CHAPTER 29 BLADDER AND SEXUAL FUNCTION AND DYSFUNCTION
The autonomic nervous system is sometimes perceived by neurologists as a somewhat mysterious, even miasmic, component of the nervous system. Consequently, when autonomic dysfunction accompanies a neurological disease process, neurologists often are reluctant to discuss the autonomic symptoms with their patients or to initiate specific evaluation or treatment, preferring to cede this to specialists in other disciplines such as cardiology, gastroenterology, and urology. However, autonomic dysfunction is an integral component of a number of neurological disease processes routinely managed by neurologists, and if attention to and assessment of autonomic dysfunction are inadequate, treatment of the disease and management of the patient may be inadequate. In this chapter, bladder and sexual dysfunction are addressed with the intent of providing practical information for the practicing neurologist.
BLADDER FUNCTION
Neuroanatomy and Neurophysiology
Cortex
There is a tendency to focus on the spinal cord and sacral nerves when bladder function is assessed, but cortical and brainstem centers play active and very important roles in the control of bladder function.1,2 Early information regarding cerebral control of voiding was collected in studies of individuals with structural brain lesions.3–5 These studies demonstrated that lesions in the anterior frontal lobe may produce disturbances in bladder control. Affected individuals were noted to experience severe, precipitous urgency without prior sensation of bladder fullness, but coordination of detrusor and sphincter muscle function during micturition remained normal. Studies of individuals after stroke have also implicated the anteromedial frontal lobe and its descending pathway, along with the basal ganglia in the production of urinary dysfunction.6 More recent elegant neuroimaging studies with single photon emission computed tomography (SPECT), positron emission tomography, and functional magnetic resonance imaging have revealed a more detailed pattern of a complex array of cortical centers involved with voluntary regulation and control of bladder function, including not only frontal cortex but also the cingulate cortex, parietal cortex, basal ganglia, hypothalamus, and even the cerebellum.2,7
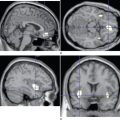
Brainstem
Direct motor control of bladder function resides in the pons. The pontine micturition center, identified by Barrington in 19258,9 and now bearing his name, lies in the medial dorsal pons. Stimulation of this nucleus has the dual effect of producing both contraction of the detrusor muscle and relaxation of the urethral sphincter, the latter via inhibition of Onuf’s nucleus in the sacral spinal cord, with consequent micturition.10 A second, more lateral pontine region appears to tonically stimulate Onuf’s nucleus and to thus prevent micturition by inhibiting detrusor contraction and urethral relaxation.11 Sensory information regarding the state of bladder filling does not appear to come directly to these two pontine centers; rather, its path is coordinated through neurons in the periaqueductal grey matter in the mesencephalon.2,12
Spinal Cord and Peripheral Nerves
Control of bladder function at the spinal cord level is dependent on both autonomic and somatic mechanisms. Parasympathetic signals reach the bladder detrusor smooth muscle via pelvic nerves that originate in the intermediolateral column of the sacral cord at the S2-S4 levels, whereas sympathetic input arises from T11-L2 spinal cord levels and arrives at the smooth muscle of the bladder neck and urethra through the hypogastric nerves. The striated muscle of the urethral sphincter is innervated by a specialized group of anterior horn cells at the S2-S4 cord levels, first described by Onufrowicz in 1899 and now called Onuf’s nucleus.13 Their axons travel in the pudendal nerves to reach the sphincter.
Parasympathetic stimulation results in contraction of the detrusor muscle (mediated by acetylcholine) and relaxation of urethral smooth muscle (mediated by nitric oxide) with the net result of micturition.14,15 Sympathetic stimulation has the opposite effect. Stimulation of Onuf’s nucleus produces contraction of the striated urethral sphincter.16
Sensory information from the bladder is transmitted by several different types of neurons.16,17 Small, unmyelinated, mechanosensitive Aδ fibers have a low activation threshold and are the principal conduit for transmitting information regarding the degree of bladder filling. Nociceptive, unmyelinated C fibers respond primarily to noxious stimuli rather than bladder distension. Finally, somatic afferents from the urethra transmit information regarding imminence of micturition.
BLADDER DYSFUNCTION
A normally functioning bladder can expand to hold 400 to 500 mL of urine before detrusor contraction is triggered and bladder pressure increases, producing a sense of the need to void.14 Damage to the nervous system can produce three basic patterns of neurogenic bladder dysfunction, described in Table 29-1.
As already noted, lesions affecting cerebral centers, both cortical and subcortical, may remove inhibitory influences on bladder function with consequent development of detrusor contractions at bladder volumes smaller than normal but without disturbing the coordinated contraction and relaxation of the detrusor and sphincter muscles. This has been labeled detrusor hyperreflexia, or neurogenic detrusor overactivity,18 and may prompt urinary frequency, often accompanied by a sense of urgency, that can lead to incontinence.
Diagnostic Tests
Although diagnostic testing of bladder function is usually performed by a urologist, it is important for neurologists to be familiar with the types of testing employed and the significance of the findings. Therefore, several of the most frequently used tests are discussed briefly as follows (Table 29-2).
