Chapter 410 Bronchopulmonary Dysplasia
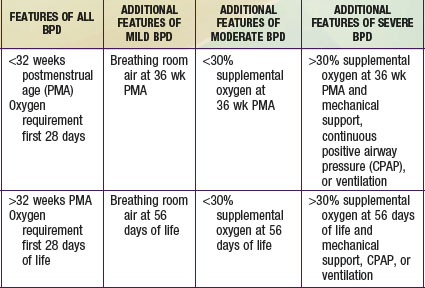
Bronchopulmonary dysplasia (BPD) is a syndrome characterized by signs and symptoms of chronic lung disease that originates in the neonatal period (Chapter 95). The pathogenesis of the lung disease was originally thought to arise from mechanical and oxidant injury to the airways and interstitium leading to edema, inflammation, and fibrosis with characteristic radiographic and pathologic stages. The pathogenesis of lung disease in the population of neonates <1000 g also includes the contribution of immature development of airway and vascular structures of the lung. This fact has led to a change in recognized radiographic, pathologic, and clinical findings in BPD and an evolution in its definition. An accepted definition includes an oxygen requirement for 28 days postnatally, and the disorder is graded as mild, moderate or severe on the basis of supplemental oxygen requirement and gestational age (see Table 410-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com ![]() ).
).
Clinical Manifestations
Gastroesophageal reflux disease (GERD) (Chapter 315) and pulmonary aspiration complicate pulmonary status, particularly during an exacerbation when the infant is most tachypneic and when pulmonary mechanics increase the risk of GERD. Other conditions due to premature birth complicating BPD include upper airway obstruction leading to hypoxia, neurodevelopmental delay with increased risk of aspiration, systemic hypertension with left ventricular hypertrophy, poor growth, and electrolyte disturbances.
American Thoracic Society. Statement on the care of the child with chronic lung disease of infancy and childhood. Am J Respir Crit Care Med. 2003;168:356-396.
Baraldi E, Filippone M. Chronic lung disease after premature birth. N Engl J Med. 2007;357:1946-1955.
Bott L, Beghin L, Devos P, et al. Nutritional status at 2 years in former infants with bronchopulmonary dysplasia influences nutrition and pulmonary outcomes during childhood. Pediatr Res. 2006;60:340-344.
Jobe AJ. The new BPD: an arrest of lung development. Pediatr Res. 1999;46:641-643.
Kinsella JP, Greenough A, Abman SH. Bronchopulmonary dysplasia. Lancet. 2006;367:1421-1430.
Stocks J, Coates A, Bush A. Lung function in infants and young children with chronic lung disease of infancy: the next steps? Pediatr Pulmonol. 2007;42:3-9.