44 Biliary Tract Disorders
• Risk factors for the development of gallstone disease include female gender, increasing age, obesity, rapid weight loss, and underlying liver disease.
• The majority of patients with gallstone disease are asymptomatic. Symptomatic complications include biliary colic, acute cholecystitis, choledocholithiasis, cholangitis, and acute pancreatitis.
• A high index of suspicion should be maintained for acute cholangitis in the chronically ill, elderly, or diabetic patients with sepsis of unknown source.
• Ultrasound is the initial diagnostic study of choice in patients with suspected gallstone disease. Cholecystoscintigraphy is the most sensitive test for cholecystitis, and magnetic resonance cholangiopancreatography is the most sensitive test for bile duct stones.
Cholelithiasis and Acute Cholecystitis
Epidemiology
Cholelithiasis affects 20 to 25 million Americans, which represents 10% to 15% of the adult population. Although most gallstones are clinically silent, 20% of people harboring stones experience biliary symptoms at some time; 1% to 2% of patients each year experience complications and require surgical removal of the gallbladder. In the United States, cholecystectomy is the most common elective abdominal surgery, with approximately 750,000 procedures performed per year. Complications of cholelithiasis include acute cholecystitis, ascending cholangitis, acute pancreatitis, and adenocarcinoma of the gallbladder, which result in a combined mortality of 5000 to 10,000 deaths per year (Box 44.1).
Box 44.1 Risk Factors for the Development of Cholelithiasis
Gender
Women have twice the incidence and prevalence of gallstones.
Estrogen stimulates low-density lipoprotein receptors and increases the uptake of cholesterol; higher cholesterol content in bile is associated with greater risk for gallstone formation.1
After menopause, the incidence of gallstone disease in women and men is comparable.
Total Parenteral Nutrition
Loss of enteric stimulation of the gallbladder in the absence of eating leads to gallbladder stasis.
Total parental nutrition (TPN) increases the risk for biliary sludge, gallstone disease, and acalculous cholecystitis.
After 4 weeks of TPN, gallbladder sludge develops in half of patients and after 6 weeks in all. The sludge resolves within 4 weeks of resuming oral intake.4
Family History
Occurrence of gallstone disease within families can be a product of genetic and shared environmental factors.5
The frequency is increased in monozygotic (12%) as opposed to dizygotic twins (6%).6
Genetic effects account for 25%, shared environmental effects for 13%, and unique environmental effects for 62% of the phenotypic variance in gallstone production.7
Chronic Diseases
The overall prevalence of gallstones in patients with cirrhosis is 25% to 30% (double that in the general population).8
Crohn disease causes ileal malabsorption of bile acids. These acids normally solubilize cholesterol and bilirubin to be excreted. An inadequate amount of bile acid means that increased cholesterol and bilirubin are available to form stones.9
Cystic fibrosis is also associated with bile acid malabsorption and gallstones.
Medications
Octreotide is used for the treatment of acromegaly and carcinoid syndrome; it affects biliary motility and sphincter of Oddi function. Cholelithiasis develops in more than 50% of patients receiving octreotide. The majority are asymptomatic.10
Ceftriaxone is secreted unmetabolized into bile, where it reaches high concentrations and produces biliary sludge.11
Pathophysiology
Bile is primarily composed of cholesterol, lecithin, bile salts, bilirubin, and electrolytes (i.e., calcium, carbonate, phosphate). Once these solutes exceed their solubility, they form crystals. Crystals trapped in biliary mucus produce sludge and aggregate to form stones. Cholesterol is the primary constituent in 60% to 80% of all gallstones. Calcium bilirubinate salts predominate in another 10% to 20% of stones; cholesterol and calcium bilirubinate are present in relatively equal quantities in the remainder of calculi. Biliary stasis is thought to play a significant role in stone formation.12
Although bile itself is normally sterile, any alterations in biliary motility lead to an increased risk for bacterial infection. The organisms implicated in cholecystitis are generally bowel flora and include Escherichia coli, Klebsiella, enterococci, and anaerobes.13
Presenting Signs and Symptoms
Gallstones can be manifested as a spectrum of disease and may be divided into asymptomatic, symptomatic, and complicated gallstone disease. Only 15% to 20% of stones become symptomatic, between 1% and 3% per year. Approximately 66% of patients have a recurrent episode of biliary colic within 2 years, and about one in six have a complication of gallstone disease13 (Table 44.1).