Urodynamic Testing
Urodynamic testing actually entails a battery of tests, the exact complement of which can vary from urologist to urologist. Uroflowmetry is a screening study in which the patient urinates into a receptacle that measures the rate at which urine is voided. A urine flow curve is generated, and a variety of measurements, including mean and maximum flow rates, can be calculated. The normal flow curve has an unbroken bell shape, whereas obstructive lesions produce flattening and elongation of the curve. The flow curve in individuals with detrusor-sphincter dyssynergia is characterized by intermittent, discontinuous flow.19
Electromyography
Electromyography of the pelvic floor can be performed with either surface or needle electrodes. Surface electrodes are less invasive but record lower amplitude signals and are more prone to artifacts.20 The normal electromyographic sphincter pattern consists of continuous activity that ceases before detrusor contraction initiates micturition. Failure of this coordinated sphincter relaxation and detrusor contraction to occur is what constitutes detrusor-sphincter dyssynergia.
Concentric needle electromyography of the urethral sphincter can also demonstrate a pattern of denervation and reinnervation. Evidence of this can be seen in structural lesions of the cauda equina and in degenerative processes that involve Onuf’s nucleus, such as multiple-system atrophy (MSA). Additional, more detailed, clinical neurophysiological testing can also be performed at specialized centers.20
Specific Neurological Diseases
Stroke
Bladder dysfunction after stroke is frequently described, although specific data about incidence are difficult to pinpoint.21 In a review of the topic of stroke and incontinence, Brittain and colleagues22 noted that in various studies, incontinence on hospital admission had been described in 32% to 79% of stroke patients and was still present in 25% to 28% at the time of discharge. Problems with incontinence persisted in 12% to 19% even months after discharge.
The pattern of urinary difficulty differs between patients with hemispheric stroke and those with lesions in the brainstem. In individuals with hemispheric stroke, Sakakibara and colleagues6 documented nocturnal urinary frequency in 36%, urge incontinence in 29%, and difficulty voiding in 25%. Urinary symptoms were more frequent in persons with frontal lobe infarcts. Urodynamic testing in symptomatic patients demonstrated detrusor hyperreflexia in 68%, detrusor-sphincter dyssynergia in 14%, and uninhibited sphincter relaxation in 36%.
In a different group of patients after acute brainstem stroke, urodynamic studies showed detrusor hyperreflexia in 73%, low compliance bladder in 9%, atonic bladder in 27%, detrusor-sphincter dyssynergia in 45%, and uninhibited sphincter relaxation in 27%.23 Lesions producing bladder dysfunction involved either the dorsolateral or medial pons.
Thus, as expected, patients with stroke, whether hemispheric or brainstem, experience predominantly overactive or irritable bladder symptoms, although obstructive symptoms, including urinary retention, may also develop.23,24 Large infarct size, aphasia, cognitive impairment, and functional disability are associated with increased risk of urinary incontinence after stroke.25 Multiple infarcts, especially if bilateral, also predispose to urinary abnormalities after stroke.26 Because of the variability in urinary dysfunction that may appear after a stroke, urodynamic testing is invaluable in documenting the specific nature of the dysfunction. Specific treatment can then be tailored to the documented deficit.
Parkinson’s Disease
Urinary symptoms are a frequent source of difficulty for individuals with Parkinson’s disease. Reported frequencies of urinary dysfunction in Parkinson’s disease show considerable variability, ranging from 36% to 90%.27–30 Hobson and colleagues,29 comparing a community-based sample of patients with Parkinson’s disease with a similar-aged healthy elderly control group, discovered that the relative risk for bladder symptoms in the group with Parkinson’s disease was more than twice that of the control group. Some27,28,31–33 but not all29 studies have found a correlation between disease duration and severity and the presence of urinary symptoms. Irritative symptoms, such as frequency, urgency, and nocturia, are most common,27,28,30,34,35 but obstructive symptoms may also be reported.
The most frequent finding on urodynamic testing in individuals with Parkinson’s disease is detrusor hyperreflexia. Studies have revealed detrusor hyperreflexia to be present in 45% to 100% of urologically symptomatic patients with Parkinson’s disease.33–36 It is important to remember, however, that obstructive uropathies, such as prostatic hypertrophy, can be superimposed on detrusor hyperreflexia. In these instances, urodynamic testing can be especially helpful.
Urethral sphincter dysfunction may also develop in patients with Parkinson’s disease. Delayed relaxation of the sphincter on initiation of voiding, termed sphincter bradykinesia, has been reported in 11% to 42% of such patients.32,35,37 This phenomenon may create an obstructive pattern, characterized by a reduced flow rate. Inability to relax the perineal muscles on initiation of micturition has also been identified in the setting of Parkinson’s disease.38
The role of dopaminergic mechanisms in the production of urinary dysfunction in Parkinson’s disease has been the focus of research interest. In rats with unilateral 6-hydroxydopamine–induced lesions of the nigrostriatal pathway, bladder capacity was documented to be reduced and could be increased with administration of the dopamine D1/D5 receptor agonist SKF38393.39 In contrast, a D2/D3/D4 receptor agonist, quinpirole, reduced bladder capacity. In monkeys rendered parkinsonian by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) injection, the same pattern was evident in that the D2 agonist bromocriptine excited the micturition reflex, whereas the mixed D1/D2 agonist pergolide inhibited the reflex.40 Improvement in urinary symptoms has also been reported in humans whose treatment switched from bromocriptine to pergolide.41
Multiple-System Atrophy
Autonomic dysfunction is one of the basic clinical features of MSA. Orthostatic hypotension and genitourinary dysfunction are especially likely to develop. In contrast to Parkinson’s disease, urinary dysfunction in MSA tends to develop earlier in the course of the disease process, sometimes appearing even before the motor features31,42; it is also more pervasively present. In a study by Stocchi and colleagues,38 100% of patients with MSA demonstrated some abnormality on urodynamic testing, whereas abnormalities were noted in only 63% of subjects with Parkinson’s disease.
