatic biliary tree may represent secondary involvement from cancers arising from the gallbladder, pancreas, and periportal lymph nodes (see Chapter 49).
Cholangiocarcinoma can arise anywhere within the biliary tree, but tumors involving the biliary confluence are the most common. Retrospective reviews from high-volume centers reveal that between 40% and 60% of cholangiocarcinoma cases involve the perihilar bile ducts (Burke, 1998; Nagorney et al, 1993; Nakeeb et al, 1996a, 1996b; Tompkins et al, 1981). Tumors of the lower bile duct are classified according to their anatomic location, although there may be considerable overlap. Distal bile duct tumors typically arise within the pancreatic portion of the common bile duct (Tompkins et al, 1981) and represent approximately 20% to 30% of all cholangiocarcinomas and 5% to 10% of all periampullary tumors (Fong et al, 1996; Nakeeb et al, 1996a, 1996b; Wade et al, 1997; Yeo et al, 1997). Tumors of the mid–bile duct are rare and arise below the confluence of the hepatic ducts, usually between the upper border of the pancreas at the level of the cystic duct. The majority of such malignant strictures are caused by gallbladder cancer or cystic duct–based tumors.
Cholangiocarcinomas can present with extensive ductal involvement alone or with early metastatic spread to the liver, regional lymph nodes, or peritoneum (Jarnagin et al, 2005; Tsuzuki et al, 1983). Most bile duct cancers demonstrate characteristic invasive spread along ductal subepithelial histologic planes. Perineural and lymphovascular involvement is common, as is direct invasion into the liver or perihepatic structures (Weinbren & Mutum, 1983).
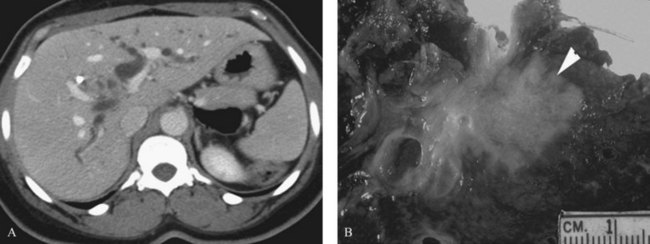
Three distinct macroscopic subtypes of cholangiocarcinoma have been described: 1) sclerosing, 2) nodular, and 3) papillary (Weinbren & Mutum, 1983). Sclerosing tumors account for most cases and are more common at the hilus than in the distal bile duct. They are firm and cause an annular thickening of the bile duct, often with diffuse infiltration and fibrosis of the periductal tissues (Fig. 50B.1). Nodular tumors are characterized by a firm, irregular nodule of tumor that projects into the lumen of the duct. Features of both types are often seen, hence the frequently used descriptor nodular-sclerosing. The papillary tumors account for approximately 10% of all cholangiocarcinomas, and although occasionally seen at the hilus, these are more common in the distal bile duct (Weinbren & Mutum, 1983). These tumors are soft and friable and may be associated with little transmural invasion; a polypoid mass that expands the duct, rather than contracting it (Fig. 50B.2), is a characteristic feature. Although papillary tumors may grow to a significant size and appear surgically unapproachable on radiographic studies, they often arise from a well-defined stalk and can be minimally invasive. The bulk of the tumor frequently is mobile within the bile duct. Recognition of this variant is important, because they appear to be more often resectable and have a more favorable prognosis than the sclerosing type (Jarnagin et al, 2005; Pitt et al, 1995a).
Longitudinal spread along the duct wall and periductal tissues is an important pathologic feature of cholangiocarcinomas (Endo, 2008b; Sakamoto et al, 1998; Weinbren & Mutum, 1983). There may be substantial extension of tumor beneath an intact epithelium, and it can extend as much as 2 cm proximally and 1 cm distally (Sakamoto et al, 1998; Shimada et al, 1988). The full tumor extent may be underestimated by radiographic studies and may not be appreciated on palpation. This predilection for submucosal extension underscores the importance of frozen-section analysis of the duct margins during resection, although its utility has been called into question (Endo et al, 2008b). Although most of these tumors are adenocarcinomas, in rare instances other malignant cell types may arise primarily in the biliary tree and cause biliary obstruction, such as carcinoid tumors (Jutte et al, 1987; Rugge et al, 1992; Sankary et al, 1995).
Clinical Presentation
The early symptoms of hilar and distal cholangiocarcinoma are nonspecific. Abdominal pain, anorexia, weight loss, and pruritus are the most common symptoms, but these are seen only in about one third of patients. Fever is rarely seen at initial presentation but is common once biliary manipulation is initiated (Farley et al, 1995; Katoh et al, 1988; Meade et al, 1994; Nakeeb et al, 1996b; Pitt et al, 1995a; Vatanasapt et al, 1990b). Most patients have few symptoms and come to attention because of jaundice or abnormal liver function tests. Although most patients eventually become jaundiced, this finding is not present initially in cases of incomplete biliary obstruction (i.e., right or left hepatic duct) or segmental ductal obstruction. Segmental obstruction may go unrecognized for a long time, resulting in ipsilateral lobar atrophy without overt jaundice (see Chapter 5). These patients often are further evaluated and diagnosed because of an elevated serum alkaline phosphatase.
The clinical presentation of distal bile duct cancer generally is indistinguishable from that of other periampullary malignancies. Progressive jaundice is seen in 75% to 90% of patients. Abdominal pain, weight loss, fever, or pruritus occur in one third of patients or fewer (Fong et al, 1996; Nakeeb et al, 1996a, 1996b).
In jaundiced patients, the total bilirubin level may suggest an etiology. In patients with obstruction from cholangiocarcinoma, the serum bilirubin level is often greater than 10 mg/dL and averages 18 mg/dL, whereas patients with obstruction from choledocholithiasis have bilirubin levels 2 to 4 mg/dL and rarely greater than 15 mg/dL (Way, 1994); however, there is likely to be considerable overlap. Furthermore, the degree of jaundice may suggest the level of bile duct obstruction. Hilar obstruction is typically associated with higher levels of serum bilirubin compared with distal tumors. In patients with cholangiocarcinoma and no previous biliary intervention, cholangitis is uncommon at initial presentation despite a 30% incidence of bactibilia (see Chapter 43; Hochwald et al, 1999; Meade et al, 1994). The incidence of bactibilia is nearly 100% after biliary intubation, and cholangitis is also more common (Hochwald et al, 1999). Gallstones or common bile duct stones may coexist with bile duct cancer. In the absence of certain predisposing conditions (PSC, choledochal cyst, hepatolithiasis), however, it is uncommon for choledocholithiasis to cause obstruction at the biliary confluence. It is imperative to investigate fully and delineate the level and nature of any obstructing lesion causing jaundice to avoid missing the diagnosis of carcinoma.
Bactibilia is relatively common in patients with hilar cholangiocarcinoma; however, in the absence of prior biliary manipulation, frank cholangitis is uncommon at initial presentation (McPherson et al, 1984).
Diagnostic Studies
The diagnosis of hilar and distal cholangiocarcinoma usually follows targeted studies for the evaluation of obstructive jaundice or elevated liver enzymes. Most patients are referred after having had some studies done elsewhere, usually computed tomography (CT) and often some form of direct cholangiography, such as percutaneous transhepatic cholangiography (PTC) or endoscopic retrograde cholangiopancreatography (ERCP). In our view, histologic confirmation of malignancy is not mandatory before exploration. In the absence of previous biliary tract surgery, the finding of a focal stenotic lesion combined with the appropriate clinical presentation is sufficient for a presumptive diagnosis of hilar cholangiocarcinoma, which is correct in most instances (Wetter et al, 1991).
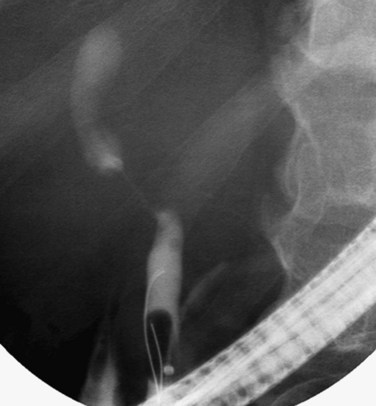
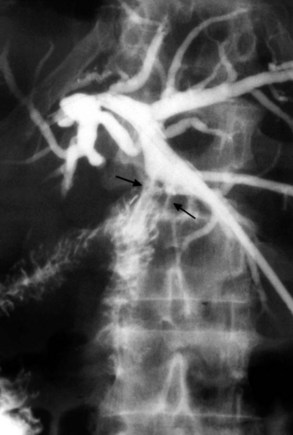
Although most patients with hilar strictures and jaundice have cholangiocarcinoma, alternative diagnoses are possible in 10% to 15% of patients (Wetter et al, 1991). The most common of these are gallbladder carcinoma, Mirizzi syndrome, and benign focal strictures, such as lymphoplasmacytic sclerosing pancreatitis/cholangitis, granulomatous disease, and PSC (see Chapter 42A, Chapter 42B, Chapter 48, Chapter 49 ). Distinguishing gallbladder carcinoma from hilar cholangiocarcinoma can be difficult. A thickened, irregular gallbladder wall with infiltration into segments IV and V of the liver, selective involvement of the right portal pedicle, and obstruction of the mid–bile duct with occlusion of the cystic duct on endoscopic cholangiography all suggest gallbladder carcinoma (Fig. 50B.3).
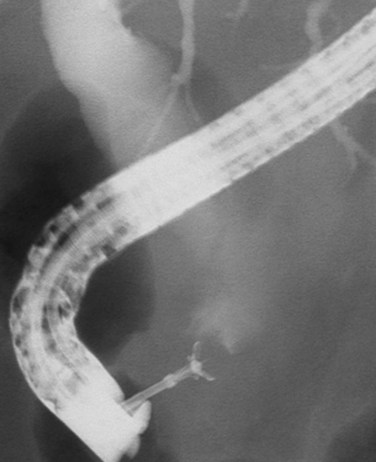
Mirizzi syndrome is a benign condition resulting from a large gallstone impacted in the neck of the gallbladder (see Chapters 29 and 42A). The ensuing pericholecystic and periductal inflammation and fibrosis can obstruct the proximal bile duct, which is often difficult to distinguish from a malignant obstruction (Baer et al, 1990; Callery et al, 1997; Cabooter et al, 1990). Other benign focal strictures (malignant masquerade) can occur at the hepatic duct confluence but are uncommon (Fig. 50B.4; Hadjis et al, 1985; Saldinger & Blumgart, 2000; Verbeek et al, 1992; Wetter et al, 1991). The finding of a smooth, tapered stricture on cholangiography suggests a benign stricture. Diagnostic assessments based on the cholangiographic appearance of the stricture are unreliable, and hilar cholangiocarcinoma must remain the leading diagnosis until definitively disproved with operative exploration. The alternative conditions that one may encounter are best assessed and treated at operation. Relying on the results of percutaneous needle biopsy or biliary brush cytology is dangerous, because they often are misleading, and the surgeon may miss the opportunity to resect an early cancer (Enjoji et al, 1998; Rabinovitz et al, 1990). In the absence of clear contraindications, exploration is indicated in all patients with suspicious hilar lesions with concordance of clinical and radiographic findings.
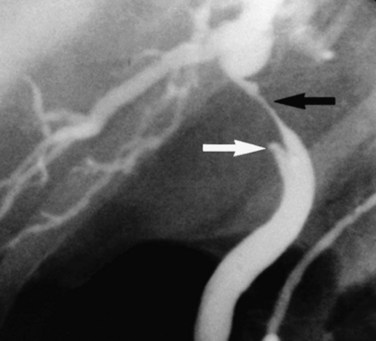
FIGURE 50B.4 Endoscopic retrograde cholangiopancreatography from a patient with a benign stricture of the proximal bile duct. The smooth, tapered appearance (black arrow) is in contrast to the irregular stricture typical of a sclerosing tumor. Nonfilling of the cystic duct (white arrow) is an important finding, and in the appropriate setting, it should raise the suspicion of gallbladder carcinoma (see Fig. 50B.3). In this patient, the chronic inflammatory process had involved the hepatic duct and cystic ducts. Most cases of benign strictures of the proximal bile duct spare the cystic duct.
