23 Borderline Personality Disorder
Clinical Presentation
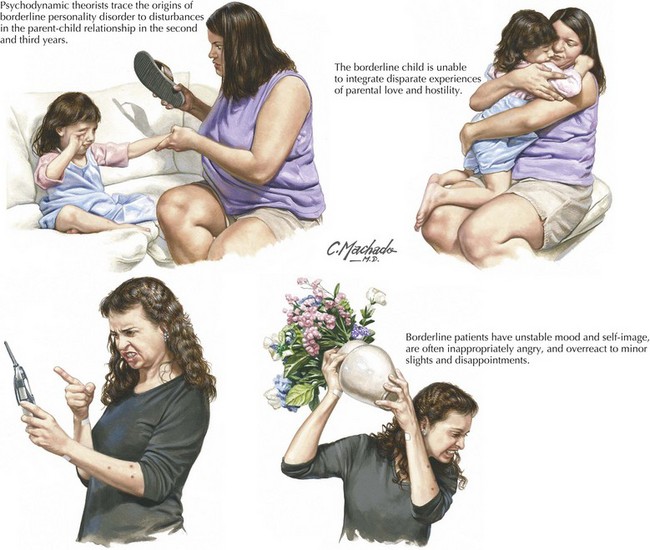
In the 1950s, one subtype of borderline patient was isolated. These individuals had a persistent odd or flat affect, mild but stable thought disorder, and a family history of schizophrenia. Such patients suffer from a forme fruste of schizophrenia, and are now diagnosed with schizotypal personality disorder. The remaining borderline patients, those with DSM borderline personality disorder, are described as “the stably unstable.” They have rapid and overwhelming mood fluctuations, are often strikingly angry, and react disastrously to minor slights and disappointments (Fig. 23-1). Their interpersonal relations are intense and stormy. They fail to establish consistent vocational identities, frequently abuse drugs, injure themselves, and are liable to brief psychotic episodes when stressed.
Abraham PF, Calabrese JR. Evidence-based pharmacologic treatment of borderline personality disorder: A shift from SSRIs to anticonvulsants and atypical antipsychotics? J Affect Disord. 2008 Feb 25.
Gunderson JG, Hoffman PD, editors. Understanding and Treating Borderline Personality Disorder: A Guide for Professional and Families. Washington, D.C: American Psychiatric Association Press, 2005.
Linehan M. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, NY: Guilford; 1993.