Urodynamic studies can be very useful in characterizing the nature of bladder dysfunction in MSA.43 A combination of detrusor hyperreflexia and impaired urethral sphincter function often produces a pattern of prominent urinary frequency and urgency, often accompanied by urge incontinence. Although this can also occur in Parkinson’s disease, it is typically a feature of only advanced Parkinson’s disease, whereas it can develop much earlier in the course of MSA. Urinary retention is also considerably more common in MSA than in Parkinson’s disease.31,44
Differentiating individuals with MSA from those with Parkinson’s disease is of very practical importance from the urological standpoint, because patients with MSA who undergo surgery for prostatic hypertrophy are at especially high risk for developing urinary incontinence as a complication of the procedure. Thus, medical management is preferable to surgical management of prostatic hypertrophy in individuals with MSA.31
Multiple Sclerosis
Symptoms of autonomic dysfunction may be present in almost 80% of patients with multiple sclerosis.45 Urinary symptoms are the most common, present in 65% of the 63 patients evaluated by McDougall and McLeod. In their study, urgency and frequency were especially common, and urinary incontinence was reported by more than 30% of patients.
Detrusor-sphincter dyssynergia, as a consequence of spinal cord involvement, is the most common urodynamic finding in multiple sclerosis, reported in 15% to 20% of affected individuals.46 However, because multiple sclerosis can affect all levels of the central nervous system, some patients show evidence of detrusor hyperreflexia as a result of involvement of suprapontine cerebral pathways.46 Impaired voiding with hesitancy, interrupted urinary flow, and incomplete voiding can also be present.47
Urinary symptoms increase in frequency and severity in tandem with disease severity and duration.48–50 They are most evident in individuals with secondary progressive multiple sclerosis.45
Spinal Cord Injury
Detrusor hyperreflexia develops in individuals with suprasacral cord lesions. Because spinal cord injuries are typically labeled by the level of the vertebral bodies injured, it is important to remember that the spinal cord actually ends at the L1-L2 vertebral level. Therefore, lesions above a T10 vertebral level evolve into a pattern of detrusor hyperreflexia or detrusor-sphincter dyssynergia, whereas the detrusor remains hyporeflexic with lesions below L2. If the injury is at vertebral levels T10-L2, either hyperreflexic or hyporeflexic bladder function may develop.51 If the spinal cord injury is complete in lesions above the T10 vertebral level, detrusor-sphincter dyssynergia is almost always present; with incomplete lesions, a pattern of detrusor hyperreflexia with maintained coordination of sphincter function is typically seen.52,53 Urodynamic testing is particularly valuable in assessing bladder function in patients with spinal cord injury at the thoracolumbar junction.54
When the vertebral injury is at the level of L2 or below, detrusor areflexia persists even after resolution of the period of spinal shock. The absence of detrusor function can be coupled with either intact sphincter function or with sphincter nonrelaxation.52
Treatment of Urinary Dysfunction
Neurogenic Detrusor Overactivity
Anticholinergic drugs have long been, and still remain, the standard treatment for detrusor overactivity (Table 29-3). Their effects are mediated via blockade of muscarinic cholinergic receptors located on the detrusor muscle. Although muscarinic receptors in human detrusor muscle are primarily of the M2 and M3 subtypes, older anticholinergic drugs are generally nonselective and block all five muscarinic receptor subtypes.55 Numerous adverse effects of these drugs, such as dry mouth and cognitive impairment, are the consequence of this nonselective blockade. Although still older anticholinergic drugs, such as hyoscyamine, atropine, propantheline, and flavoxate, are still occasionally used, oxybutynin and tolterodine have been the mainstays of treatment for a number of years. Both immediate- and extended-release preparations of these two drugs are available; oxybutynin is also available in a transdermal patch preparation. Oxybutynin is reported to have a higher propensity to produce central nervous system toxicity than does tolterodine, presumably because it crosses the blood-brain barrier more readily.56 The antimuscarinic armamentarium has expanded considerably with the introduction of trospium,57 solifenacin,58,59 and darifenacin.60 Trospium binds to M1, M2, and M3 receptors but does not cross the blood-brain barrier, whereas solifenacin and darifenacin are selective M3 receptor antagonists. These characteristics should diminish toxicity, but at increased expense.
In individuals who have not responded to or have been intolerant of antimuscarinic drugs, various other experimental treatment approaches have been tried. Gabapentin has been reported to improve symptoms of overactive bladder.61 Desmopressin has also been employed as a means to reduce nocturia in individuals in whom anticholinergic drugs alone have not been adequate.47,62 A more radical treatment approach has been the intravesical instillation of drugs. Both capsaicin and resiniferatoxin have been used in this manner.47 Resiniferatoxin is a capsaicin analogue, derived from the Euphorbia species (Euphorbia resinifera) of cactus found in Morocco, and is 1000 times more potent than capsaicin.63 These compounds are presumed to act by means of their toxic effects on nonmyelinated C fiber afferent nerves.47,63,64 Botulinum toxin injections into the detrusor muscle under cystoscopic guidance have also been used successfully in treating detrusor overactivity.65,66 Vesical pacing has also been reported to be useful.67 Surgical treatment is rarely indicated.