Many tumors express carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA 19-9). Serum levels of these markers, although elevated in some patients, have had little diagnostic value (Pitt et al, 1995a). It has been suggested that CEA levels in hepatic bile may help distinguish between benign and malignant strictures in patients with premalignant conditions (Nakeeb et al, 1996a).
Direct cholangiography (see Chapter 18) shows the location of the tumor and the biliary extent of disease, both of which are crucial in surgical planning. When performed skillfully, ERCP provides useful duct detail and can effectively drain functional liver segments prior to operative planning. Although invasive, PTC outlines the extent of intrahepatic bile duct involvement reliably and has been the preferred study in the past (Pitt et al, 1995a, 1995b). High-quality cholangiograms are often thought to be essential for accurately diagnosing the extent of cancer (Kondo et al, 2004; Nimura, 1997). In many centers, particularly in Japan, surgeons extend the diagnostic process by performing detailed cholangiography with one or more percutaneous catheters placed in the intrahepatic ducts, often combined with percutaneous cholangioscopy along a mature transhepatic drain tract (Ohkubo et al, 2004; Ozden, 2002). PTC with biliary drainage should be considered not only an effective method of relieving jaundice but also an important diagnostic modality.
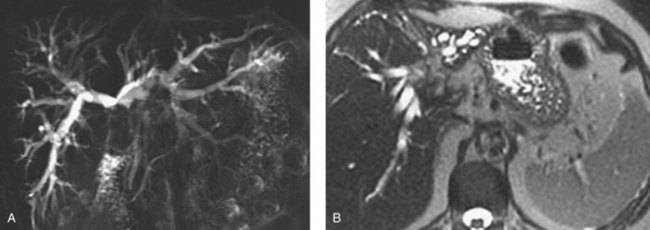
MRCP is a powerful investigative tool that has almost replaced endoscopic and percutaneous cholangiography as the initial preoperative assessment of hilar cholangiocarcinoma (see Chapter 17). Several studies have shown its utility in evaluating patients with biliary obstruction (Guthrie et al, 1996; Lee et al, 1997; Schwartz et al, 1998). MRCP may not only identify the tumor and the level of biliary obstruction, but it also may reveal obstructed and isolated ducts not appreciated at endoscopic or percutaneous study (Fig. 50B.5). MRCP also provides information regarding the patency of hilar vascular structures, the presence of nodal or distant metastases, and the presence of lobar atrophy (Fig. 50B.6).
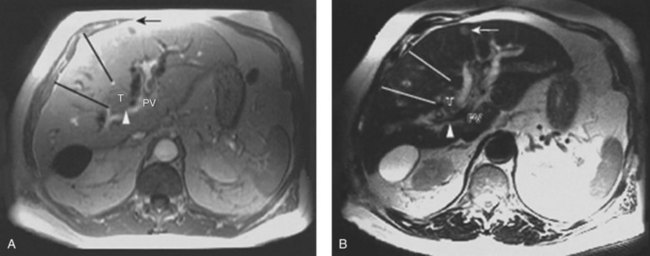
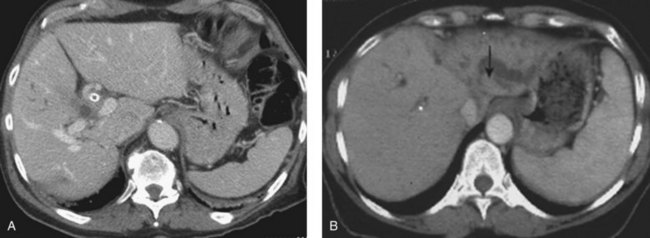
CT is an important study for evaluating patients with biliary obstruction. A high-quality CT scan can provide valuable information regarding the level of obstruction, vascular involvement, and liver atrophy (Fig. 50B.7; see Chapter 16). Advances in CT technology permit the acquisition of three distinct circulatory phases—the arterial, pancreatic, and portal venous phases—in the hilar and pancreatobiliary region with 1-mm collimation. These isotropic volume data allow generation of high-quality three-dimensional images—such as CT arteriography, CT cholangiopancreatography, and CT portography—in a single scanning session (Itoh et al, 2005).
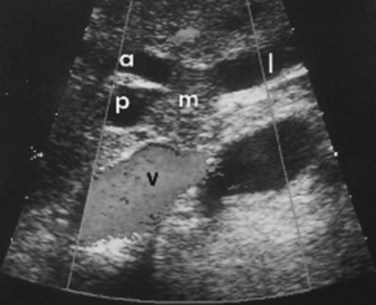
Although it is operator dependent, ultrasound (US) is a useful noninvasive diagnostic study (see Chapter 13). When utilized by experienced centers, it often delineates tumor extent accurately. US can not only show the level of biliary ductal obstruction, but it can also provide information regarding tumor extension within the bile duct and in the periductal tissues (Gibson et al, 1986; Hann et al, 1997; Okuda et al, 1988). Duplex US is firmly established as a highly accurate predictor of vascular involvement and resectability (Fig. 50B.8). In a series of 19 consecutive patients with malignant hilar obstruction, US with color spectral Doppler technique was equivalent to angiography and CT portography in diagnosing lobar atrophy, level of biliary obstruction, hepatic parenchymal involvement, and venous invasion (Hann et al, 1997). Duplex US is particularly useful for assessing portal venous invasion. In a series of 63 consecutive patients from Memorial Sloan-Kettering Cancer Center (MSKCC), duplex US predicted portal vein involvement in 93% of cases, with a specificity of 99% and a positive predictive value of 97%. In the same series, angiography with CT angioportography had a 90% sensitivity, 99% specificity, and 95% positive predictive value (Bach et al, 1996).
The diagnosis of malignancy in patients with bile duct strictures can be challenging and depends on accurate interpretation of ERCP and/or PTC as well as cross-sectional imaging (MRCP and CT) findings. ERCP in particular is a useful tool for assessing biliary tract strictures, as it permits visualization of the biliary tree with the opportunity for therapeutic intervention (biliary drainage) and collection of specimens for cytopathologic and histopathologic evaluation (Fig. 50B.9). Although highly specific, biliary brush cytology is limited by low to moderate sensitivity (15% to 68%; Fritcher et al, 2009). As a result, adjunctive diagnostic techniques including mutation analysis, DNA ploidy analysis, and fluorescence in situ hybridization (FISH) have been studied clinically and experimentally to improve tumor detection sensitivity (Kipp et al, 2010). Two types of chromosomal abnormalities are frequently identified with a clinical FISH probe set, namely polysomy and trisomy 7. Polysomy has been defined as a gain of two or more of the four probes in five cells. A large clinical study recently demonstrated that FISH was more sensitive than cytology for detecting biliary tract cancer and was able to detect 49 (22%) of 227 cancers that routine cytology interpreted as nonmalignant, without compromising test specificity (Fritcher et al, 2009).
Distal bile duct tumors frequently are mistaken for adenocarcinoma of the pancreatic head, the most common periampullary malignancy. In a series of 119 periampullary tumors, the site of origin was diagnosed incorrectly in 28% of patients preoperatively and in 20% of patients intraoperatively (Jones et al, 1985). Nevertheless, ERCP can provide valuable information regarding the level of obstruction and may show clearly that the obstruction is arising from the bile duct and does not involve the pancreatic duct. ERCP also may be useful in cases in which choledocholithiasis is suspected and may be therapeutic in these patients. PTC is generally less useful for tumors of the distal bile duct. A good quality cross-sectional imaging study also is required, usually CT, to assess for vascular involvement and metastatic disease. CT commonly does not reveal a mass, however, because these tumors are frequently small at the time of presentation. MRCP increasingly is being used to evaluate periampullary tumors. As is true for hilar lesions, it can provide images of the distal bile duct previously obtainable only with direct cholangiography and without the need for invasive procedures (Georgopoulos et al, 1999). A dilated extrahepatic bile duct terminating abruptly at its distal aspect without a concomitantly dilated pancreatic duct suggests a distal bile duct carcinoma.
In patients with a stricture of the distal bile duct and a clinical presentation consistent with cholangiocarcinoma, histologic confirmation of malignancy is generally unnecessary, unless nonoperative therapy is planned. Benign strictures occur in the lower bile duct, but these are difficult to differentiate definitively from malignant strictures without resection. Percutaneous needle biopsy is difficult, often impossible, because of the small size of these tumors. In addition, endoscopic brushings of the bile duct have an unacceptably low sensitivity, making a negative result virtually useless (Ryan, 1991). Reliance on the results of percutaneous endoscopic US-guided fine needle aspiration or endoscopic brush biopsy serves only to delay operative therapy.
Preoperative Evaluation and Management
When a biliary tract malignancy is suspected on clinical and radiographic grounds, patient evaluation should turn toward an assessment of tumor resectability and of hepatic and overall physiologic reserve. The presence of significant comorbid conditions, chronic liver disease, or portal hypertension generally precludes resection. In patients not fit for operation, biliary drainage is an appropriate intervention to consider, and the diagnosis should be confirmed histologically if palliative therapies focused on local and systemic disease control are anticipated. Patients with potentially resectable tumors occasionally present with biliary tract sepsis, frequently after instrumentation of the biliary tree. These patients require resuscitation and treatment of the infection before operation can be considered. The preoperative evaluation must address the four crucial determinants of resectability: 1) extent of tumor within the biliary tree, 2) vascular involvement, 3) hepatic lobar atrophy, and 4) metastatic disease (Burke, 1998; Jarnagin et al, 2005).
Lobar atrophy is an often overlooked or underappreciated finding in patients with hilar cholangiocarcinoma; however, its importance in determining resectability cannot be overemphasized, because it often influences therapy (Hadjis & Blumgart, 1987; see Chapter 5). Long-standing biliary obstruction may cause moderate atrophy, whereas concomitant portal venous compromise induces rapid and severe atrophy of the involved segments. On cross-sectional imaging, atrophy is characterized by a small, often hypoperfused lobe with crowding of the dilated intrahepatic ducts (Figs. 50B.10 and 50B.5B). The crucial determinants of resectability, including lobar atrophy, can be assessed with noninvasive studies that include cross-sectional imaging. Tumor involvement of the portal vein is usually present if compression, narrowing, encasement, or occlusion is seen on imaging studies.
Preoperative Biliary Drainage
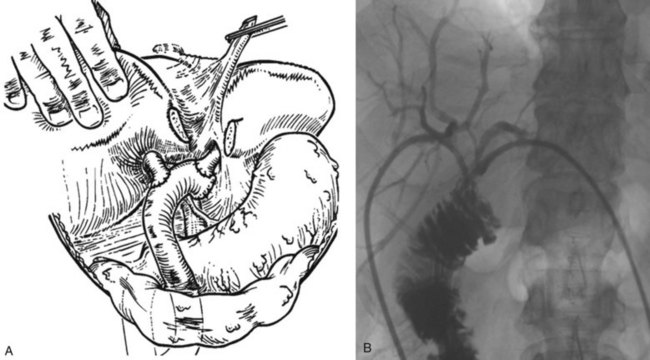
Typically, patients with hilar cholangiocarcinoma will require major liver resection, so their preoperative management must be optimized carefully. Obstructive jaundice associated with perihilar cholangiocarcinoma differs from that associated with middle or distal bile duct cancer. In distal bile duct cancer, a single catheter is enough for biliary drainage, whereas in perihilar cholangiocarcinoma, multiple biliary drainage catheters of the future liver remnant may be necessary. Experienced centers have demonstrated excellent results with endoscopic biliary drainage, but controversy exists as to whether this technique should replace percutaneous transhepatic biliary drainage (Gholson & Burton, 1991; Polydorou et al, 1992; Speer et al, 1987). Endoscopic retrograde biliary drainage offers several advantages, including low procedure-related morbidity and mortality, shorter hospital stay, and improved patient comfort. The limitations of endoscopic retrograde biliary drainage include a high incidence of cholangitis, especially when multiple obstructed ducts are instrumented but not subsequently drained (Andersen et al, 1989; Chang et al, 1998; Liu et al, 1998; Rerknimitr et al, 2004), and the difficulty in follow-up assessment of the extent of segmental duct involvement once an endobiliary stent is placed. Furthermore, control of which exact segmental ducts are cannulated is imperfect when performed endoscopically. For both endoscopic and percutaneous biliary drainage, a few guiding principles should be followed. The intrahepatic bile duct of the predicted future liver remnant (FLR) is intubated or punctured (Kawasaki et al, 2003; Seyama et al, 2003) and subsequently drained. If the FLR cannot be predicted with certainty in the preoperative setting, the left hepatic duct should be manipulated and drained (Fig. 50B.11). When the intrahepatic bile ducts are isolated into segmental units, PTC and multiple direct segmental transhepatic drainages may be necessary (Nagino et al, 1992; Nimura et al, 1995). If segmental cholangitis develops in patients with endoscopic or transhepatic biliary drainage catheters, urgent drainage of affected ducts should be attempted (Iyomasa et al, 1994; Sakamoto et al, 1995).