Table 44.1 Symptoms of Gallstone Disease and Its Complications
| DISEASE | PATHOPHYSIOLOGY | SYMPTOMS |
|---|---|---|
| Biliary colic | Transient gallstone impaction at the cystic duct or ampulla of Vater | Intermittent RUQ pain associated with nausea or vomiting. Pain in the epigastrium or radiating to the right scapular tip. Episodes last 30 min to several hours with days or months between episodes. |
| Acute cholecystitis | Inflammation of the gallbladder caused by obstruction of the cystic duct May occur in the presence or absence of bacterial superinfection |
Patients appear ill and cannot take deep breaths. They have constant pain that lasts 30-60 min and worsens with movement. Persistent common bile duct impaction usually promotes vomiting. Physical examination demonstrates RUQ tenderness with voluntary guarding and a positive Murphy sign (arrest of inspiration during deep palpation over the gallbladder). |
| Emphysematous cholecystitis | Infection with gas-producing bacteria such as Escherichia coli, Clostridium perfringens, and anaerobic streptococci | Symptoms are similar to those with acute cholecystitis. Gas may be seen on abdominal plain films or CT. Male diabetics are most commonly affected. |
| Chronic cholecystitis | Persistent inflammation and fibrosis of the gallbladder with poor motor and absorptive function | Patients are usually asymptomatic but may report multiple previous attacks of colic. Porcelain gallbladder develops from chronic inflammation and may progress to carcinoma. |
| Acalculous cholecystitis | Probably related to biliary stasis in the setting of critical illness and altered gastrointestinal motility | Seen in patients with traumatic injuries, burns, and critical illness, as well as in those receiving total parenteral nutrition. The mortality for this disorder is twice as high as that for acute calculous cholecystitis.14 |
| Gallbladder perforation | Stones erode through an inflamed and necrotic gallbladder wall Stones may travel into the peritoneal cavity or cause adhesions between nearby structures. Bile peritonitis may develop |
More than half of patients with gallbladder perforation have fever and a palpable RUQ mass.15 Mortality in these patients is 30%.16 |
CT, Computed tomography; RUQ, right upper quadrant.
Diagnostic Imaging for Cholelithiasis and Cholecystitis
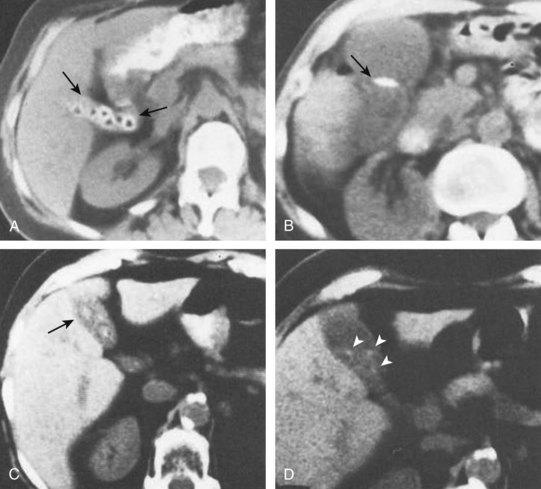
Ultrasonography is the preferred first-line modality for evaluating potential biliary stones (Fig. 44.1). A metaanalysis of studies demonstrated that ultrasound has a sensitivity of 97% and specificity of 95% for the diagnosis of cholelithiasis.17 Common findings on ultrasonography are hyperechoic stones with hypoechoic shadowing, biliary sludge, and stone mobility with changes in patient positioning (Fig. 44.2). Pericholecystic fluid (Fig. 44.3), gallbladder wall thickening (>3 mm), common bile duct dilation (>6 mm), and intrahepatic and extrahepatic biliary ductal dilation are highly suggestive of acute cholecystitis.
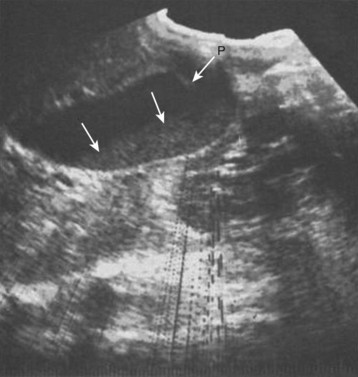
Fig. 44.1 Ultrasonogram demonstrating biliary sludge (arrows).