Detrusor-Sphincter Dyssynergia
In individuals with detrusor-sphincter dyssynergia, two problems must be attacked simultaneously. Anticholinergic drugs can reduce detrusor overactivity, but the failure of the urethral sphincter to relax during voiding must be addressed by other means. Intermittent self-catheterization remains the standard treatment approach for this problem,47 although botulinum toxin injections into the urethral sphincter have also been used.66 Incontinence is a potential complication of sphincter injections, but its incidence is low.66
Acontractile or Hypoactive Detrusor
There really is no effective medical treatment for incomplete bladder emptying that results from an underactive or acontractile detrusor muscle. Intermittent self-catheterization is the best treatment option in this situation.47 If self-catheterization is not possible, an indwelling catheter can be placed, but this increases the risk for recurrent urinary tract infections, bladder calculi, and urethral injury.47
SEXUAL FUNCTION
Neuroanatomy and Neurophysiology
Cerebrum
Although the cerebral cortex is presumed to be active in the realm of sexual desire, or libido, little is known about actual cortical localization of sexual function. Parasagittal primary sensory cortex receives sensory input from the genitalia, and the limbic cortex appears to play a role in sexual desire and behavior.68 Right frontal lobe activation during ejaculation has been identified in one study in which SPECT imaging was used.69 Additional evidence for frontal lobe involvement in sexual function comes from alterations in behavior, including sexual behavior, that have been observed in individuals with frontal lobe lesions.68 Temporal lobe dysfunction, especially in the setting of epilepsy, has also been implicated as a source of sexual dysfunction in both male and female patients; hypersexuality is occasionally seen, but sexual apathy is much more common.70,71 Hypothalamic involvement in sexual function and behavior has been clearly delineated. Hypothalamic injury can lead to a loss of sexual desire, as can occur in persons with pituitary tumors.68,72,73
Spinal Cord and Peripheral Nerves
As with many aspects of sexual function, more detailed information regarding neuroanatomical and neurophysiological pathways and function is available for male patients than for female patients. Two distinct pathways have been identified for erectile function: psychogenic and reflexogenic. Psychogenic erections are triggered by visual or auditory stimuli or by fantasy thinking, whereas reflexogenic erections are induced by genital stimulation.74 Intact spinal cord pathways are necessary for psychogenic erections, whereas reflexogenic erections are mediated through the sacral spinal cord at the S2-S4 levels. The afferent pathway for reflexogenic erection is via the pudendal nerve; the efferent limb, through pelvic parasympathetic fibers. Thus, parasympathetic pathways are operative primarily in the generation of penile erection, although sympathetic function plays a role in psychogenic erection and also in detumescence.74
Ejaculation is a phenomenon separate from erection and involves parasympathetic, sympathetic, and somatic contributions.74 Parasympathetic fibers produce secretion by accessory glands during arousal; sympathetic fibers are responsible for producing bladder neck closure and contraction of smooth muscle within the seminal vesicles; somatic fibers induce actual ejaculation by triggering contraction of the bulbocavernosus and ischiocavernosus muscles.74,75
Diagnostic Tests
Diagnostic testing for sexual dysfunction is more limited than that available for urological dysfunction, and it is limited primarily to the evaluation of erectile dysfunction (Table 29-4). Tests of both neurogenic and vascular integrity have been developed; vascular testing is not discussed here.
Nocturnal Penile Tumescence Testing
Nocturnal penile tumescence testing has been used in the past as a means of separating neurogenic from psychogenic erectile dysfunction.76 If an individual with erectile dysfunction was documented to attain a full erection while sleeping, a psychogenic basis for the erectile dysfunction was presumed to be present. However, it has been recognized more recently that such test results can be unreliable and even misleading.77,78
Sacral Reflex Testing
The bulbocavernosus reflex is the most frequently used sacral reflex test and typically involves electrical stimulation of the dorsal penile nerve with recording of the subsequent motor response in the bulbocavernosus muscle.20 Both the afferent and efferent responses of this reflex travel via the pudendal nerve. In patients with sacral cord (S2-S4) lesions or pudendal nerve lesions, latency of this reflex may be prolonged, or the reflex may be absent altogether. However, the sensitivity of this test is less than optimal,77 and its value in evaluating erectile dysfunction has been questioned.79
Pudendal Evoked Responses
The pudendal somatosensory evoked potential is elicited by electrically stimulating the dorsal penile nerve and recording from the cerebrum.20 Latency may be prolonged in persons with spinal cord abnormalities, but the sensitivity and specificity of the test have been questioned, and its usefulness beyond the more frequently employed tibial somatosensory evoked potential testing is uncertain.77
Specific Neurological Diseases
Epilepsy
Sexual dysfunction is more common in individuals with epilepsy than in the general population. However, studies have shown that it is not epilepsy itself but rather the location of the lesion responsible for the epilepsy that is the determining factor. Thus, individuals with focal temporal lobe epilepsy are more likely to experience sexual dysfunction than are persons with generalized epilepsy.1,70,71,80,81 Both hypersexuality and sexual apathy may occur, although the latter is much more frequent.1,68 Genital sensations or sexual behavior can also occur as ictal phenomena.68
Parkinson’s Disease
