Bronchodilators
β-adrenergic receptor agonists
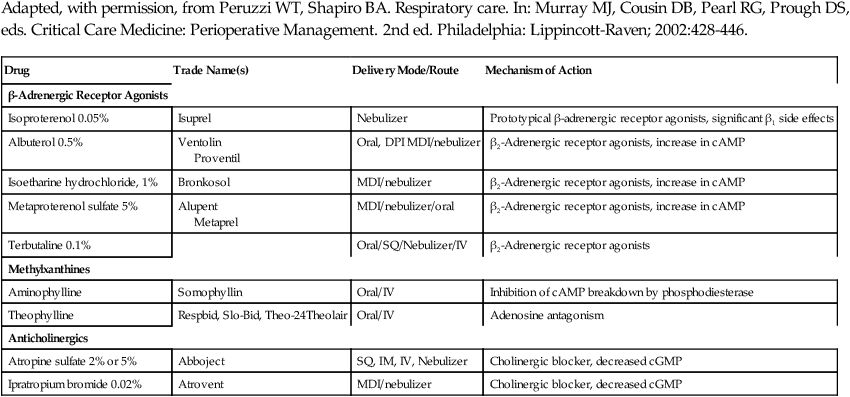
Selective β2-receptor agonists relax bronchioles and uterine smooth muscle without affecting the heart via β1-receptor stimulation. These drugs activate adenyl cyclase, which converts adenosine triphosphate (ATP) to cyclic adenosine 3´-5´-monophosphate (cAMP), which in turn causes relaxation of smooth muscle, resulting in bronchodilation. Nonselective β-receptor agonists used for bronchodilation include epinephrine, isoproterenol, and isoetharine. Selective β2-receptor agonists include albuterol, terbutaline, metaproterenol, and others (Table 94-1). Side effects associated with the use of nonselective medications include increased heart rate, contractility, and myocardial O2 consumption. Selective β2-receptor agonists may also produce some cardiac effects, especially if administered subcutaneously or intravenously. Hypokalemia and hyperglycemia may also occur. Chronic use can be associated with tachyphylaxis.
Table 94-1
| Drug | Trade Name(s) | Delivery Mode/Route | Mechanism of Action |
| β-Adrenergic Receptor Agonists | |||
| Isoproterenol 0.05% | Isuprel | Nebulizer | Prototypical β-adrenergic receptor agonists, significant β1 side effects |
| Albuterol 0.5% | Ventolin Proventil |
Oral, DPI MDI/nebulizer | β2-Adrenergic receptor agonists, increase in cAMP |
| Isoetharine hydrochloride, 1% | Bronkosol | MDI/nebulizer | β2-Adrenergic receptor agonists, increase in cAMP |
| Metaproterenol sulfate 5% | Alupent Metaprel |
MDI/nebulizer/oral | β2-Adrenergic receptor agonists, increase in cAMP |
| Terbutaline 0.1% | Oral/SQ/Nebulizer/IV | β2-Adrenergic receptor agonists | |
| Methylxanthines | |||
| Aminophylline | Somophyllin | Oral/IV | Inhibition of cAMP breakdown by phosphodiesterase |
| Theophylline | Respbid, Slo-Bid, Theo-24Theolair | Oral/IV | Adenosine antagonism |
| Anticholinergics | |||
| Atropine sulfate 2% or 5% | Abboject | SQ, IM, IV, Nebulizer | Cholinergic blocker, decreased cGMP |
| Ipratropium bromide 0.02% | Atrovent | MDI/nebulizer | Cholinergic blocker, decreased cGMP |