Clinical studies of biliary decompression have shown that external drainage has limited benefit, and that by preserving intestinal bile flow, the internal drainage is associated with more advantages (Clements et al, 1993). Superiority of internal drainage was shown in experimental studies, which showed that rat liver regeneration after partial hepatectomy is suppressed under external drainage but not under internal drainage (Saiki et al, 1999; Suzuki et al, 1994). Ogata and colleagues (2003) investigated bacterial translocation in bile duct–ligated rats, finding that bile replacement is essential to maintain intestinal barrier function. Impaired intestinal barrier function does not recover by percutaneous biliary drainage (PBD) without bile replacement. Bile replacement can restore the intestinal barrier function primarily as a result of repair of physical damage to the intestinal mucosa. Bile replacement during external biliary drainage should be recommended for planned hepatectomy for hilar cholangiocarcinoma because of the substantial infectious morbidity associated with these resections.
Many retrospective reports (Denning et al, 1981; Gundy et al, 1994; Nakayama et al, 1978; Norlander et al, 1982) support preoperative biliary drainage, whereas several older, prospective randomized studies (Hatfield et al, 1982; McPherson et al, 1984; Pitt et al, 1985) concluded that drainage did not reduce overall morbidity and mortality following management of proximal cholangiocarcinoma. The pertinence of the these cited randomized studies is questionable, as few major hepatectomies were included in these trials, and preoperative biliary drainage procedures were associated with unexpectedly high morbidity and mortality rates. In addition to accurate assessment of bile duct involvement, preoperative biliary drainage improves cholestatic liver disease and affords safer performance of hepatectomy for hilar cholangiocarcinoma. Lastly, the volume of the future liver remnant should be assessed prior to drainage, because with an atrophic hemiliver, very little functional liver may be removed with the resection, and performance of the operation without drainage should be considered (Kennedy et al, 2009).
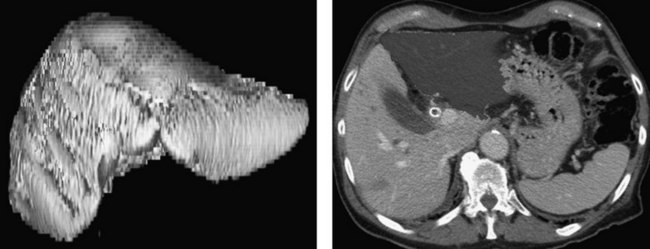
Three-Dimensional Computed Tomography
Advances in helical CT technology, such as multiple simultaneous detectors and subsecond rotation, have shown unparalleled capabilities for fast data acquisition and narrow collimation (see Chapter 16). Multidetector CT permits the acquisition of three distinct circulatory phases—arterial, portal, and late venous—in the pancreatobiliary and intrahepatic regions with 1-mm collimation. These isotropic volume data allow generation of high-quality three-dimensional images with CT arteriography, CT cholangiopancreatography, and CT portography in a single scanning session (Itoh et al, 2005).
CT is now a mainstay in the preoperative diagnostic evaluation for patients with perihilar cholangiocarcinoma, and it provides information on resectability and planning of the operation. Three-dimensional understanding of the main hepatic artery distribution may facilitate skeletonization of the hepatoduodenal ligament, and understanding of the intrahepatic artery branching is helpful during resection of the segmental or subsegmental bile ducts as the final step of resection. Hepatobiliary surgeons must appreciate two variations of the hepatic artery distribution: One is the left hepatic artery running right to the umbilical portion of the left portal vein, the other is a posterior branch of the right hepatic artery running cranially to the right portal trunk. Careful attention should be paid to the former variant in extended right hepatectomy with caudate lobectomy, and the same applies to the latter variant in extended left hepatectomy with caudate lobectomy (see Chapter 1B).
Unilateral involvement of the hepatic artery is compatible with resection (Williamson et al, 1980). Bilateral involvement of the hepatic artery usually is associated with nonresectability, when the tumor is located mainly on the right. Hepatic arterial reconstruction to accomplish a complete resection should be reserved for highly selected patients with potentially curable disease. Similarly, although not an absolute contraindication for resection of hilar cholangiocarcinoma, main portal vein invasion will preclude a complete resection with long-term benefit for the majority of patients (Blumgart et al, 1984; Hoevels & Ihse, 1979; Launois et al, 1979; Williamson et al, 1980). Despite the poor prognosis associated with main portal vein invasion in general, several groups have reported reasonable long-term outcomes with portal vein resection for advanced biliary cancer (Ebata et al, 2003; Miyazaki et al, 1998a; Nimura et al, 1991a; Sakaguchi & Nakamura, 1986).
Three-dimensional CT also offers the capacity to generate volumetric models of the total liver for planned hepatic resection and FLR (Fig. 50B.12). Because patients subjected to resection of more than 75% of functional liver parenchyma have substantially higher risk of postoperative liver failure regardless of existing cholestatic liver disease, routine preoperative volumetry may help to identify and select candidates for biliary drainage and portal vein embolization (PVE) who may be at considerable risk for postoperative morbidity and mortality.
Portal Vein Embolization
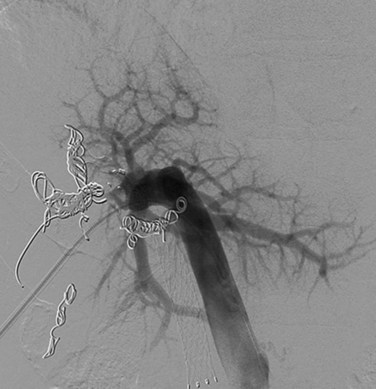
Devised by Makuuchi and colleagues (1990) and Kinoshita and colleagues (1986), PVE has become important in the presurgical management of patients who are to undergo extensive liver resection (see Chapter 93A, Chapter 93B ). The purpose of PVE is to increase the functional liver mass by inducing compensatory hypertrophy in the FLR. The ultimate goal of PVE is to minimize postoperative liver dysfunction, which contributes to mortality. PVE may be approached in two ways: the percutaneous approach, or percutaneous transhepatic portal vein embolization (PTPE) (Baere et al, 1993; Kinoshita et al, 1986), and the transileocolic approach, or transileocolic PVE (Makuuchi et al, 1990). PTPE can be accomplished with coil and/or microparticle embolization (Fig. 50B.13) and has established itself as the superior technique for several reasons, two of which are the avoidance of a laparotomy and avoidance of general anesthesia.
PTPE can produce a sizable compensatory hypertrophy of the nonembolized segments of the liver (Baere et al, 1993; Kawasaki et al, 1994; Nagino et al, 1995; Nagino, 2006). In right PVE, the volume of the left lobe increases by 130 cm3 on average within 2 weeks after embolization, and the estimated resection volume decreases by an average of approximately 10% (Nagino et al, 1995). Many case series have reported the clinical value of PVE (Abdalla et al, 2002; Elias et al, 2002; Farges et al, 2003; Hemming et al, 2003; Kawasaki et al, 2003; Nagino, 2006). A single prospective trial in patients undergoing right hemihepatectomy demonstrated a benefit in patients with chronic liver disease, but no benefit was reported in patients with normal livers (Farges et al, 2003), thus indications for PVE remain somewhat arbitrary.
Preoperative Staging
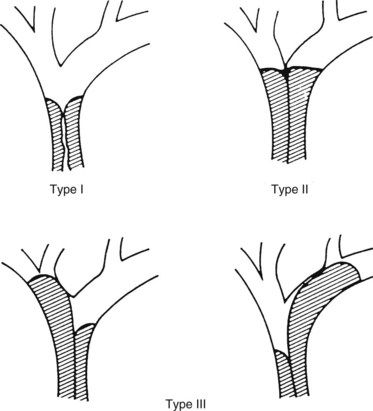
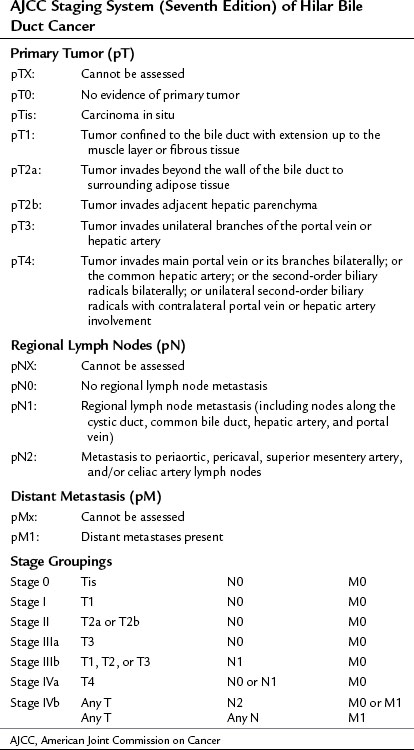
Historically, no clinical staging system was available to stratify patients preoperatively into subgroups based on potential for resection. The modified Bismuth-Corlette classification stratifies patients based on the extent of biliary duct involvement by tumor alone (Fig. 50B.14; Bismuth et al, 1992). Although useful to some extent, it does not predict resectability or survival. The American Joint Commission for Cancer (AJCC) tumor-node-metastais (TNM) staging system (Table 50B.1) is based largely on pathologic criteria and has little relevance to preoperative staging, because it can only be determined after resection. The ideal staging system should accurately predict resectability, the need for hepatic resection, and survival. Such a system would assist the surgeon in formulating a treatment plan, and it would help the patient understand the treatment options and likely outcome. Jarnagin and colleagues (2001) proposed such a system, one that improves characterization of tumor extent by taking into account all of the available preoperative data related to local tumor extent including 1) extent of tumor within the biliary tree, 2) vascular involvement, and 3) lobar atrophy. Using such an approach, it is possible to stage tumors preoperatively in a way that correlates with resectability and outcome. This preoperative T-staging system is based on the extent of local disease regardless of N or M status (Table 50B.2; Jarnagin et al, 2001). Longitudinal ductal tumor extension can be assessed by either MRCP, ERCP, or PTC. Duplex US and CT may be useful for assessing radial spread of tumor (Hann et al, 1997, 1998; Voyles et al, 1983).
Table 50B.2 Preoperative Tumor Staging System for Hilar Cholangiocarcinoma
| Stage | Criteria |
| T1 | Tumor involving biliary confluence ± unilateral extension to two biliary radicles |
| T2 | Tumor involving biliary confluence ± unilateral extension to two biliary radicles and ipsilateral portal vein involvement ± ipsilateral hepatic lobar atrophy |
| T3 | Tumor involving biliary confluence + bilateral extension to two biliary radicles or unilateral extension to two biliary radicles with contralateral portal vein involvement or unilateral extension to two biliary radicles with contralateral hepatic lobar atrophy or main or bilateral portal venous involvement |
From Jarnagin WR, et al, 2001: Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 234:507-519.
This preoperative clinical staging system has been compared with the AJCC classification in a series of 87 patients with cholangiocarcinoma, with no correlation seen between AJCC stage and resectability or median survival (Burke, 1998; Jarnagin et al, 2001). By contrast, the proposed staging system correlated closely with resectability, which was highest in the T1 group (59%) and decreased progressively to 0 in the T3 group (nonresectable because of extent of local disease). Other related variables also correlated with T stage, including the likelihood of an R0 resection, presence of metastatic disease, the need for partial hepatectomy, and survival (Table 50B.3). The clinical T-stage grouping was an independent predictor not only of resectability but also of the likelihood of achieving an R0 resection. The proposed clinical staging scheme underscores the importance of considering portal vein involvement and liver atrophy in relation to the extent of ductal cancer spread. Ipsilateral involvement of vessels and bile ducts is usually amenable to resection, whereas contralateral involvement is not.