Alterations in sexual function are common in patients with Parkinson’s disease. In a survey of 115 such patients, Sakakibara and colleagues82 reported decreased libido in 84% of the women and 83% of the men; erectile dysfunction was present in 79% and impairment of ejaculation in 79% of the men. Other investigators have reported the presence of erectile dysfunction in 60% of individuals83 or a greater than twofold risk of developing erectile difficulty29 in men with Parkinson’s disease. Erectile dysfunction typically develops later in the course of Parkinson’s disease31; this is in sharp contrast with MSA, in which erectile dysfunction is often the initial clinical feature.84
Multiple Sclerosis
Although it is rarely a presenting feature,85–87 sexual dysfunction eventually develops in the majority of persons with multiple sclerosis. More than 50% of women with multiple sclerosis experience impaired sexual functioning, including decreased libido, difficulty achieving orgasm, and reduced lubrication.88,89 Although erectile dysfunction was noted less frequently in older studies, more recent reports indicate that it is present in approximately 50% to 70% of men with multiple sclerosis.45,87 Impairment of ejaculation is also common in men with multiple sclerosis.90 Some86,91 but not all92 reports note a correlation between signs of pyramidal tract involvement in the legs and the presence of erectile dysfunction in men with multiple sclerosis. Sexual dysfunction in multiple sclerosis is closely associated with urinary dysfunction in both men and women.45,87
Spinal Cord Injury
Erectile dysfunction can occur with both sacral and suprasacral spinal cord injury, but differences between the two manifestations are often evident. Men with clinically complete sacral cord injury are unable to achieve erection with genital stimulation but may be able to do so with psychogenic stimulation.74,93 In contrast, men with suprasacral cord injury can achieve erection with genital stimulation but are usually unable to do so with psychogenic stimulation if the spinal cord injury is at a cervical or thoracic level.74,93 Analogous abnormalities have been documented in women with spinal cord injuries. In women with complete upper motor neuron lesions, impaired vaginal lubrication during sexual excitation is typically evident, whereas vaginal lubrication may occur with psychogenic stimulation in women with sacral spinal cord injuries.94
Treatment of Sexual Dysfunction
The emergence of orally administered drugs that can enhance erections has revolutionized the treatment of erectile dysfunction (Table 29-5). Sildenafil, now joined by tadalafil and vardenafil, has been shown to be effective in men with spinal cord injury, multiple sclerosis, and other neurological conditions.95–98 These drugs are inhibitors of type 5 cyclic guanosine monophosphate phosphodiesterase, which via nitric oxide–mediated mechanisms produces smooth muscle relaxation and increases corpora cavernosa blood flow, thus enhancing penile erection.14,99 Sildenafil and related drugs are generally well tolerated, but headache, flushing, gastrointestinal upset, changes in color vision, and rhinitis may occur. Lethal adverse reactions have occurred in individuals taking nitrates concomitantly, and these drugs should be used very cautiously by persons with neurological diseases, such as Parkinson’s disease, in which orthostatic hypotension may occur. In fact, use of these drugs by persons with MSA is probably ill advised.
For individuals who cannot use or tolerate sildenafil and its analogues, other treatment approaches are available. Intracavernosal injections of alprostadil and moxisylyte are effective, but the requirement for injections, which are sometimes associated with significant pain, and the potential for development of fibrotic nodules within the corpora deter many individuals from using this form of treatment.94 Priapism may also occur. Intraurethral administration of alprostadil is also available. Vacuum devices, used in conjunction with constrictor bands, are also effective in inducing penile erection, but patient acceptance of the devices is low.
Dopamine agonist drugs have been shown to induce penile erection in both animals100 and humans.14,101 There is evidence that this may be caused specifically by D4 receptor–mediated activation of oxytocinergic neurons within the paraventricular nucleus of the hypothalamus.100 A sublingual apomorphine preparation has been developed for use by humans.14,101
CONCLUSION
Andersson KE. Antimuscarinics for treatment of overactive bladder. Lancet Neurol. 2004;3:46-53.
Apostolidis AN, Fowler CJ. Evaluation and treatment of autonomic disorders of the urogenital system. Semin Neurol. 2003;23:443-452.
Fowler CJ. Neurological disorders of micturition and their treatment. Brain. 1999;122:1213-1231.
Fowler CJ, editor. Neurology of Bladder, Bowel and Sexual Dysfunction. Boston: Butterworth Heinemann, 1999.
Singer C. Urinary dysfunction in Parkinson’s disease. In: Ebadi M, Pfeiffer RF, editors. Parkinson’s Disease. Boca Raton, FL: CRC Press; 2005:275-286.
1 Sakakibara R, Fowler CJ. Cerebral control of bladder, bowel, and sexual function and effects of brain disease. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:229-243.
2 Athwal BS, Berkley KJ, Hussain I, et al. Brain responses to changes in bladder volume and urge to void in healthy men. Brain. 2001;124:369-377.
3 Andrew J, Nathan PW. Lesions of the anterior frontal lobes and disturbances of micturition and defaecation. Brain. 1964;87:233-262.
4 Ueki K. Disturbances of micturition observed in some patients with brain tumor. Neurol Med Chir. 1960;2:25-33.
5 Maurice-Williams RS. Micturition symptoms in frontal tumours. J Neurol Neurosurg Psychiatry. 1974;37:431-436.
6 Sakakibara R, Hattori T, Yasuda K, et al. Micturitional disturbance after acute hemispheric stroke: analysis of the lesion site by CT and MRI. J Neurol Sci. 1996;137:47-56.
7 Zhang H, Reitz A, Kollias S, et al. An fMRI study of the role of suprapontine brain structures in the voluntary voiding control induced by pelvic floor contraction. Neuroimage. 2005;24:174-180.
8 Barrington FJF. The relation of the hindbrain to micturition. Brain. 1921;44:23-53.
9 Barrington FJF. The effect of lesions of the hind and midbrain on micturition in the cat. Q J Exp Physiol. 1925;15:81-102.
