Body dysmorphic disease (dermatologic nondisease)
Synonyms: body dysmorphic disorder, dysmorphophobia (not good as the condition is not a ‘phobia’), dermatological nondisease (not good as it is not particularly accurate)
Management strategy
Body areas on which patients with BDD may focus:
 Face: preoccupation with facial wrinkles, pigmentation, oiliness, redness, paleness, facial vessels, and facial hair are common. Preoccupation with the nose, ears, and pore size is reported. Despite the fact that others usually do not see these minimal or nonexistent flaws, patients can spend hours in front of mirrors, preventing them from working or socializing
Face: preoccupation with facial wrinkles, pigmentation, oiliness, redness, paleness, facial vessels, and facial hair are common. Preoccupation with the nose, ears, and pore size is reported. Despite the fact that others usually do not see these minimal or nonexistent flaws, patients can spend hours in front of mirrors, preventing them from working or socializing
 Scalp: BDDs with real or imagined hair loss are common
Scalp: BDDs with real or imagined hair loss are common
 Genital: genital size, shape and appearance may be a focus of patients with BDD. Some patients complain of persistent genital burning, itching and pain. Preoccupation with sexually transmitted disease or neoplastic process is common.
Genital: genital size, shape and appearance may be a focus of patients with BDD. Some patients complain of persistent genital burning, itching and pain. Preoccupation with sexually transmitted disease or neoplastic process is common.
Specific investigations
A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice.
Dufresne Jr RG, Phillips KA, Vittorio CC, Wilkel CS. Dermatol Surg 2001; 27:457–62.
The Body Dysmorphic Disorder questionnaire is an alternative screening tool for BDD.
It is important to have a series of screening questions to ascertain if BDD is an issue for patients (Table 30.1).
Table 30.1
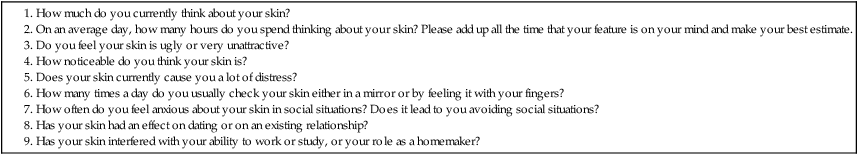
(Adapted from Veale D, Ellison N, Werner TG, et al. Development of a cosmetic procedure screening questionnaire (COPSs) for body dysmorphic disorder. J Plast Reconstr Aesthet Surg 2012;65(4): 530–532.)








 Treatment of the skin
Treatment of the skin Selective serotonin reuptake inhibitors
Selective serotonin reuptake inhibitors Cognitive behavioral therapy
Cognitive behavioral therapy Antipsychotic drugs
Antipsychotic drugs