Chapter 9. Blood Pressure
Blood pressure readings provide significant information about the child’s health status. Until recently, children younger than 3 years were commonly not screened for blood pressure because of the extra skill and patience required to obtain a blood pressure reading in such young patients. Most children with hypertension have renal disease; many fewer have coarctation of the aorta or pheochromocytoma. Screening of blood pressure in young children permits early detection of serious disorders and should be performed at least yearly on children from 3 years of age to adolescence. Blood pressure determination is routine on admission to health care facilities and in postoperative procedures. It should also be performed after invasive diagnostic procedures and before and after administration of drugs known to alter blood pressure. Blood pressure is taken whenever a child “feels funny” or when a child’s condition deteriorates.
Anatomy and Physiology
Blood pressure is a product of cardiac output and increased peripheral resistance. In the neonate, systolic blood pressure is low, reflecting the weaker ability of the left ventricle. As the child grows, the size of the heart and of the left ventricle also increases, resulting in steadily increasing blood pressure values. At adolescence the heart enlarges abruptly, which also results in an increase in blood pressure values, comparable to those of the adult (Table 9-1).
| *Values that fall at or below the lower number in each range are considered normotensive. Values that fall above the higher number in each range might be indicative of hypertension. |
||||
| Age | Girls Systole (mmHg) | Girls Diastole (mmHg) | Boys Systole (mmHg) | Boys Diastole (mmHg) |
|---|---|---|---|---|
| 1 yr | 97–107 | 53–60 | 94–106 | 50–59 |
| 3 yr | 100–110 | 61–68 | 100–113 | 59–67 |
| 6 yr | 104–114 | 67–75 | 105–117 | 67–76 |
| 8 yr | 108–118 | 70–78 | 107–120 | 71–80 |
| 10 yr | 112–122 | 73–80 | 110–123 | 73–82 |
| 12 yr | 116–126 | 75–82 | 115–127 | 75–83 |
| 14 yr | 119–130 | 77–85 | 120–132 | 76–84 |
| 16 yr | 122–132 | 79–86 | 125–138 | 79–87 |
An increase in cardiac output or in peripheral resistance will raise blood pressure. Decrease in cardiac output or in peripheral resistance will lower blood pressure. Overall maintenance of blood pressure reflects an intimate relationship among cardiac output, peripheral resistance, and blood volume, which can be influenced by several other factors (Table 9-2).
| Influence | Effect |
|---|---|
| Medications |
Narcotic analgesics, general anesthetics, diuretics decrease blood pressure.
Aminophylline increases blood pressure.
|
| Conditions |
Blood pressure decreases during hemorrhage.
Blood pressure increases with renal disease, increased intracranial pressure, coarctation of aorta (blood pressure in arms), pheochromocytoma, hyperthyroidism, diabetes mellitus, and acute pain.
Pulse pressure widens with increased intracranial pressure.
|
| Diurnal variation | Blood pressure usually is higher during morning and afternoon than during evening and night. |
| Apprehension and anxiety | Increases blood pressure. |
| Increased activity | Increases blood pressure. |
Equipment for Measuring Blood Pressure
▪ Pediatric stethoscope
▪ Sphygmomanometer with either a mercury or an aneroid manometer or electronic blood pressure devices (oscillometer, Doppler ultrasound)
▪ Ace or tensor bandage (flush technique)
Preparation
Ask the parent or child about family history of hypertension or cardiac or kidney disease. Ask if the child has or has had headaches, nosebleeds, swelling, alterations in voiding patterns, or clotting disorder or whether the child is on anticoagulant therapy.
▪ Select appropriate method. Palpation rather than auscultation can be performed if the child has a narrow or deep brachial artery. The flush technique can be selected if it is impossible to obtain blood pressure readings in young children or infants by other means. Oscillometric devices yield readings that correlate better with direct radial artery values than methods using auscultation and avoid problems associated with auscultation such as too rapid deflation of the cuff. Doppler ultrasound is accurate for systolic blood pressure but unreliable for diastolic pressure measurement. Limbs must be stabilized during measurement with oscillometric devices if accurate readings are to be obtained. Electronic or automatic cuffs must be used cautiously if the child is receiving anticoagulant therapy and has a disorder that affects clotting. The maximal inflation pressure on the automatic blood pressure machine should be adjusted to the child’s last systolic blood pressure. Once the child’s blood pressure is stable, the intervals between measurement should be increased to avoid too frequent inflation of the cuff.
▪ Select appropriate site (Figure 9-1). Extremities in casts, those in which intravenous fluids are being infused, or those that are traumatized should not be used. Thighs can be selected if only large cuffs are available.
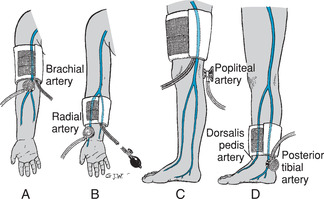 |
| Figure 9-1Sites for blood pressure measurement. A, Upper arm. B, Lower arm or forearm. C, Thigh. D, Calf or ankle.(From Hockenberry MJ et al: Wong’s nursing care of infants and children, ed 7, St Louis, 2003, Mosby.)Elsevier Inc. |
▪ Select appropriate cuff size. The cuff should cover at least 75% of the upper arm or thigh in children and adolescents (Table 9-3), leaving enough room to place the bell of the stethoscope at the antecubital fossa and to avoid obstruction of the axilla. An overly large cuff might produce low readings. A cuff that is too narrow might produce high readings. If a correctly fitting cuff is not available, a wider cuff can be used. (Wider cuffs do not create the low readings in infants and young children that are produced in adults.) The cuff bladder should be long enough to encircle the arm without overlapping. In children who are overweight or who have thick arms, measuring limb circumference can be a more accurate method for determining cuff size. When considering limb circumference, the cuff should be 40% to 50% of the limb circumference when measuring at the upper arm, midway between the top of the shoulder and the olecranon. Limb circumference guidelines should be used when using an area other than the upper arms for blood pressure measurement.
| Age | Bladder Width (cm) | Bladder Length (cm) |
|---|---|---|
| Infant | 5 | 8 |
| Child | 8 | 13 |
| Adult | 13 | 24 |
▪ Check needle of aneroid manometer. It should be at zero.