Table 50B.3 Correlation of Proposed Clinical Tumor Staging System with Resectability, Metastatic Disease, and Survival
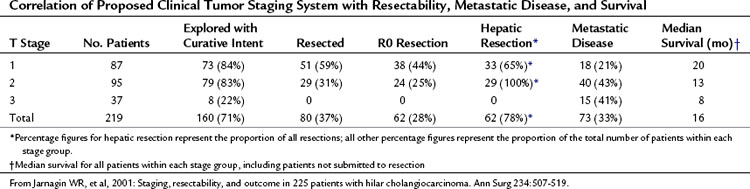
Despite advances in imaging technology, a large proportion of patients with hilar cholangiocarcinoma are found to have unresectable disease at the time of exploration. Hilar cholangiocarcinoma previously was considered more of a locally invasive disease uncommonly associated with metastases. However, in a report of 225 patients, 73 (32%) had unresectable disease; of the 160 patients submitted to exploration, 47 (29%) had metastases discovered intraoperatively that precluded a curative resection (Jarnagin et al, 2001). Given the high rate of nontherapeutic laparotomy, staging laparoscopy has been investigated as a means of improving resectability and seems to have a defined role.
Early studies examined the role of laparoscopy combined with laparoscopic US in a mixture of hepatobiliary and pancreatic malignancies and detected occult metastases in 30% to 35% of patients (Callery et al, 1997; D’Angelica et al, 2003; Jarnagin et al, 2000), but these studies included a small proportion of patients with hilar cholangiocarcinoma. Two studies showed the utility of staging laparoscopy in patients with biliary tract cancer. In a study that included 23 patients with hilar and distal cholangiocarcinoma, Vollmer and colleagues (2002) reported that laparoscopy identified 57% of patients with unresectable disease and improved resectability by 14%. Another study analyzed 56 patients, all with hilar cholangiocarcinoma, and showed similar benefit; it further showed that the yield of laparoscopy is greatest in patients with more locally advanced tumors (i.e., clinical stage T2 and T3; Weber et al, 2002). Whether fluorodeoxyglucose positron-emission tomography (FDG PET) has a role in preoperative staging is unclear (see Chapter 15). Several studies have suggested that FDG PET may identify occult metastatic disease or advanced regional lymphadenopathy (N2 disease) in a significant proportion of patients (Anderson et al, 2004; Fritscher-Ravens et al, 2001; Kluge et al, 2001); however, larger confirmatory studies are necessary before FDG PET can be recommended as routine.
As mentioned earlier, both direct cholangiography of segmental ducts and percutaneous cholangioscopy have been used to increase resectability rates for hilar cholangiocarcinoma (Kondo et al, 2004; Nimura et al, 2000). Definition of proximal and distal cancer extent and early detection of small lesions and multiple foci of cancer can be accomplished by cholangioscopic observation followed by biopsy and histologic confirmation (Nimura et al, 1988).
Treatment
Most patients with unresectable bile duct cancer die within 6 months to 1 year of diagnosis. Death usually results from liver failure or infectious complications secondary to biliary obstruction (Burke, 1998; Kuwayti et al, 1957; Okuda et al, 1977; Sako et al, 1957). In patients with unresectable disease, the prognosis has been considered worse for tumors affecting the confluence of the bile ducts and better for distal tumors close to the papilla. This difference in prognosis may reflect the relatively later presentation and the complexity of managing hilar biliary obstruction rather than a difference in biologic behavior. It has been shown that location within the biliary tree (proximal versus distal) has no impact on survival, provided complete resection is achieved (Allen et al, 2008; Nagorney et al, 1993).
Complete resection is the only effective therapy for cancers of the lower bile duct (Fong et al, 1996; Nagorney et al, 1993; Nakeeb et al, 1996b; Tompkins et al, 1981; Wade et al, 1997; Yeo et al, 1997). Meaningful experience with these relatively uncommon tumors has been limited to a few centers. In reports containing significant numbers of patients, 5-year survival rates of 40% have been reported after complete resection. In most studies, survival beyond 1 year was uncommon in patients subjected to palliative bypass or biliary intubation (Fong et al, 1996; Nakeeb et al, 1996b; Tompkins et al, 1981; Wade et al, 1997).
Operative Resection for Hilar Cholangiocarcinoma
Orthotopic liver transplantation has been attempted for hilar cholangiocarcinoma considered unresectable (see Chapter 97E). Klempnauer and colleagues (1997b) reported four long-term survivors out of 32 patients who underwent transplantation for hilar cholangiocarcinoma. The same group also reported a 5-year survival of 17% for their overall transplant group (Pichlmayr et al, 1996). Iwatsuki and colleagues (1998) reported comparable results. Data from the Mayo Clinic suggest good results with transplantation in highly selected patients with no metastatic disease on imaging or at laparotomy when combined with an intensive pretransplant treatment regimen that includes chemoradiotherapy (Heimbach et al, 2004; Rea et al, 2005). Although the data are compelling, this approach is applicable to only a small fraction of patients because of the high incidence of lymph node metastases and distant occult metastases.
In patients with potentially resectable tumors based on preoperative imaging, the primary goal should be complete resection with intent to cure. Our criterion for curative resection is complete removal of all gross disease with clear histologic margins (R0 resection). Achieving an R0 resection almost always requires a partial hepatectomy for hilar cholangiocarcinoma (Jarnagin et al, 2001). Bile duct excision with en bloc partial hepatectomy, often with en bloc caudate lobectomy (Nimura et al, 1990), is frequently necessary to achieve negative histologic margins.
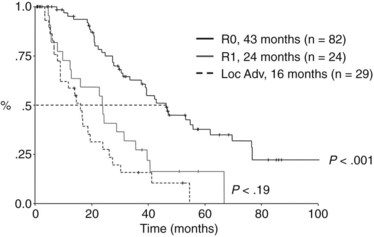
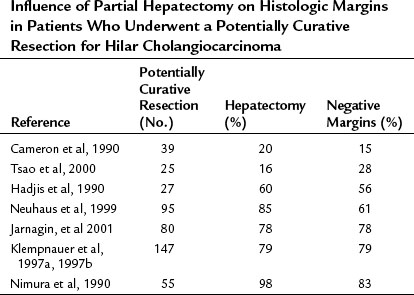
Several studies show a parallel between the number of patients undergoing partial hepatectomy and negative resection margins (Table 50B.4). We routinely use hepatic resection but perform caudate resection selectively in cases with suggested tumor extension into the ducts of the caudate lobe. The principal caudate lobe ducts drain into the left hepatic duct, and tumors extending into the left hepatic duct almost always involve the caudate duct and usually require caudate resection (Mizumoto & Suzuki, 1988). A dilated caudate duct suggestive of tumor involvement may occasionally be seen on preoperative imaging. In some cases, intraoperative frozen section of the caudate duct margin may help in making the decision to proceed to caudate resection. The importance of negative resection margins for long-term survival is confirmed by the results of several studies (see Table 50B.4). In the MSKCC experience, survival after an R1 resection (histologically involved resection margins) is similar to survival in patients with unresectable, locally advanced tumors identified at exploration (Fig. 50B.15; Endo et al, 2008b; Jarnagin et al, 2001).
Table 50B.4 Influence of Partial Hepatectomy on Histologic Margins in Patients Who Underwent a Potentially Curative Resection for Hilar Cholangiocarcinoma
Distinguishing resectable from nonresectable tumors demands careful consideration of all available clinical and imaging data. Bilateral tumor extension to second-order intrahepatic biliary radicles and, in many patients, encasement or occlusion of the main portal vein preclude a resection. The individual determinants of resectability must be considered within the context of all of the imaging findings. Ipsilateral involvement of the portal vein and bile ducts may be amenable to resection, whereas contralateral involvement usually is not. Likewise, ipsilateral lobar atrophy does not preclude resection, whereas atrophy of the contralateral lobe does. Other factors that influence resectability include the presence of significant comorbid medical conditions, significant hepatic parenchymal disease, and distant metastatic spread of tumor (Table 50B.5).
Table 50B.5 Criteria of Nonresectability in Patients with Hilar Cholangiocarcinoma
| Patient Factors |
| Medically unfit for operation |
| Cirrhosis/portal hypertension |
| Local Factors |
| Hepatic duct involvement up to secondary radicles bilaterally |
| Encasement or occlusion of the main portal vein proximal to its bifurcation |
| Atrophy of one lobe with encasement of contralateral portal vein branch |
| Atrophy of one lobe with contralateral involvement of secondary biliary radicles |
| Distant Disease |
| Histologically proven metastases to lymph node groups beyond the hepatoduodenal ligament (celiac, paraaortic, retropancreatic) |
| Histologically proven metastases to liver, lung, or peritoneum |
Invasion of the main portal vein or its branches by tumor is a major determinant of resectability. The preoperative assessment of vascular involvement and ductal extension of tumor is an essential part of operative planning and gives valuable information to the surgeon with respect to the extent of operation and operative strategy. Limited tumor involvement of the portal venous confluence or the main portal vein may be amenable to resection and portal vein reconstruction (see Chapter 91B).
Several technical steps during the exploration and resection of hilar cholangiocarcinoma are crucial to the success of the operation. Local resection—that is, resection of the extrahepatic biliary apparatus without concomitant partial hepatectomy—for small Bismuth-Corlette type I tumors not involving the major vessels may be possible. In this situation, resection must include removal of the entire supraduodenal bile duct, gallbladder, cystic duct, and extrahepatic hepatic ducts with clearance of the supraduodenal tissues, including the related lymph nodes. Even if a complete resection can be achieved without an en bloc partial hepatectomy, such local resections seem to be inferior with respect to long-term survival. In 106 resections at MSKCC, 19 were local resections, and 9 of these were considered complete or R0; however, no patient submitted to an R0 bile duct resection was among the 5-year survivors (Jarnagin et al, 2005). In most patients, the option of a local resection does not exist, however, because of intrahepatic extension of the tumor, right or left portal vein involvement, or both. In these cases, en bloc liver resection, often with caudate lobectomy, is necessary to achieve tumor clearance. In some patients, tumor adherence to the portal vein can be managed by segmental portal vein resection and reconstruction (Blumgart et al, 1984; Neuhaus et al, 1999; Nimura et al, 1991b). This procedure can be done only if intraoperative assessment shows that a tumor-free remnant with intact biliary drainage and blood supply can be left in situ. Some centrally located tumors may be amenable to a more limited hepatic resection. Such resections, which include segments IV and V or IV and I, are limited in their application (Grune et al, 1991; Miyakawa et al, 1996; Miyazaki et al, 1998a, 1998b) and are inappropriate in the face of lobar atrophy and involvement of a main portal vein branch, both of which are common findings.
Operative exploration is carried out through a right subcostal incision with proximal extension to the xiphoid, a so-called “hockey stick” incision. The exploration should begin with a thorough inspection of the peritoneal cavity and distant nodal sites, because metastatic disease is common in patients with hilar cholangiocarcinoma. In our experience, 73 (50%) of 145 unresectable patients had metastases to regional lymph nodes or distant sites (Jarnagin et al, 2001). These findings are supported by results from other series (Cameron et al, 1990; Lai et al, 1987). Careful bimanual palpation of the liver and intraoperative US are performed to rule out unsuspected masses in the liver. Palpation of the caudate lobe is performed after incision of the lesser omentum, allowing access to the lesser sac. A Kocher maneuver is performed to allow access to the retroduodenal lymph nodes, and the ligamentum teres is elevated, exposing the undersurface of the liver and allowing thorough examination of the subhilar and retroduodenal area. Precise assessment of tumor extension and biopsy of any suspicious lesions or distant lymph nodes with frozen-section analysis should be performed. Evidence of intrahepatic metastases, multicentricity within the liver, or spread to distant sites precludes resection. With any of these findings, the patient should be considered for palliative biliary drainage.
Although a segmental bile duct resection and biliary reconstruction are possible in some patients, most require partial hepatectomy to achieve complete tumor clearance. In all cases, the surgeon must be prepared to perform a liver resection. The general principles of intraoperative management are discussed in detail in other chapters within this text (see Chapter 90A, Chapter 90B, Chapter 90C, Chapter 90D, Chapter 90E, Chapter 90F, Chapter 91A, Chapter 91B ). Preparation for surgery includes suitable intraoperative monitoring and the possibility for rapid transfusion. The patient’s central venous pressure is kept at less than 5 mm Hg during the operation to keep blood loss from hepatic veins at a minimum during retrohepatic dissection, dissection of the hepatic veins, and parenchymal transection (Cunningham et al, 1994; Melendez et al, 1998).
