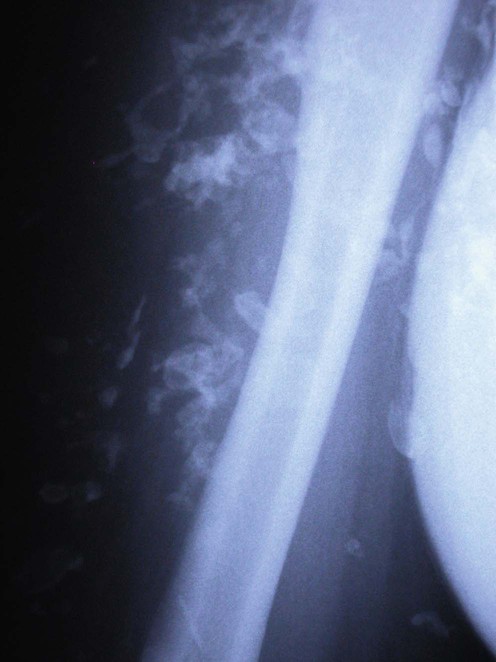
Calcinosis cutis
 Idiopathic: occurs without tissue injury or metabolic defect (e.g., idiopathic scrotal calcinosis).
Idiopathic: occurs without tissue injury or metabolic defect (e.g., idiopathic scrotal calcinosis).
 Dystrophic: secondary to local tissue damage or alterations in collagen, elastin or subcutaneous fat but normal calcium and phosphate levels (e.g., in connective tissue diseases, post trauma or infection).
Dystrophic: secondary to local tissue damage or alterations in collagen, elastin or subcutaneous fat but normal calcium and phosphate levels (e.g., in connective tissue diseases, post trauma or infection).
 Metastatic: abnormal calcium and/or phosphate metabolism leading to precipitation of calcium salts in normal tissue.
Metastatic: abnormal calcium and/or phosphate metabolism leading to precipitation of calcium salts in normal tissue.
 Iatrogenic: secondary to a treatment or procedure (such as extravasation of calcium or phosphate infusions).
Iatrogenic: secondary to a treatment or procedure (such as extravasation of calcium or phosphate infusions).
First-line therapies
Second-line therapies
Third-line therapies












 No treatment/self-healing
No treatment/self-healing Aluminum hydroxide
Aluminum hydroxide Intralesional corticosteroid
Intralesional corticosteroid Diltiazem
Diltiazem Bisphosphonates
Bisphosphonates Probenecid
Probenecid Colchicine
Colchicine Minocycline
Minocycline Warfarin
Warfarin Ceftriaxone
Ceftriaxone Rituximab
Rituximab Intravenous immunoglobulin
Intravenous immunoglobulin Intravenous Sodium thiosulphate
Intravenous Sodium thiosulphate Topical sodium thiosulphate
Topical sodium thiosulphate Surgery
Surgery Carbon dioxide laser
Carbon dioxide laser Extracorporeal shock wave lithotripsy
Extracorporeal shock wave lithotripsy