▪ Check mercury column of mercury-gravity manometer. It should be at zero.
▪ Blood pressure readings should be performed before other anxiety-producing procedures. The infant or child should be sitting quietly or lying down. The very young child might be most comfortable cradled in the parent’s arms or lap.
| Assessment | Findings |
|---|---|
| Select appropriate site and cuff. Position the child’s limb. The arm should be at heart level. If positioned below the heart, falsely high reading might be obtained. If obtaining a thigh reading, the child can be positioned on the abdomen or with the knee slightly flexed. Expose the limb completely. Compression of the limb by rolled-up clothing can give a low reading. If the child is upset by removal of clothing, it is best to apply the cuff over the sleeve rather than rolling it up. Rolling produces a tight band. | |
| Palpate the brachial artery if using the arm, or the popliteal artery if using the thigh. Ensure that the cuff is fully deflated. Center the arrows on the cuff over the brachial artery of the arm, or position the bladder over the posterior aspect of the thigh. Position the manometer at eye level. | Viewing the manometer from above or below gives inaccurate readings. |
| Palpate the radial or popliteal artery, and inflate the cuff to 20 mmHg above the point at which the pulse disappears. | |
| Deflate the cuff; wait 15 to 30 seconds. | Inadequate release of venous congestion gives falsely high readings. |
| Assessment | Findings |
|---|---|
| Place the earpieces of the stethoscope in your ears. Earpieces should point forward to be inserted correctly. A pediatric stethoscope and bell should be used for infants and small children. | Incorrect placement of earpieces produces muffling or no sound at all. |
| Relocate the brachial or the popliteal artery. Place the bell or the diaphragm over the artery. Turn the valve of the pressure bulb clockwise until tight, and inflate cuff to 20 mmHg above the child’s systolic reading. | Improper placement of the stethoscope produces low systolic and high diastolic readings. |
| Gradually release the valve to reduce pressure at a rate of 2 to 3 mmHg/sec. | Rapid release can cause inaccurate reading of the systolic pressure. |
| Observe the point at which the first clear reading (first Korotkoff sound) is obtained (systolic pressure) and at which the first muffling occurs (fourth Korotkoff sound) for the diastolic pressure in children younger than 13 years. Record the point at which all sound disappears (fifth Korotkoff sound) as the diastolic pressure in children 13 years and older. |
In children younger than 1 year, thigh pressures should equal arm pressures; in children older than 1 year, thigh pressure is approximately 20 mmHg higher.
Blood pressure will tend to be higher in children who are large for age than in children who are small.
Korotkoff sounds might not be audible in early childhood because of a narrow or deeply placed artery.
Clinical Alert
A thigh pressure reading that is the same or lower than upper arm readings in infants might indicate coarctation of the aorta.
|
| Assessment | Findings |
|---|---|
| Deflate the cuff rapidly after readings have been obtained. Wait 30 seconds before obtaining further readings. |
Clinical Alert
Repeat blood pressure readings if lower or higher than expected.
|
| Record limb, position, cuff size, and how reading was obtained. |
Document and report persistently elevated or lowered blood pressure readings. Consistently elevated serial readings can indicate hypertension. Persistently low diastolic pressure can indicate a patent ductus arteriosus.
Pulse pressure (difference between systolic and diastolic pressures) of more than 50 mmHg can indicate congestive heart failure. Pulse pressure of less than 10 mmHg can indicate aortic stenosis.
|
| Assessment | Findings |
|---|---|
|
Select appropriate site and cuff. Position child’s limb, and prepare the cuff as though determining blood pressure by auscultation method.
Palpate the brachial or the radial artery (arm) or the popliteal artery (thigh), and inflate the cuff 20 mmHg above point at which pulse disappears.
Slowly deflate the cuff, at a rate of 2 to 3 mmHg/sec.
|
|
| Determine point at which the pulse is first felt. This is the systolic pressure. The diastolic pressure cannot be determined by this method. | The systolic pressure obtained by radial palpation is approximately 10 mmHg lower than arm pressure. |
| Assessment | Findings |
|---|---|
| Wrap cuff around the limb. Elevate the limb. Wrap an elastic bandage from the fingers toward the antecubital space (or from the toes toward the knee). | |
| Inflate the cuff above the expected systolic pressure. Remove bandage. Place the child’s arm at his or her side. | The limb will appear pale. |
| Slowly deflate the cuff until color suddenly returns. The reading is taken when color appears. | The value (flush pressure) obtained is the mean blood pressure (average of the diastolic and systolic pressures). |
Related Nursing Diagnoses
Decreased cardiac output: related to arrhythmias, congenital anomalies, medications.
Fluid volume deficit: related to active volume loss.
Fluid volume excess: related to excess fluid intake.
Altered tissue perfusion, cardiopulmonary and peripheral: related to hypovolemia, interrupted arterial or venous blood flow, blood pressure changes in extremities.