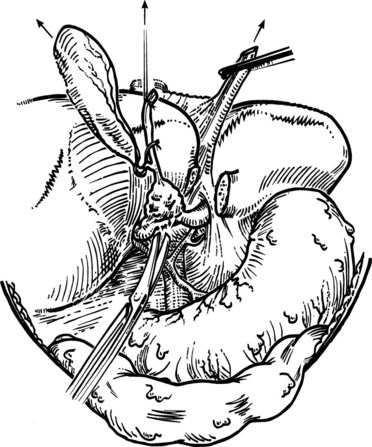
To reach the confluence of the bile ducts and assess its relationship to the portal vein, the common bile duct first must be transected above the duodenum and turned upward. The liver hilus is fully exposed anteriorly by taking down the gallbladder and lowering the hilar plate by incising the Glisson capsule along the base of segment IV. Exposure of the left hepatic duct is improved by dividing the bridge of liver tissue that often connects the base of segment IV and the left lateral segment; this may be quite substantial in some patients. The entire extrahepatic biliary apparatus and adjacent lymphatic tissues are turned upward to expose the portal vein. A plane can be developed easily between the posterior aspect of the bile duct tumor and the portal vein, provided no tumor has invaded into the vessels (Fig. 50B.16). The dissection is continued upward toward the hilus, skeletonizing the portal vein and hepatic artery.
At this point, the surgeon should assess the proximal extent of tumor by palpation and, if necessary, by biopsy. Segmental bile duct resection is possible only if an adequate length of the hepatic ducts can be achieved beyond the tumor, and if no vascular involvement is evident. If the tumor extends to the second-order biliary radicles unilaterally such that clearance cannot be achieved, or if the ipsilateral portal vein branch is involved, partial hepatectomy must be performed. Tumors extending well into the left hepatic duct may involve the caudate ducts as well and require en bloc caudate lobectomy (Mizumoto et al, 1986; Mizumoto & Suzuki, 1988). If partial hepatectomy is required, inflow control is obtained by ligation and transection of the ipsilateral branch of the portal vein and hepatic artery. Extrahepatic control and division of the ipsilateral hepatic vein are performed before parenchymal transection.
When it has been established that segmental bile duct excision is feasible and will result in an R0 resection, the left and right hepatic ducts are divided above the tumor. Occasionally, unresectability as a result of main portal vein invasion or extensive bilateral intrahepatic duct involvement (see Table 50B.5) will not be determined until the extrahepatic biliary tree has been divided and mobilized. In both of these situations, biliary-enteric continuity is restored by hepaticojejunostomy to a Roux-en-Y loop of jejunum. When residual disease remains at the final level of the transected duct, appropriate consideration should be made for placement of retrograde transhepatic biliary stents (Fig. 50B.17). After removal of the tumor, the surgeon may be faced with multiple exposed duct orifices, all of which require suitable drainage (see Chapters 29 and 42A). Frequently, removal of the tumor results in discontinuity of the right anterior and posterior sectoral ducts, separation of one or more caudate ducts from the left hepatic duct, or both. The sidewalls of adjacent ducts can be brought into apposition with sutures and regarded as a single duct for purposes of anastomosis. In cases of multiple exposed ducts, it is often possible to make it so that no more than two or three separate ducts need to be anastomosed. A Roux-en-Y loop of jejunum is prepared and brought up, usually in a retrocolic fashion, and anastomosis is carried out in an end-to-side fashion between the exposed ducts and the side of the jejunal loop using a single layer of 4-0 interrupted polyglactin 910 (Vicryl) sutures (Blumgart & Kelley, 1985; Voyles & Blumgart, 1982). Anastomotic techniques are illustrated and discussed in more detail in other chapters.
Operative Resection for Distal Cholangiocarcinoma
Resection of most distal bile duct cancers requires pancreatoduodenectomy (see Chapter 62A). Compared with patients with pancreatic cancer, those with distal bile duct cancer are more often amenable to resection, less often have microscopic disease at the resection margin, and less frequently have spread of tumor to adjacent lymph nodes (Fong et al, 1996; Nakeeb et al, 1996a, 1996b; Yeo et al, 1997). In addition to completeness of resection, lymph node status is a crucial determinant of outcome. Fong and colleagues (1996) found that lymph node status was the only independent predictor of long-term survival in resected patients, with positive nodes conferring a 6.7 times greater likelihood of recurrence and death. Similarly, Wade and colleagues (1997) identified no survivors beyond 3 years with involved regional lymph nodes, and Nakeeb and colleagues (1996a, 1996b) found that lymph node status and tumor differentiation were independent predictors of outcome.
Outcomes after Operation
Long-term survival can be achieved with an acceptable operative mortality (Ahrendt et al, 1998; Baer et al, 1993; Hadjis et al, 1990; Hasegawa et al, 2007; Haswell-Elkins et al, 1991; Hemming et al, 2005; Jarnagin et al, 2001; Klempnauer et al, 1997a; Kondo et al, 2004; Nagata et al, 1990; Nagorney et al, 1993; Nakeeb et al, 1996a, 1996b; Neuhaus et al, 1999; Nimura et al, 1990, 2000; Parc et al, 1997; Pichlmayr et al, 1996; Rosen et al, 1991; Sano et al, 2006; Wolber et al, 1991). Five-year survival rates range from 25% to 40%, and status of the resection margins is crucial to obtaining such results. Several studies have shown that patients resected with negative histologic margins survive significantly longer than those with involved margins (Ahrendt et al, 1998; Endo et al, 2008b; Hadjis et al, 1990; Jarnagin et al, 2001; Lupi et al, 1990; Pichlmayr et al, 1996).
Since the 1980s, the use of hepatic resection in patients with hilar cholangiocarcinoma has increased steadily. We believe this increase is responsible for the increase in the percentage of R0 resections (negative histologic margins) and the observed improvement in survival after resection (Saldinger & Blumgart, 2000). In addition to status of the resection margin, many other variables have been shown to have an impact on outcome, including tumor involvement of regional lymph nodes, tumor grade or differentiation, and tumor morphology (e.g., papillary versus nodular sclerosing) (Ebata et al, 2003; Jarnagin et al, 2005). The issue of lymph node metastases, their impact on outcome, and extent of lymphadenectomy remain points of some controversy. Some authors have reported long-term survivors, even with involved paraaortic lymph nodes, and have argued for extended lymphadenectomy as a routine part of the resection procedure (Kitagawa et al, 2001). Examination of several series in which 5-year survival is documented suggests, however, that involved lymph nodes are a powerful adverse prognostic variable. We do not advocate extended lymph node dissection, and we consider metastatic involvement of distant lymph node basins (N2 disease) to represent unresectable disease.
In many prior studies, the operative mortality associated with hilar cholangiocarcinoma, including partial hepatectomy, was on the order of 10%. In an effort to improve these figures, numerous centers have adopted an approach that combines extensive preoperative biliary drainage and PVE, as discussed previously. Using such an approach, Sano and colleagues (2006) reported 102 consecutive resections without operative mortality. A major rationale for using these preoperative procedures is to reduce the incidence of postoperative hepatic failure associated with extended resections in the setting of biliary obstruction.
The combined data from the literature suggest that survival after resection of adenocarcinoma of the distal bile duct is at least as good as and probably better than that for pancreatic cancer (Fong et al, 1996; Wade et al, 1997). It has long been assumed that survival after resection of distal bile duct tumors is greater than after resection of hilar cholangiocarcinomas (Tompkins et al, 1981). This assumption is almost certainly erroneous and likely evolved from older reports that did not take into account the status of resection margins in patients with hilar tumors. If adjusted for stage and completeness of resection, the survival rates seem to be comparable (Allen et al, 2008; Nagorney et al, 1993).
Adjuvant Therapy after Operative Resection
Several single-arm studies have investigated the benefit of postoperative adjuvant radiation therapy in patients with hilar cholangiocarcinoma. Two separate reports from Johns Hopkins (Cameron et al, 1990; Pitt et al, 1995b) showed no benefit of adjuvant external beam and intraluminal radiation therapy. Kamada and associates (1996) suggested that radiation might improve survival in patients with histologically positive hepatic duct margins. Additionally, in a small series of patients (five with hilar cholangiocarcinoma), resectability was reportedly greater in patients given neoadjuvant radiation therapy before exploration (McMasters et al, 1997). None of these studies was randomized, however, and most consist of a small, heterogeneous group of patients. At present, no data are available to support the routine use of adjuvant or neoadjuvant radiation therapy except in the context of a controlled trial.
Takada and associates (2002) reported results of a Phase III multicenter randomized study evaluating the potential benefit of adjuvant systemic chemotherapy after resection of pancreatobiliary tumors. This study found no benefit of adjuvant systemic 5-fluorouracil (5-FU) and mitomycin C compared with surgery alone for patients with bile duct carcinoma. Whether newer agents, such as gemcitabine and/or oxaliplatin, have a role in the adjuvant setting remains to be determined.
Adjuvant therapy (chemotherapy and/or radiation therapy) after resection has not been shown to improve survival for distal bile duct cancer, although this issue has not been evaluated in a prospective fashion for a homogeneous population of patients with distal cholangiocarcinoma only (Nakeeb et al, 1996b).
Palliative Therapy
Most patients with hilar cholangiocarcinoma are not suitable for resection. In this setting, management options include some form of biliary decompression or supportive care. Jaundice alone, without pruritus or cholangitis, is not an indication for biliary decompression. For biliary decompression in inoperable patients, our current indications are to relieve intractable pruritus, treat cholangitis, gain access for intraluminal radiotherapy, and allow recovery of hepatic parenchymal function in patients who are potential candidates for chemotherapy. Supportive care alone is probably the best approach for elderly patients with significant comorbid conditions, provided that pruritus is not a major feature. Patients who are found to be unresectable at operation represent a different group, and operative biliary decompression usually is performed successfully (Burke, 1998) and can be constructed to provide access to the biliary tree for postoperative irradiation (see Fig. 50B.17; Kuvshinoff et al, 1995).
Assessment of palliative biliary drainage procedures is difficult, because the spectrum of patients ranges from those critically ill and unresectable to those in relatively good health with potentially resectable tumors. All patients should be assessed properly by experienced personnel with a view toward possible resection. This point cannot be overemphasized: If the patient is deemed unresectable, the diagnosis should be confirmed with a biopsy. Biliary decompression can be achieved by percutaneous transhepatic puncture or by endoscopic stent placement (see Chapters 27, 28, and 50D). Hilar tumors are more difficult to traverse with the endoscopic technique, which should only be approached by skilled endoscopists with extensive ERCP experience. The failure rates and incidence of subsequent cholangitis after endoscopic drainage can be high (Liu et al, 1998). For this reason, initial endobiliary drainage, even in the palliative setting, should utilize plastic stents. Exchange for metallic stents can be considered after close monitoring for adequate palliative biliary drainage with plastic stents in the short and intermediate term.
Percutaneous transhepatic biliary drainage and subsequent placement of a self-expandable metallic endoprosthesis can be performed successfully in most patients with hilar obstruction. Satisfactory results, even with experienced interventional radiologists, are more difficult to achieve in patients with hilar tumors than in patients with distal biliary obstruction (Becker et al, 1993; Cheung & Lai, 1995; Miyazaki et al, 1998a, 1998b; see Chapters 28 and 50D). Satisfactory drainage of only 25% to 30% of functional hepatic parenchyma is required for resolution of jaundice. Still, hilar tumors frequently isolate all three major hilar ducts—left hepatic, right anterior sectoral hepatic, and right posterior sectoral hepatic—and two or more uncovered stents must be placed for adequate drainage (Fig. 50B.18; Schima et al, 1997). Bilateral drainage is not better or more effective than unilateral drainage, provided that an adequate volume of liver parenchyma can be decompressed (De Palma et al, 2001). It also must be considered that jaundice may result from hepatic dysfunction secondary to portal vein occlusion. Jaundice in this setting, without intrahepatic biliary dilation, is not correctable with biliary stents. In addition, lobar atrophy is an important factor when considering palliative biliary procedures. Percutaneous drainage through an atrophic lobe does not relieve jaundice and should be avoided. The presence of multiple intrahepatic metastases or ascites also may add to the technical difficulty of the procedure.