10 Holstege G, Griffiths D, de Wall H, et al. Anatomical and physiological observations on supraspinal control of bladder and urethral sphincter muscles in the cat. J Comp Neurol. 1986;250:449-461.
11 Griffiths D, Holstege G, Dalm E, et al. Control and coordination of bladder and urethral function in the brainstem of the cat. Neurourol Urodyn. 1990;9:63-82.
12 Taniguchi N, Miyata M, Yachiku S, et al. A study of micturition inducing sites in the periaqueductal gray of the mesencephalon. J Urol. 2002;168:1626-1631.
13 Onufrowicz B. Notes on the arrangement and function of the cell groups in the sacral region of the spinal cord. J Nerv Mental Dis. 1899;26:498-504.
14 Apostolidis AN, Fowler CJ. Evaluation and treatment of autonomic disorders of the urogenital system. Semin Neurol. 2003;23:443-452.
15 Lundberg JM. Pharmacology of cotransmission in the autonomic nervous system: integrative aspects on amines, neuropeptides, adenosine triphosphate, amino acids and nitric oxide. Pharmacol Rev. 1996;48:113-178.
16 Yoshimura N. Bladder afferent pathway and spinal cord injury: possible mechanisms inducing hyperreflexia of the urinary bladder. Prog Neurobiol. 1999;57:583-606.
17 Fowler CJ. Bladder afferents and their role in the overactive bladder. Urology. 2002;59(5, Suppl 1):37-42.
18 Abrams P, Cardozo L, Fall M, et al. The standardization of terminology in lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Urology. 2003;61:37-49.
19 Swinn MJ. Urodynamics. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:97-107.
20 Vodušek DB, Fowler CJ. Clinical neurophysiology. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:109-143.
21 Korpelainen JT, Sotaniemi KA, Myllyla VV. Autonomic nervous system disorders in stroke. Clin Auton Res. 1999;9:325-333.
22 Brittain KR, Peet SM, Castleden CM. Stroke and incontinence. Stroke. 1998;29:524-528.
23 Sakakibara R, Hattori T, Yasuda K, et al. Micturitional disturbance and the pontine tegmental lesion: urodynamic and MRI analyses of vascular cases. J Neurol Sci. 1996;141:105-110.
24 Kong KH, Young S. Incidence and outcome of poststroke urinary retention: a prospective study. Arch Phys Med Rehabil. 2000;81:1464-1467.
25 Gelber DA, Good DC, Laven LJ, et al. Causes of urinary incontinence after acute hemispheric stroke. Stroke. 1993;24:378-382.
26 Arena MG, Di Rosa AE, Arcudi L, et al. Voiding disorders in patients with cerebrovascular disease. Funct Neurol. 1992;7:47-49.
27 Singer C. Urological dysfunction. In: Pfeiffer RF, Bodis-Wollner I, editors. Parkinson’s Disease and Nonmotor Dysfunction. Totowa, NJ: Humana Press; 2005:139-148.
28 Singer C. Urinary dysfunction in Parkinson’s disease. In: Ebadi M, Pfeiffer RF, editors. Parkinson’s Disease. Boca Raton, FL: CRC Press; 2005:275-286.
29 Hobson P, Islam W, Roberts S, et al. The risk of bladder and autonomic dysfunction in a community cohort of Parkinson’s disease patients and normal controls. Parkinsonism Relat Disord. 2003;10:67-71.
30 Campos-Sousa RN, Quagliato E, da Silva BB, et al. Urinary symptoms in Parkinson’s disease. Prevalence and associated factors. Arq Neuropsiquiatr. 2003;61:359-363.
31 Chandiramani VA, Palace J, Fowler CJ. How to recognize patients with parkinsonism who should not have urological surgery. Br J Urol. 1997;80:100-104.
32 Chandiramani VA, Fowler CJ. Urogenital disorders in Parkinson’s disease and multiple system atrophy. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:245-254.
33 Araki I, Kitahara M, Oida T, et al. Voiding dysfunction in Parkinson’s disease: urodynamic abnormalities and urinary symptoms. J Urol. 2000;164:1640-1643.
34 Murnaghan GF. Neurogenic disorders of the bladder in parkinsonism. Br J Urol. 1961;33:403-409.
35 Pavlakis AJ, Siroky MB, Goldstein I, et al. Neurourologic findings in Parkinson’s disease. J Urol. 1983;129:80-83.
36 Fitzmaurice H, Fowler CJ, Rickards D, et al. Micturition disturbance in Parkinson’s disease. Br J Urol. 1985;57:652-656.
37 Galloway NTM. Urethral sphincter abnormalities in parkinsonism. Br J Urol. 1983;55:691-693.
38 Stocchi F, Carbone A, Inghilleri M, et al. Urodynamic and neurophysiological evaluation in Parkinson’s disease and multiple system atrophy. J Neurol Neurosurg Psychiatry. 1997;62:507-511.
39 Yoshimura N, Kuno S, Chancellor MB, et al. Dopaminergic mechanisms underlying bladder hyperactivity in rats with a unilateral 6-hydroxydopamine (6-OHDA) lesion of the nigrostriatal pathway. Br J Pharmacol. 2003;139:1425-1432.
40 Yoshimura N, Mizuta E, Yoshida O, et al. Therapeutic effects of dopamine D1/D2 receptor agonists on detrusor hyperreflexia in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridinelesioned parkinsonian cynomolgus monkeys. J Pharmacol Exp Ther. 1998;286:228-233.