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 206.)
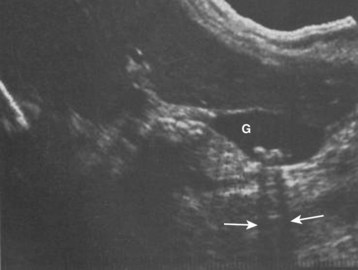
Fig. 44.2 Cholelithiasis shown by ultrasonography (arrows).
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 255.)

Fig. 44.3 Ultrasonogram demonstrating pericholecystic fluid (arrow).
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 213.)
Cholecystoscintigraphy or hepatobiliary iminodiacetic acid (HIDA) scanning is a more sensitive test for diagnosing acute cholecystitis. In this nuclear medicine study, a radioactive tracer is injected peripherally and allowed to circulate to the liver, where it is excreted in bile. In the absence of disease, the gallbladder is visualized within 1 hour of injection (Fig. 44.4). Nonvisualization of the gallbladder within 4 hours after injection indicates either cholecystitis or cystic duct obstruction (Fig. 44.5). In a retrospective review of 170 patients evaluated in the emergency department (ED) because of right upper quadrant (RUQ) pain, cholecystoscintigraphy had a diagnostic sensitivity of 86% for acute cholecystitis as compared with 48% for ultrasonography. In another study, the results of cholecystoscintigraphy were positive in 87% of patients in whom the initial ultrasonographic findings were negative.18
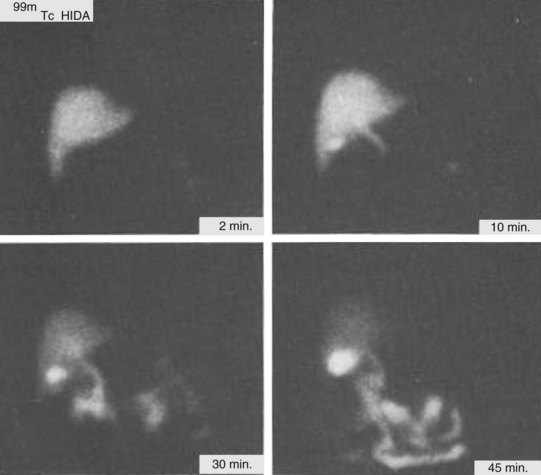
Fig. 44.4 Normal cholecystoscintigrams.
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 265.)
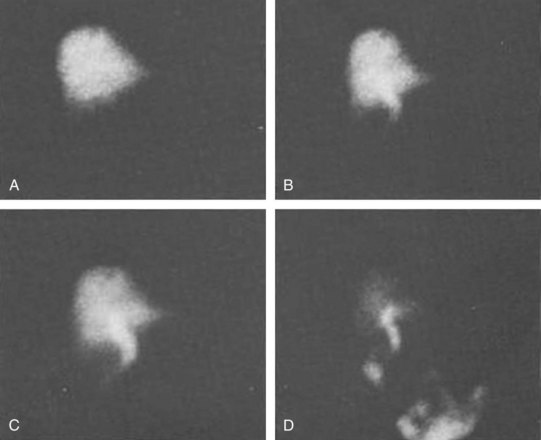
Fig. 44.5 A to D, Abnormal cholecystoscintigrams.
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 273.)