The median patency of metallic endoprostheses at the hilus is approximately 6 months (Glattli et al, 1993), significantly less than that reported for similar stents placed in the distal bile duct. Becker and colleagues (1993) reported 1-year patency rates of 46% and 89% for metal stents placed at the hilus and at the distal bile duct. Similarly, Stoker and Lameris (1993) documented occlusion in 36% of patients at the hilus compared with 6% of patients with self-expanding metal stents (SEMS) in the distal bile duct. In most series of SEMS placed for hilar obstruction, documented stent occlusion requiring reintervention occurs in 25% of patients (Becker et al, 1993; Bergquist et al, 1998; Glattli et al, 1993; Hurlimann & Gardiol, 1991; Rossi et al, 1994; Schima et al, 1997; Stoker & Lameris, 1993). This percentage concurs with our findings of a mean patency of 6.1 months in 35 patients palliated for malignant high biliary obstruction by placement of expandable metallic endoprostheses. The periprocedural mortality was 14% at 30 days, and seven patients (24%) had documented stent occlusion that required repeated intervention (Glattli et al, 1993). In a recent prospective trial, patients presenting for percutaneous biliary drainage for malignant biliary obstruction had a dismal survival and experienced no improvement in quality of life with drainage. The exception in this trial was an improvement in pruritus-related quality of life, which was significantly better (Robson et al, 2010).
Palliating distal biliary obstruction in unresectable patients can be achieved with an operative bypass (hepaticojejunostomy or choledochojejunostomy) or with placement of a biliary stent. Endoprostheses for distal biliary obstruction are typically easy to place and have a greater long-term patency than endoprostheses placed for hilar obstruction (Becker et al, 1993). Operative biliary-enteric bypass, either open or laparoscopic, will provide excellent relief of jaundice and can be done with an acceptably low morbidity and mortality. Patients who are found to have unresectable disease at the time of operative exploration should undergo biliary-enteric bypass. Planned palliative operative bypass should be reserved for patients expected to survive greater than 6 months (van den Bosch et al, 1994), and endoscopic SEMS should be used in patients with clear-cut metastatic disease on cross-sectional imaging or discovered with staging laparoscopy.
Patients with hilar tumors who are found to be unresectable at operation may be candidates for hepaticojejunostomy or intrahepatic biliary-enteric bypass. The segment III duct usually is the most accessible and is our preferred approach, but the right anterior or posterior sectoral hepatic ducts also can be used (Jarnagin et al, 1998; see Chapter 42A). Typically, a segment III bypass is used to restore biliary-enteric continuity after the bile duct has been divided and a locally invasive, unresectable tumor has been discovered. Segment III bypass provides excellent biliary drainage and is less prone to occlusion by tumor than a SEMS (Stoker & Lameris, 1993), because the anastomosis can be placed some distance away from the tumor (Fig. 50B.19). Relief of jaundice is achieved if at least one third of the functioning hepatic parenchyma is adequately drained. Communication between the right and left hepatic ducts is unnecessary, provided the undrained lobe has not been percutaneously drained or otherwise contaminated (Baer et al, 1994). In this circumstance, there is a high risk of persistent biliary fistula and cholangitis. Bypass to an atrophic lobe or a lobe heavily involved with tumor is ineffective. In a report of 55 consecutive bypasses in patients with malignant hilar obstruction, segment III bypass in patients with hilar cholangiocarcinoma (n = 20) yielded the best results. The 1-year bypass patency in this group was 80%, with no perioperative deaths (Jarnagin et al, 1998).
Patients with unresectable, locally advanced tumors but without evidence of widespread disease may be candidates for palliative radiation therapy. A combination of external beam radiation (5000 to 6000 cGy) and intraluminal iridium-192 (2000 cGy) delivered percutaneously is typically used. Several authors have shown the feasibility of this approach, but improved survival compared with biliary decompression alone has not been documented in a controlled study (Bowling et al, 1996; Cameron et al, 1990; Kuvshinoff et al, 1995; Nagano et al, 1990; Vallis et al, 1996; Vatanasapt et al, 1990a). In a group of 12 patients treated with this regimen over 3 years at MSKCC, the median survival was 14.5 months. Episodes of cholangitis and intermittent jaundice were relatively common, but the incidence of serious complications was low, and there were no treatment-related deaths (Kuvshinoff et al, 1995). Cameron and colleagues (1990) reported improved survival in irradiated patients compared with a group of patients not irradiated; however, the median survival in both groups was less than 1 year. Other investigators reported no benefit and questioned the routine use of radiation, given the increased incidence of complications and greater time spent in the hospital (Bowling et al, 1996). Radiation therapy is inappropriate in patients with widespread disease. Systemic chemotherapy is the only option for these patients, but response rates are low (Patt et al, 1996).
Ortner and colleagues (1998) evaluated the efficacy of photodynamic therapy in unresectable hilar cholangiocarcinoma. This method has been used in the treatment of tumors of the esophagus, colon, stomach, bronchus, bladder, and brain. It is a two-step procedure. First, a photosensitizer is injected; second, direct illumination via cholangioscopy activates the compound, causing tumor cell death. Ortner and colleagues (1998) treated nine patients in this fashion who had not responded to endoscopic stenting. They reported zero mortality for the procedure; however, a 25% mortality rate was related to the initial endoscopic stenting, which must be considered. These investigators did not mention their indication for biliary drainage. This information is important to assess the extent of disease before therapy. Detailed reasons for nonresectability were not discussed, and the reported median survival of 439 days is difficult to interpret. The data presented in this report, including decrease in bilirubin and some improved quality of life, are insufficient to advocate routine use of this method. Two randomized studies in patients with unresectable cholangiocarcinoma suggested improved survival with biliary stenting combined with photodynamic therapy compared with biliary stenting alone (Ortner et al, 2003; Zoepf et al, 2005). The improved survival observed with photodynamic therapy is likely related to better biliary decompression and avoidance of early segmental duct isolation and subsequent cholangitis, rather than any significant reduction in tumor burden (Quyn et al, 2009).
Palliative systemic chemotherapy has been investigated. Two phase II studies analyzing the effect of 5-FU combined with interferon alfa-2b and the effect of paclitaxel failed to show any benefit (Jones et al, 1996; Patt et al, 1996). In more recent studies, gemcitabine and irinotecan seemed to have limited efficacy, although they may offer a higher response rate than that seen with 5-FU–based regimens, (Alberts et al, 2005; Park et al, 2005; Sanz-Altamira et al, 2001). A recent Phase III study by the investigators of the Advanced Biliary Cancer (ABC) 02 trial randomized 410 patients with locally advanced or metastatic cholangiocarcinoma, gallbladder cancer, or ampullary cancer to receive either cisplatin followed by gemcitabine or gemcitabine alone for up to 6 months (Valle et al, 2010). This study showed an improvement in median survival from 8.2 to 11.7 months for patients receiving cisplatin plus gemcitabine without the addition of substantial toxicity.
Abdalla EK, et al. Extended hepatectomy in patients with hepatobiliary malignancies with and without preoperative portal vein embolization. Arch Surg. 2002;137:675-681.
Ahrendt SA, et al. Primary sclerosing cholangitis: resect, dilate, or transplant? Ann Surg. 1998;227:412-423.
Alberts SR, et al. Gemcitabine, 5-fluorouracil, and leucovorin in advanced biliary tract and gallbladder carcinoma: a North Central Cancer Treatment Group phase II trial. Cancer. 2005;103:111-118.
Allen PJ, et al. Extrahepatic cholangiocarcinoma: a comparison of patients with resected proximal and distal lesions. HPB (Oxford). 2008;10(5):341-346.
Anderson CD, et al. Fluorodeoxyglucose PET imaging in the evaluation of gallbladder carcinoma and cholangiocarcinoma. J Gastrointest Surg. 2004;8:90-97.
Are C, et al. Differential diagnosis of proximal biliary obstruction. Surgery. 2006;140(5):756-763.
Bach AM, et al. Portal vein evaluation with US: comparison to angiography combined with CT arterial portography. Radiology. 1996;201:149-154.
Baer HU, et al. Management of the Mirizzi syndrome and the surgical implications of cholecystcholedochal fistula. Br J Surg. 1990;77:743-745.
Baer HU, et al. Improvements in survival by aggressive resections of hilar cholangiocarcinoma. Ann Surg. 1993;217:20-27.
Baer HU, et al. The effect of communication between the right and left liver on the outcome of surgical drainage for jaundice due to malignant obstruction at the hilus of the liver. HPB Surg. 1994;8(1):27-31.
Baere T, et al. Portal vein embolization: utility for inducing left hepatic lobe hypertrophy before surgery. Radiology. 1993;188:73-77.
Becker CD, et al. Percutaneous palliation of malignant obstructive jaundice with the Wallstent endoprosthesis: follow-up and reintervention in patients with hilar and non-hilar obstruction. J Vasc Interv Radiol. 1993;4:597-604.
Bergquist A, et al. Risk factors and clinical presentation of hepatobiliary carcinoma in patients with primary sclerosing cholangitis: a case-control study. Hepatology. 1998;27:311-316.
Bismuth H, et al. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992;215:31-38.
Blumgart LH, Kelley CJ. Hepaticojejunostomy in benign and malignant high bile duct stricture: approaches to the left hepatic ducts. Schweiz Rundsch Med Prax. 1985;74:1238-1244.
Blumgart LH, et al. Surgical approaches to cholangiocarcinoma at confluence of hepatic ducts. Lancet. 1984;1:66-70.
Bowling TE, et al. A retrospective comparison of endoscopic stenting alone with stenting and radiotherapy in non-resectable cholangiocarcinoma. Gut. 1996;39:852-855.
Broome U, et al. Natural history and prognostic factors in 305 Swedish patients with primary sclerosing cholangitis. Gut. 1996;38:610-615.
Burke EC. Hilar cholangiocarcinoma: patterns of spread, the importance of hepatic resection for curative operation, and a presurgical clinical staging system. Ann Surg. 1998;228:385-394.
Cabooter M, et al. Mirizzi syndrome. Ned Tijdschr Geneeskd. 1990;134:708-711.
Callery MP, et al. Staging laparoscopy with laparoscopic ultrasonography: optimizing resectability in hepatobiliary and pancreatic malignancy. J Am Coll Surg. 1997;185:33-39.
Cameron JL, et al. Management of proximal cholangiocarcinomas by surgical resection and radiotherapy. Am J Surg. 1990;159:91-98.
Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer. 1995;75:171-190.
Chang WH, et al. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998;47:354-362.
Chen DW, et al. Immediate and long-term outcomes of hepatectomy for hepatolithiasis. Surgery. 2004;135:386-393.
Cheung KL, Lai EC. Endoscopic stenting for malignant biliary obstruction. Arch Surg. 1995;130:204-207.
Chu KM, et al. Malignancy associated with hepatolithiasis. Hepatogastroenterology. 1997;44:352-357.
Clements WBD, et al. Biliary drainage in obstructive jaundice: experimental and clinical aspects. Br J Surg. 1993;80:834-842.
Corvera C, et al. Clinical and pathologic features of proximal biliary strictures masquerading as hilar cholangiocarcinoma. J Am Coll Surg. 2005;201:862-869.
Cunningham JD, et al. One hundred consecutive hepatic resections: blood loss, transfusion, and operative technique. Arch Surg. 1994;129:1050-1056.
D’Angelica M, et al. The role of staging laparoscopy in hepatobiliary malignancy: prospective analysis of 401 cases. Ann Surg Oncol. 2003;10:183-189.
Denning DA, et al. Preoperative percutaneous transhepatic biliary decompression lowers operative mortality in patients with obstructive jaundice. Am J Surg. 1981;141:61-65.
De Palma GD, et al. Unilateral versus bilateral endoscopic hepatic ductdrainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001;53:547-553.
Ebata T, et al. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg. 2003;238:720-727.
Elias D, et al. Preoperative selective portal vein embolization before hepatectomy for liver metastases: long-term results and impact on survival. Surgery. 2002;131:294-299.
Endo I, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008;248(1):84-96.
Endo I, et al. Clinical significance of intraoperative bile duct margin assessment for hilar cholangiocarcinoma. Ann Surg Oncology. 2008;15(8):2104-2112.