41 Kuno S, Mizuta E, Yamasaki S, et al. Effects of pergolide on nocturia in Parkinson’s disease: three female cases selected from over 400 patients. Parkinsonism Relat Disord. 2004;10:181-187.
42 Wenning GK, Colosimo C, Geser F, et al. Multiple system atrophy. Lancet Neurol. 2004;3:93-103.
43 Kirby R, Fowler CJ, Gosling J, et al. Urethrovesical dysfunction in progressive autonomic failure with multiple system atrophy. J Neurol Neurosurg Psychiatry. 1986;49:554-562.
44 Bonnet AM, Pichon J, Vidailhet M, et al. Urinary disturbances in striatonigral degeneration and Parkinson’s disease: clinical and urodynamic aspects. Mov Disord. 1997;12:509-513.
45 McDougall AJ, McLeod JG. Autonomic nervous system function in multiple sclerosis. J Neurol Sci. 2003;215:79-85.
46 Shah DK, Badlani GH. Urological symptoms. In: Voltz R, Bernat JL, Borasio GD, et al, editors. Palliative Care in Neurology. Oxford, UK: Oxford University Press; 2004:262-271.
47 Fowler CJ. Neurological disorders of micturition and their treatment. Brain. 1999;122:1213-1231.
48 Nortvedt MW, Riise T, Myhr KM, et al. Reduced quality of life among multiple sclerosis patients with sexual disturbance and bladder dysfunction. Mult Scler. 2001;7:231-235.
49 Giannantoni A, Scivoletto G, Di Stasi SM, et al. Lower urinary tract dysfunction and disability status in patients with multiple sclerosis. Arch Phys Med Rehabil. 1999;80:437-441.
50 Barbalius GA, Nikiforidis G, Liatsikos EN. Vesicourethral dysfunction associated with multiple sclerosis: clinical and urodynamic perspectives. J Urol. 1998;160:106-111.
51 Wyndaele JJ. Correlation between clinical neurological data and urodynamic function in spinal cord injured patients. Spinal Cord. 1997;35:213-216.
52 Van Kerrebroeck PEV. Lower urinary tract dysfunction in spinal cord injury. In: Corazziari E, editor. Neurogastroenterology. Berlin: Walter de Gruyter; 1996:289-299.
53 Kaplan SA, Chancellor MB, Blaivas J. Bladder and sphincter behavior in patients with spinal cord lesions. J Urol. 1991;146:113-117.
54 Pesce F, Castellano V, Finazzi Agro E, et al. Voiding dysfunction in patients with spinal cord lesions at the thoracolumbar vertebral junction. Spinal Cord. 1997;35:37-39.
55 Andersson KE. Antimuscarinics for treatment of overactive bladder. Lancet Neurol. 2004;3:46-53.
56 Todorova A, Vonderheid-Guth B, Dimpfel W. Effects of tolterodine, trospium chloride, and oxybutynin on the central nervous system. J Clin Pharmacol. 2001;41:636-644.
57 Rovner ES. Trospium chloride in the management of overactive bladder. Drugs. 2004;64:2433-2446.
58 Chilman-Blair K, Bosch JL. Solifenacin: treatment of overactive bladder. Drugs Today (Barc). 2004;40:343-353.
59 Brunton S, Kurtizky L. Recent developments in the management of overactive bladder: focus on the efficacy and tolerability of once daily solifenacin succinate 5 mg. Curr Med Res Opin. 2005;21:71-80.
60 Cardozo L, Dixon A. Increased warning time with darifenacin: a new concept in the management of urinary urgency. J Urol. 2005;173:1214-1218.
61 Kim YT, Kwon DD, Kim J, et al. Gabapentin for overactive bladder and nocturia after anticholinergic failure. Int Braz J Urol. 2004;30:275-278.
62 Dasgupta P, Haslam C. Treatment of neurogenic bladder dysfunction. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:163-183.
63 Palma PCR, Thiel M, Riccetto CLZ, et al. Resiniferatoxin for detrusor instability refractory to anticholinergics. Int Braz J Urol. 2004;30:53-58.
64 Kuo HC. Multiple intravesical instillation of low-dose resiniferatoxin is effective in the treatment of detrusor overactivity refractory to anticholinergics. BJU Int. 2005;95:1023-1027.
65 Hajebrahimi S, Altaweel W, Cadoret J, et al. Efficacy of botulinum-A toxin in adults with neurogenic overactive bladder: initial results. Can J Urol. 2005;12:2543-2546.
66 Smith CP, Nishiguchi J, O’Leary M, et al. Single-institution experience in 110 patients with botulinum toxin A injection into bladder or urethra. Urology. 2005;65:37-41.
67 Shafik A, El Sibai O, Shafik AA, et al. Vesical pacing: pacing parameters required for normalization of vesical electric activity in patients with overactive bladder. Front Biosci. 2004;9:995-999.
68 Lundberg PO. Physiology of female sexual function and effect of neurologic disease. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:33-46.
69 Tiihonen J, Kuikka J, Kupila J, et al. Increase in cerebral blood flow of right prefrontal cortex in man during orgasm. Neurosci Lett. 1994;170:241-243.
70 Shukla GD, Srivastava ON, Katiyar BC. Sexual disturbances in temporal lobe epilepsy: a controlled study. Br J Psychiatry. 1979;134:288-292.