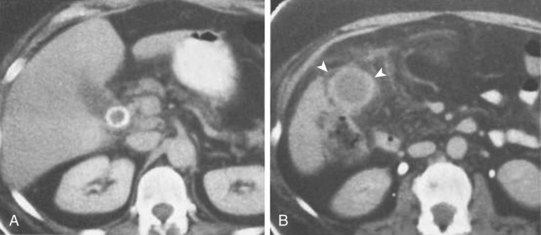
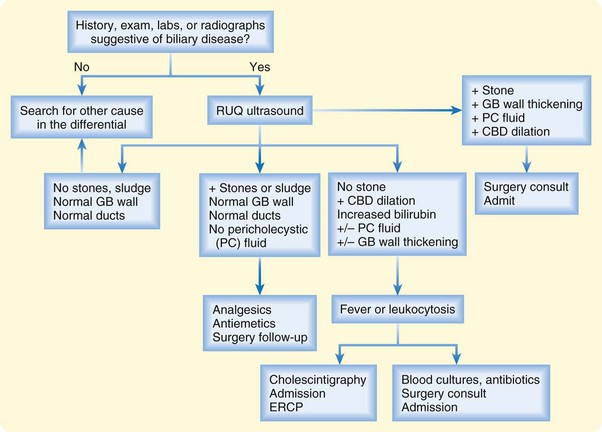
Computed tomography (CT) is less sensitive than ultrasonography for the diagnosis of acute biliary disease.19 CT may offer valuable information about the surrounding anatomy if confounding clinical signs or symptoms are present, if ultrasonography does not demonstrate calculus, or if an alternative diagnosis is as likely as biliary disease (Fig. 44.6). A retrospective study of 123 patients who underwent both CT and RUQ ultrasonography demonstrated a sensitivity of only 39% for CT in detecting biliary disease.19 Ultrasonography had a sensitivity of 83% in that study and suggested the correct diagnosis in seven of eight patients in whom the CT findings led to misdiagnosis (Fig. 44.7). Figure 44.8 presents a summary of the diagnostic and treatment algorithm for right upper quadrant pain.
Treatment
Medical Management
Empiric antibiotics should cover E. coli, Klebsiella, Streptococcus faecalis, and anaerobic organisms. An acceptable combination regimen consists of a third- or fourth-generation cephalosporin (e.g., ceftazidime) plus metronidazole. An alternative would be a combination of a β-lactam antibiotic and a β-lactamase inhibitor such as piperacillin and tazobactam or ampicillin and sulbactam.13
Medical therapy for chronic gallstone disease may include oral bile acids or extracorporal shock wave lithotripsy (ESWL). Oral bile acids dissolve cholesterol gallstones. The most commonly used agent is ursodeoxycholic acid, which is a primary bile acid of bears. It both dissolves cholesterol gallstones and reduces biliary cholesterol secretion.20 ESWL fragments gallstones with external shock waves. These stones are then more amenable to dissolution with oral bile acids. The major complications are biliary colic and problems stemming from the expulsion of smaller gallstones, such as acute pancreatitis.21
Surgical Management
Laparoscopic cholecystectomy is the mainstay of surgical treatment of symptomatic gallstones. When compared with open cholecystectomy, laparoscopic surgery is associated with decreased postoperative pain; decreased hospital length of stay; decreased risk for mortality, cardiopulmonary complications, and wound infections, but also with an increased risk for bile duct injuries.22,23 Cholecystectomy is also the treatment of choice for acute cholecystitis. Although the timing of surgery in this context has been debated, early cholecystectomy within a few days of initial evaluation is probably associated with lower morbidity and mortality.24 Patients who are critically ill or have acute contraindications to cholecystectomy can be temporized with percutaneous cholecystostomy for drainage pending definitive management.
The most common immediate complication of cholecystectomy is bile leakage, which is treated by endoscopic retrograde cholangiopancreatography (ERCP) with stent placement.25 Stent placement decreases outflow resistance and allows spontaneous closure of the leak, usually within a few days. Postoperative cholecystectomy patients with recurrent abdominal symptoms should be evaluated for retained stones along with choledocholithiasis, pancreatitis, abscess, or bile leak.
Choledocholithiasis and Cholangitis
Epidemiology
Approximately 80% of cases of cholangitis are caused by obstructing gallbladder stones, with a reported mortality of 5%.26
Pathophysiology
E. coli, Klebsiella, Streptococcus, Clostridium, and Bacteroides are the common bacterial organisms inciting cholangitis. Infection usually spreads in a retrograde fashion from the intestines because of obstruction. The resulting damage to the biliary ductal epithelium causes fibrosis and ductal loss. This sequence of events may also be seen without biliary obstruction in patients who have undergone sphincteroplasty or biliary anastomosis to the duodenum (sump syndrome).15
Infection by the Chinese liver fluke (Clonorchis sinensis) with secondary bacterial infection can cause cholangitis. Patients with acquired immunodeficiency syndrome may have cholangitis with or without obstruction. The infectious organisms associated with this and other immunodeficiency disorders are cytomegalovirus, Cryptosporidium, Cryptococcus, and Candida albicans.27,28 Neonates may have cholangitis secondary to cytomegalovirus or reovirus type III. Cholangitis may also be seen in patients with failing liver transplants as a result of graft incompatibility or hepatic arterial thrombosis.29 Rejection leading to cholangitis is likewise seen in patients who have undergone allogeneic bone marrow transplantation.30 Progressive biliary ductal necrosis eventually leads to cirrhosis (Table 44.2).