Enjoji M, et al. Integrins: utility as cell type- and stage-specific markers for hepatocellular carcinoma and cholangiocarcinoma. In Vitro Cell Dev Biol Anim. 1998;34:25-27. (letter)
Farges O, et al. Portal vein embolization before right hepatectomy: prospective clinical trial. Ann Surg. 2003;237:208-217.
Farley DR, et al. “Natural history” of unresected cholangiocarcinoma: patient outcome after noncurative intervention. Mayo Clin Proc. 1995;70:425-429.
Felekouras E, et al. Malignant carcinoid tumors of the cystic duct. HPB. 2009;8(6):640-646.
Fong Y, et al. Outcome of treatment for distal bile duct cancer. Br J Surg. 1996;83:1712-1715.
Fritcher EG, et al. A multivariable model using advanced cytologic methods for the evaluation of indeterminate pancreatobiliary strictures. Gastroenterology. 2009;136:2180-2186.
Fritscher-Ravens A, et al. FDG PET in the diagnosis of hilar cholangiocarcinoma. Nucl Med Commun. 2001;22:1277-1285.
Georgopoulos SK, et al. A comparison of magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) in malignant pancreaticobiliary obstruction. Arch Surg. 1999;134:1002-1007.
Gholson CF, Burton FR. Obstructive jaundice: nonsurgical options for surgical jaundice. Postgrad Med. 1991;90:107-110.
Gibson RN, et al. Bile duct obstruction: radiologic evaluation of level, cause, and tumor resectability. Radiology. 1986;160:43-47.
Glättli A, et al. Unresectable malignant biliary obstruction: treatment by self-expandable biliary endoprostheses. HPB Surg. 1993;6:175-184.
Greenlee RT, et al. Cancer statistics, 2001. CA Cancer J Clin. 2001;51:15-36.
Grune S, et al. Primary sclerosing cholangitis. Dtsch Med Wochenschr. 1991;116:1095-1100.
Gundy SR, et al. Efficacy of preoperative biliary tract decompression in patients with obstructive jaundice. Arch Surg. 1994;119:703-708.
Guthrie JA, et al. Hilar cholangiocarcinomas: T2-weighted spin-echo and gadolinium-enhanced FLASH MR imaging. Radiology. 1996;201:347-351.
Hadjis NS, Blumgart LH. Role of liver atrophy, hepatic resection and hepatocyte hyperplasia in the development of portal hypertension in biliary disease. Gut. 1987;28:1022-1028.
Hadjis NS, et al. Malignant masquerade at the hilum of the liver. Br J Surg. 1985;72:659-661.
Hadjis NS, et al. Outcome of radical surgery in hilar cholangiocarcinoma. Surgery. 1990;107:597-604.
Hakamada K, et al. Late development of bile duct cancer after sphincteroplasty: a ten- to twenty-two-year follow-up study. Surgery. 1997;121:488-492.
Hann LE, et al. Cholangiocarcinoma at the hepatic hilus: sonographic findings. Am J Roentgenol. 1997;168:985-989.
Hann LE, et al. Tumor involvement in hepatic veins: comparison of MR imaging and US for preoperative assessment. Radiology. 1998;206:651-656.
Hasegawa S, et al. Surgical resection of hilar cholangiocarcinoma: analysis of survival and postoperative complications. World J Surg. 2007;31:1256-1263.
Haswell-Elkins MR, et al. Immune responsiveness and parasite-specific antibody levels in human hepatobiliary disease associated with Opisthorchis viverrini infection. Clin Exp Immunol. 1991;84:213-218.
Hatfield ARW, et al. Preoperative external biliary drainage in obstructive jaundice: a prospective controlled trial. Lancet. 1982;2:896-899.
Heimbach JK, et al. Transplantation for hilar cholangiocarcinoma. Liver Transplant. 2004;10(Suppl 2):S65-S68.
Hemming AW, et al. Preoperative portal vein embolization for extended hepatectomy. Ann Surg. 2003;237:686-691.
Hemming AW, et al. Surgical management of hilar cholangiocarcinoma. Ann Surg. 2005;241:693-699.
Hewitt PM, et al. Choledochal cyst in pregnancy: a therapeutic dilemma. J Am Coll Surg. 1995;181:237-240.
Hochwald SN, et al. Preoperative biliary stenting is associated with increased post-operative infectious complications in proximal cholangiocarcinoma. Arch Surg. 1999;134:261-266.
Hoevels J, Ihse I. Percutaneous transhepatic portography in bile duct carcinoma: correlation with percutaneous transhepatic cholangiography and angiography. Fortesch Roentgenstr. 1979;131:140-150.
Holzinger F, et al. Mechanisms of biliary carcinogenesis. Ann Oncol. 1999;10:122-126.
Hurlimann J, Gardiol D. Immunohistochemistry in the differential diagnosis of liver carcinomas. Am J Surg Pathol. 1991;15:280-288.
Itoh S, et al. Three-phase CT examination of the pancreatobiliary region using multislice CT with 1-mm collimation. Radiat Med. 2005;23:283-291.
Iwatsuki S, et al. Treatment of hilar cholangiocarcinoma (Klatskin tumors) with hepatic resection or transplantation. J Am Coll Surg. 1998;187:358-364.
Iyomasa S, et al. Successful management of preoperative cholangitis by percutaneous transhepatic biliary drainage: case report of advanced gallbladder carcinoma with severe cholangitis. J Hepatobiliary Pancreat Surg. 1994;1:424-428.
Jarnagin WR, et al. Intrahepatic biliary enteric bypass provides effective palliation in selected patients with malignant obstruction at the hepatic duct confluence. Am J Surg. 1998;175:453-460.
Jarnagin WR, et al. A prospective analysis of staging laparoscopy in patients with primary and secondary hepatobiliary malignancies. J Gastrointest Surg. 2000;4:34-43.
Jarnagin WR, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507-519.
Jarnagin WR, et al. Papillary phenotype confers improved survival after resection of hilar cholangiocarcinoma. Ann Surg. 2005;241:703-712.
Jeng KS, et al. Coexisting sharp ductal angulation with intrahepatic biliary strictures in right hepatolithiasis. Arch Surg. 1994;129:1097-1102.
Jones BA, et al. Periampullary tumours: which ones should be resected? Am J Surg. 1985;149:46-51.
Jones DVJr, et al. Phase II study of paclitaxel therapy for unresectable biliary tree carcinomas. J Clin Oncol. 1996;14:2306-2310.
Jutte DL, et al. Carcinoid tumor of the biliary system: case report and literature review. Dig Dis Sci. 1987;32:763-769.
Kamada T, et al. The role of radiotherapy in the management of extrahepatic bile duct cancer: an analysis of 145 consecutive patients treated with intraluminal and/or external beam radiotherapy. Int J Radiat Oncol Biol Physics. 1996;34:767-774.
Katoh H, et al. Character of a human cholangiocarcinoma CHGS, serially transplanted to nude mice. Hum Cell. 1988;1:101-105.
Kawasaki S, et al. Radical operation after portal embolization for tumor of hilar bile duct. J Am Coll Surg. 1994;178:480-486.
Kawasaki S, et al. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg. 2003;238:84-92.
Kennedy TJ, et al. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB. 2009;11(5):445-451.
Khan SA, et al. Cholangiocarcinoma. Lancet. 2005;366:1303-1314.
Kinoshita H, et al. Preoperative portal vein embolization for hepatocellular carcinoma. World J Surg. 1986;10:803-808.
Kipp BR, et al. Comparison of KRAS mutation analysis and FISH for detecting pancreatobiliary tract cancer in cytology specimens collected during endoscopic retrograde cholangiopancreatography. J Molec Diagnostics. 2010;12:780-786.
Kitagawa Y, et al. Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg. 2001;233:385-392.
Klempnauer J, et al. Resectional surgery of hilar cholangiocarcinoma: a multivariate analysis of prognostic factors. J Clin Oncol. 1997;15:947-954.
Klempnauer J, et al. What constitutes long-term survival after surgery for hilar cholangiocarcinoma? Cancer. 1997;79:26-34.
Kluge R, et al. Positron emission tomography with [(18)F]fluoro-2-deoxy-D-glucose for diagnosis and staging of bile duct cancer. Hepatology. 2001;33:1029-1035.
Kondo S, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240:95-101.
Kubo S, et al. Hepatolithiasis associated with cholangiocarcinoma. World J Surg. 1995;19:637-641.
Kuvshinoff BW, et al. Palliation of irresectable hilar cholangiocarcinoma with biliary drainage and radiotherapy. Br J Surg. 1995;82:1522-1525.
Kuwayti K, et al. Carcinoma of the major intrahepatic and the extrahepatic bile ducts exclusive of the papilla of Vater. Surg Gynecol Obstet. 1957;104:357-366.
Lai EC, et al. Proximal bile duct cancer: quality of survival. Ann Surg. 1987;205:111-118.
Launois B, et al. Carcinoma of the hepatic hilus: surgical management and the case for resection. Ann Surg. 1979;190:151-157.
Lee JC, et al. Analysis of K-ras gene mutations in periampullary cancers, gallbladder cancers and cholangiocarcinomas from paraffin-embedded tissue sections. J Formos Med Assoc. 1995;94:719-723.
Lee MG, et al. Extrahepatic biliary diseases: 3D MR cholangiopancreatography compared with endoscopic retrograde cholangiopancreatography. Radiology. 1997;202(3):663-669.
Levi S, et al. Multiple K-ras codon 12 mutations in cholangiocarcinomas demonstrated with a sensitive polymerase chain reaction technique. Cancer Res. 1991;51:3497-3502.
Lipsett PA, et al. Choledochal cyst disease: a changing pattern of presentation. Ann Surg. 1994;220:644-652.
Liu CL, et al. Endoscopic retrograde cholangiopancreatography and endoscopic endoprosthesis insertion in patients with Klatskin tumors. Arch Surg. 1998;133:293-296.
Lupi L, et al. The CT and US aspects in hepatic cholangiocarcinoma due to thorium dioxide (Thorotrast): a case report and review of the literature. Radiol Med. 1990;79:399-401.
Makuuchi M, et al. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990;107:521-527.
McMasters KM, et al. Neoadjuvant chemoradiation for extrahepatic cholangiocarcinoma. Am J Surg. 1997;174:605-609.
McPherson GA, et al. Pre-operative percutaneous transhepatic biliary drainage: the results of a controlled trial. Br J Surg. 1984;71:371-375.
Meade CJ, et al. Serum PAF-acetylhydrolase in severe renal or hepatic disease in man: relationship to circulating levels of PAF and effects of nephrectomy or transplantation. J Lipid Mediat Cell Signal. 1994;9:205-215.
Melendez JA, et al. Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg. 1998;187:620-625.
Miyakawa S, et al. Arterial reconstruction of the posterior segment after central bisegmentectomy and caudate lobectomy. Hepatogastroenterology. 1996;43:225-228.
Miyazaki M, et al. Aggressive surgical approaches to hilar cholangiocarcinoma: hepatic or local resection? Surgery. 1998;123:131-136.
Miyazaki M, et al. Segments I and IV resection as a new approach for hepatic hilar cholangiocarcinoma. Am J Surg. 1998;175:229-231.
Mizumoto R, et al. Surgical treatment of hilar carcinoma of the bile duct. Surg Gynecol Obstet. 1986;162:153-158.
Mizumoto R, Suzuki H. Surgical anatomy of the hepatic hilum with special reference to the caudate lobe. World J Surg. 1988;12:2-10.
Nagano H, et al. Intraarterial and intraportal chemotherapy combined with decollateralization for cholangiocellular carcinoma and metastatic liver cancer. Jpn J Cancer Chemother. 1990;17:1758-1762.
Nagata Y, et al. Radiofrequency thermotherapy for malignant liver tumors. Cancer. 1990;65:1730-1736.
Nagino M. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg. 2006;243:364-372.
Nagino M, et al. Percutaneous transhepatic biliary drainage in patients with malignant biliary obstruction of the hepatic confluence. Hepatogastroenterology. 1992;39:296-300.
Nagino M, et al. Changes in hepatic lobe volume in biliary tract cancer patients after right portal vein embolization. Hepatology. 1995;21:434-439.