71 Blumer D, Walker AE. Sexual behavior in temporal lobe epilepsy. A study of the effects of temporal lobectomy on sexual behavior. Arch Neurol. 1967;16:37-43.
72 Hulting AL, Muhr C, Lundberg PO, et al. Prolactinomas in men: clinical characteristics and the effect of bromocriptine treatment. Acta Med Scand. 1985;217:101-109.
73 Lundberg PO, Hulter B. Sexual dysfunction in patients with hypothalamopituitary disorders. Exp Clin Endocrinol. 1991;98:81-88.
74 Beck RO. Physiology of male sexual function and dysfunction in neurologic disease. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:47-56.
75 Hoyle CHV, Lincoln J, Burnstock G. Neural control of pelvic organs. In: Rushton DN, editor. Handbook of Neuro-Urology. New York: Marcel Dekker; 1994:1-54.
76 Karacan I, Williams RL, Thornby JI, et al. Sleep-related penile tumescence as a function of age. Am J Psychiatry. 1975;132:932-937.
77 Beck RO. Investigation of male erectile dysfunction. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:145-160.
78 Schmidt MH, Schmidt HS. Sleep-related erections: neural mechanisms and clinical significance. Curr Neurol Neurosci Rep. 2004;4:170-178.
79 Nogueira MC, Herbaut AG, Wespes E. Neurophysiological investigations of two hundred men with erectile dysfunction. Interest of bulbocavernosus reflex and pudendal evoked responses. Eur Urol. 1990;18:37-41.
80 Lundberg PO. Sexual dysfunction in patients with neurological disorders. Annu Rev Sex Res. 1992;3:121-150.
81 Lundberg PO, Brattberg A. Sexual dysfunction in selected neurologic disorders: hypothalamopituitary disorders, epilepsy, myelopathies, polyneuropathies, and sacral nerve lesions. Semin Neurol. 1992;12:115-119.
82 Sakakibara R, Shinotoh H, Uchiyama T, et al. Questionnairebased assessment of pelvic organ dysfunction in Parkinson’s disease. Auton Neurosci. 2001;92:76-85.
83 Singer C, Weiner WJ, Sanchez-Ramos JR. Autonomic dysfunction in men with Parkinson’s disease. Eur Neurol. 1992;32:134-140.
84 Beck RO, Betts CD, Fowler CJ. Genitourinary dysfunction in multiple system atrophy: clinical features and treatment in 62 cases. J Urol. 1994;151:1336-1341.
85 Müller R. Studies on disseminated multiple sclerosis. Acta Med Scand. 1949;222:67-71.
86 Betts CD, Jones SJ, Fowler CG, et al. Erectile dysfunction in multiple sclerosis. Associated neurological and neurophysiological deficits, and treatment of the condition. Brain. 1994;117:1303-1310.
87 Betts CD. Bladder and sexual dysfunction in multiple sclerosis. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:289-308.
88 Lundberg PO. Sexual dysfunction in female patients with multiple sclerosis. Int Rehabil Med. 1981;3:32-34.
89 Hulter BM, Lundberg PO. Sexual function in women with advanced multiple sclerosis. J Neurol Neurosurg Psychiatry. 1995;59:83-86.
90 Zorzon M, Zivadinov R, Bosco A, et al. Sexual dysfunction in multiple sclerosis: a case-control study. I. Frequency and comparison of groups. Mult Scler. 1999;5:418-427.
91 Valleroy ML, Kraft GH. Sexual dysfunction in multiple sclerosis. Arch Phys Med Rehabil. 1984;65:125-128.
92 Minderhoud JM, Leemhuis JG, Kremer J, et al. Sexual disturbances arising from multiple sclerosis. Acta Neurol Scand. 1984;70:299-306.
93 Bors E, Comarr AE. Neurological disturbance of sexual function with special reference to 529 patients with spinal cord injury. Urol Surv. 1960;10:191-222.
94 Hatzichristou DG. Treatment of sexual dysfunction and infertility in patients with neurologic diseases. In: Fowler CJ, editor. Neurology of Bladder, Bowel, and Sexual Dysfunction. Boston: Butterworth Heinemann; 1999:209-225.
95 Derry F, Hultling C, Seftel AD, et al. Efficacy and safety of sildenafil citrate (Viagra) in men with erectile dysfunction and spinal cord injury: a review. Urology. 2002;60(2, Suppl 2):49-57.
96 Langtry HD, Markham A. Sildenafil: a review of its use in erectile dysfunction. Drugs. 1999;57:967-989.
97 Sanchez Ramos A, Vidal J, Jauregui ML, et al. Efficacy, safety and predictive factors of therapeutic success with sildenafil for erectile dysfunction in patients with different spinal cord injuries. Spinal Cord. 2001;39:637-643.
98 Doggrell SA. Comparison of clinical trials with sildenafil, vardenafil and tadalafil in erectile dysfunction. Expert Opin Pharmacother. 2005;6:75-84.
99 Hallén K, Gustafsson LE, Wiklund NP. Nerve-induced release of nitric oxide from the rabbit corpus cavernosum is modulated by cyclic guanosine 3′,5′-monophosphate. Neuroscience. 2005;133:169-174.
100 Melis MR, Succu S, Mascia MS, et al. PD-168077, a selective dopamine D4 receptor agonist, induces penile erection when injected into the paraventricular nucleus of male rats. Neurosci Lett. 2005;379:59-62.
101 Montorsi F, Salonia A, Dehò F, et al. Pharmacological management of erectile dysfunction. BJU Int. 2003;91:446-454.