Board certification and maintenance of certification
Primary certification
Physicians who successfully complete the requirements for residency training (the Continuum of Education) in an Accreditation Council for Graduate Medical Education (ACGME)-accredited anesthesiology residency program may qualify to enter the examination process for primary certification by the ABA if they meet the threshold requirements for primary certification in anesthesiology (Box 248-1).
Subspecialty certification
The ABA also offers subspecialty certification in critical care medicine, pain medicine, hospice and palliative care medicine, sleep medicine, and pediatric anesthesiology (Box 248-2). Subspecialty recertification is offered through successful completion of a written examination. A transition from subspecialty recertification examination programs to Maintenance of Certification in Anesthesiology for Subspecialties (MOCA-SUBS) began January 1, 2010. The last subspecialty recertification examinations will be conducted in 2016 and the first MOCA-SUBS examinations will be conducted in 2017. The MOCA-SUBS program is the only option for holders of ABA subspecialty certification or recertification awarded after January 1, 2010. After 2016, the MOCA-SUBS program is the only option to maintain subspecialty certification.
Maintenance of certification
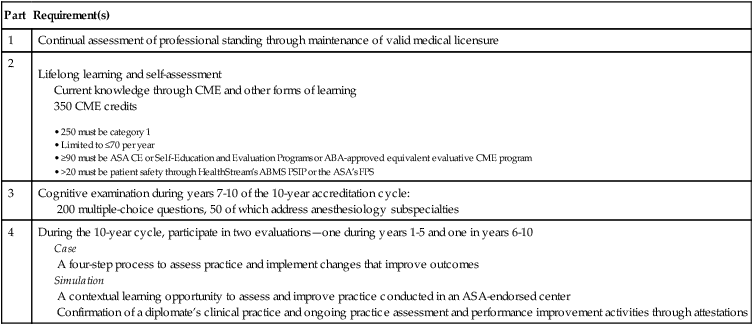
Maintenance of Certification in Anesthesiology (MOCA) is required for ongoing certification of anesthesiologists who achieved primary certification in anesthesiology during or after 2000. The MOCA process is completed in 10-year cycles intended to assure the public of a diplomate’s continuing competence in the practice of anesthesiology. MOCA requirements are divided into four parts: professional standing, lifelong learning and self-assessment, cognitive examination, and practice performance assessment and improvement. MOCA requirements are summarized in Table 248-1.
Table 248-1
Maintenance of Certification in Anesthesiology Requirements
| Part | Requirement(s) |
| 1 | Continual assessment of professional standing through maintenance of valid medical licensure |
| 2 |
Lifelong learning and self-assessment |
200 multiple-choice questions, 50 of which address anesthesiology subspecialties
Case
A four-step process to assess practice and implement changes that improve outcomes
Simulation
A contextual learning opportunity to assess and improve practice conducted in an ASA-endorsed center
Confirmation of a diplomate’s clinical practice and ongoing practice assessment and performance improvement activities through attestations