Nagorney DM, et al. Outcomes after curative resections of cholangiocarcinoma. Arch Surg. 1993;128:871-879.
Nakamura K, et al. Combined use of surgical treatment and postoperative radiotherapy for carcinoma of the extrahepatic bile ducts (author’s transl). J Jpn Soc Cancer Ther. 1981;16:194-203.
Nakayama T, et al. Percutaneous transhepatic bile drainage. Gastroenterology. 1978;74:554-559.
Nakeeb A, et al. Biliary carcinoembryonic antigen levels are a marker for cholangiocarcinoma. Am J Surg. 1996;171:147-153.
Nakeeb A, et al. Cholangiocarcinoma: a spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996;224:463-475.
Neuhaus P, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230:808-818.
Nimura Y. Surgical anatomy of the biliary ducts. In: Rossi, P, editor. Biliary Tract Radiology. Berlin: Springer-Verlag; 1997:21-30.
Nimura Y, et al. Value of percutaneous transhepatic cholangioscopy. Surg Endosc. 1988;2:213-217.
Nimura Y, et al. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 1990;14:535-544.
Nimura Y, et al. Combined portal vein and liver resection for carcinoma of the biliary tract. Br J Surg. 1991;78:727-731.
Nimura Y, et al. Hepatopancreatoduodenectomy for advanced carcinoma of the biliary tract. Hepatogastroenterology. 1991;38:170-175.
Nimura Y, et al. Technique of inserting multiple biliary drainage and management. Hepatogastroenterology. 1995;42:323-331.
Nimura Y, et al. Aggressive preoperative management and extended surgery for hilar cholangiocarcinoma: Nagoya experience. J Hepatobiliary Pancreat Surg. 2000;7:155-162.
Norlander A, et al. Effect of percutaneous transhepatic drainage upon liver function and postoperative mortality. Surg Gynecol Obstet. 1982;155:161-166.
Ogata Y, et al. Role of bile in intestinal barrier function and its inhibitory effect on bacterial translocation in obstructive jaundice in rats. J Surg Res. 2003;115:18-23.
Ohkubo M, et al. Surgical anatomy of the bile ducts at the hepatic hilus as applied to living donor liver transplantation. Ann Surg. 2004;239:82-86.
Okuda K, et al. Clinical aspects of intrahepatic bile duct carcinoma including hilar carcinoma: a study of 57 autopsy-proven cases. Cancer. 1977;39:232-246.
Okuda K, et al. The role of ultrasound, percutaneous transhepatic cholangiography, computed tomographic scanning, and magnetic resonance imaging in the preoperative assessment of bile duct cancer. World J Surg. 1988;12:18-26.
Ortner MA, et al. Photodynamic therapy of nonresectable cholangiocarcinoma. Gastroenterology. 1998;114:536-542.
Ortner ME, et al, 2003: Successful photodynamic therapy for nonresectable cholangiocarcinoma: a randomized prospective study. 125(5):1355-1363.
Ozden I. Clinicopathological study on the infraportal bile ducts of segment 3. World J Surg. 2002;26:1441-1445.
Parc Y, et al. Surgical strategy for the management of hilar bile duct cancer. Br J Surg. 1997;64(12):1575-1579.
Park JO, et al. A phase II trial of gemcitabine plus cisplatin (GP) in patients with inoperable biliary tract cancer (BTC). Proc Am Soc Clin Oncol. 2005;23(Pt 1):4133.
Patel T. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Hepatology. 2001;33:1353-1357.
Patt YZ, et al. Phase II trial of intravenous fluorouracil and subcutaneous interferon alfa-2b for biliary tract cancer. J Clin Oncol. 1996;14:2311-2315.
Pichlmayr R, et al. Surgical treatment in proximal bile duct cancer: a single-center experience. Ann Surg. 1996;224:628-638.
Pitt HA, et al. Does preoperative percutaneous biliary drainage reduce operative risk or increase hospital cost? Ann Surg. 1985;201:545-552.
Pitt HA, et al. Malignancies of the biliary tree. Curr Prob Surg. 1995;32:1-90.
Pitt HA, et al. Perihilar cholangiocarcinoma: postoperative radiotherapy does not improve survival. Ann Surg. 1995;221:788-798.
Polydorou AA, et al. Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut. 1992;32:685-689.
Quyn AJ, et al. Photodynamic therapy is associated with an improvement in survival for pateints with irresectable hilar cholangiocarcinoma. HPB. 2009;11(7):570-577.
Rabinovitz M, et al. Diagnostic value of brush cytology in the diagnosis of bile duct carcinoma: a study in 65 patients with bile duct strictures. Hepatology. 1990;12:747-752.
Rashid A. Cellular and molecular biology of biliary tract cancers. Surg Oncol Clin N Am. 2002;11:995-1009.
Rea DJ, et al. Liver transplantation with neoadjuvant chemoradiation is more effective than resection for hilar cholangiocarcinoma. Ann Surg. 2005;242:451-458.
Rerknimitr R, et al. Results of endoscopic biliary drainage in hilar cholangiocarcinoma. J Clinical Gastroenterol. 2004;38:518-523.
Robson P, et al. Prospective study of outcomes after percutaneous biliary drainage for malignant biliary obstruction. Ann Surg Oncol. 2010;17(9):2303-2311.
Rosen CB, et al. Cholangiocarcinoma complicating primary sclerosing cholangitis. Ann Surg. 1991;213(1):21-25.
Rossi P, et al. Metallic stents in malignant biliary obstruction: results of a multicenter European study of 240 patients. J Vasc Interv Radiol. 1994;5:279-285.
Rugge M, et al. Primary carcinoid tumor of the cystic and common bile ducts. Am J Surg Pathol. 1992;16:802-807.
Ryan ME. Cytologic brushings of ductal lesions during ERCP. Gastrointest Endosc. 1991;37:139-142.
Saiki S, et al. Preoperative internal drainage is superior to external biliary drainage in liver regeneration and function after hepatectomy in obstructive jaundiced rats. Ann Surg. 1999;230:655-662.
Sakaguchi S, Nakamura S. Surgery of the portal vein in resection of cancer of the hepatic hilus. Surgery. 1986;99:344-349.
Sakamoto E, et al. Case of bile duct carcinoma of the hepatic hilus with segmental obstructive cholangitis. Hepatogastroenterology. 1995;42:501-505.
Sakamoto E, et al. The pattern of infiltration at the proximal border of hilar bile duct carcinoma. Ann Surg. 1998;227:405-411.
Sako K, et al. Carcinoma of the extra-hepatic bile ducts: review of the literature and report of six cases. Surgery. 1957;41:416-437.
Saldinger PF, Blumgart LH. Resection of hilar cholangiocarcinoma: a European and United States experience. J Hepatobiliary Pancreat Surg. 2000;7:111-114.
Sankary HN, et al. Carcinoid tumors of the extrahepatic bile duct: an unusual cause of bile duct obstruction. Liver Transplant Surg. 1995;1:122-123.
Sano T, et al. One hundred two consecutive hepatobiliary resections for perihilar cholangiocarcinoma with zero mortality. Ann Surg. 2006;244(2):240-247.
Sanz-Altamira PM, et al. A phase II trial of irinotecan (CPT-11) for unresectable biliary tree carcinoma. Ann Oncol. 2001;12:501-504.
Schima W, et al. Biliary Wallstent endoprosthesis in malignant hilar obstruction: long-term results with regard to the type of obstruction. Clin Radiol. 1997;52:213-219.
Schwartz LH, et al. Neoplastic pancreaticobiliary duct obstruction: evaluation with breath-hold MR cholangiopancreatography. AJR Am J Roentgenol. 1998;170(6):1491-1495.
Seyama Y, et al. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 2003;238:73-83.
Shimada H, et al. The infiltration of bile duct carcinoma along the bile duct wall. Int Surg. 1988;73:87-90.
Speer AG, et al. Randomized trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet. 1987;2:57-62.
Stoker J, Lameris JS. Complications of percutaneously inserted biliary Wallstents. J Vasc Interv Radiol. 1993;4:767-772.
Suzuki H, et al. Internal biliary drainage, unlike external drainage, does not suppress the regeneration of cholestatic rat liver after partial hepatectomy. Hepatology. 1994;20:1318-1322.
Takada T, et al. Is postoperative adjuvant chemotherapy useful for gallbladder carcinoma? A phase III multicenter prospective randomized controlled trial in patients with resected pancreaticobiliary carcinoma. Cancer. 2002;95(8):1685-1695.
Tanaka K, et al. Biliary tract cancer accompanied by anomalous junction of pancreaticobiliary ductal system in adults. Am J Surg. 1998;175:218-220.
Tanaka M, et al. Long-term consequence of endosopic sphincterotomy for bile duct stones. Gastrointest Endosc. 1998;48:465-469.
Tompkins RK, et al. Prognostic factors in bile duct carcinoma: analysis of 96 cases. Ann Surg. 1981;194:447-457.
Tsao JI, et al, 2000: Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. 232(2):166-174.
Tsuzuki T, et al. Carcinoma of the bifurcation of the hepatic ducts. Arch Surg. 1983;118:1147-1151.
Valle J, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362:1273-1281.
Vallis KA, et al. External beam and intraluminal radiotherapy for locally advanced bile duct cancer: role and tolerability. Radiother Oncol. 1996;41:61-66.
van den Bosch RP, et al. Guidelines for the application of surgery and endoprostheses in the palliation of obstructive jaundice in advanced cancer of the pancreas. Ann Surg. 1994;219:18-24.
Vatanasapt V, et al. Cholangiocarcinoma in north-east Thailand (letter). Lancet. 1990;335:116-117.
Vatanasapt V, et al. A high incidence of liver cancer in Khon Kaen Province, Thailand. Southeast Asian J Trop Med Public Health. 1990;21:489-494.
Verbeek PC, et al. Benign fibrosing disease at the hepatic confluence mimicking Klatskin tumors. Surgery. 1992;112:866-871.
Vogt DP. Current management of cholangiocarcinoma. Oncology. 1954;2:37-44.
Vollmer CM, et al. Utility of staging laparoscopy in subsets of peripancreatic and biliary malignancies. Ann Surg. 2002;235:1-7.
Voyles CR, Blumgart LH. A technique for the construction of high biliary-enteric anastomoses. Surg Gynecol Obstet. 1982;154:885-887.
Voyles CR, et al. Carcinoma of the proximal extrahepatic biliary tree: radiologic assessment and therapeutic alternatives. Ann Surg. 1983;197:188-194.
Wade TP, et al. Experience with distal bile duct cancers in U.S. Veterans Affairs hospitals: 1987-1991. J Surg Oncol. 1997;64:242-245.
Watanapa P. Cholangiocarcinoma in patients with opisthorchiasis. Br J Surg. 1996;83:1062-1064.
Way LW. Biliary tract. In: Way, LW, editor. Current Surgical Diagnosis and Treatment. 10th ed. Norwalk, CT: Appleton & Lange; 1994:537-566.
Weber A, et al. Long-term outcomes and prognostic factors of patients with hilar cholangiocarcinoma. World J Gastroenterol. 2007;13:1422-1426.
Weber SM, et al. Staging laparoscopy in patients with extrahepatic biliary carcinoma: analysis of 100 patients. Ann Surg. 2002;235:392-399.
Weinbren K, Mutum SS. Pathological aspects of cholangiocarcinoma. J Pathol. 1983;139:217-238.
Wetter LA, et al. Differential diagnosis of sclerosing cholangiocarcinomas of the common hepatic duct (Klatskin tumors). Am J Surg. 1991;161:57-63.
Williamson BW, et al. Management of tumors of the liver: combined use of arteriography and venography in the assessment of resectability especially in hilar tumours. Am J Surg. 1980;139:210-215.
Winslet MC, et al. Diffuse increase in renal uptake of technetium 99m methylene diphosphonate in association with disseminated cholangiocarcinoma. Eur J Nucl Med. 1990;17:372-373.
Wolber RA, et al. Polyclonal carcinoembryonic antigen staining in the cytologic differential diagnosis of primary and metastatic hepatic malignancies. Acta Cytol. 1991;35:215-220.
Yeo CJ, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg. 1997;226:248-257.
Zoepf T, et al. Palliation of nonresectable bile duct cancer: improved survival after photodynamic therapy. Am J Gastroenterol. 2005;100:2426-2430.