Table 44.2 Signs and Symptoms of Choledocholithiasis and Cholangitis
| DISEASE | PATHOPHYSIOLOGY | SIGNS AND SYMPTOMS |
|---|---|---|
| Choledocholithiasis | Obstruction of the common bile duct by a gallstone that either migrates from the gallbladder or (less commonly) forms primarily in the duct Obstruction of the pancreatic duct can cause acute gallstone pancreatitis |
Manifestations are similar to those of biliary colic, but jaundice may develop. |
| Cholangitis | Inflammation of the bile ducts May be caused by infection (bacterial, viral, tuberculin) or autoimmune reaction |
The Charcot triad of fever, jaundice, and RUQ pain is neither sensitive nor specific.31 The addition of obtundation and hypotension to the triad constitutes the Reynold pentad. Patients with infectious cholangitis are usually older, appear ill, and may not complain of RUQ pain. Younger patients with diabetes can also have nonspecific complaints. |
| Acute gallstone pancreatitis | Increased pancreatic ductal pressure, possibly with biliopancreatic reflux, that occurs when the bile duct stone passes or becomes impacted at the ampulla of Vater | Patients typically have a sudden onset of unrelenting upper abdominal pain that radiates to the back in about 50% of cases.32 |
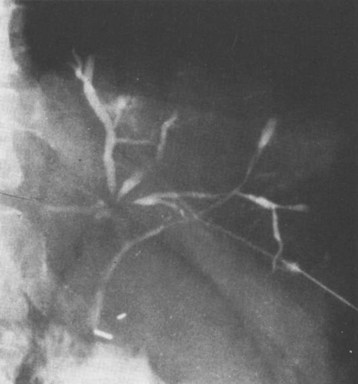
| Primary sclerosing cholangitis (PSC) | Immune-mediated progressive fibrosis of the intrahepatic or extrahepatic biliary ducts (Fig. 44.9) | More than 70% of patients with PSC have concomitant inflammatory bowel disease, and elevated alkaline phosphatase is found on routine screening.15 The majority of patients with PSC are asymptomatic until signs of cirrhosis develop. Common symptoms are RUQ pain, jaundice, pruritus, weight loss, and fatigue. |
RUQ, Right upper quadrant.
Differential Diagnosis and Medical Decision Making
Laboratory evaluation may help distinguish biliary colic and cholecystitis from choledocholithiasis. In choledocholithiasis, more than 90% of patients will have elevations in serum alkaline phosphatase and GGT levels.33 Obstruction of the common bile duct will lead to elevation of total and conjugated serum bilirubin, although most ductal stones result in serum bilirubin levels lower than 15 mg/dL because the biliary obstruction that they cause is intermittent. Serum transaminase levels may be elevated, rarely with profound elevations of greater than 2000 IU/L mimicking acute hepatitis.32
Transabdominal ultrasound has low sensitivity (25% to 60%) for the detection of bile duct stones, but it has a very high specificity.32 Stones within the common bile duct are difficult to visualize on ultrasonography, but greater than 6-mm dilation of the common bile duct suggests the presence of a calculus. CT imaging also has low sensitivity for bile duct stones but can demonstrate biliary dilation and exclude other causes of biliary obstruction such as tumor. Magnetic resonance cholangiopancreatography and ERCP can detect stones with comparable accuracy (Fig. 44.9).34
Treatment
Initial management of cholangitis is typically medical with empiric antibiotics. Multiple antibiotic regimens are acceptable, and emergency physicians should follow institutional preferences and local resistance patterns when choosing antibiotics. Accepted regimens are combination therapy with an extended-spectrum cephalosporin, metronidazole, and ampicillin; single-agent or combination fluoroquinolones; and ureidopenicillins alone or with metronidazole.35 Although fluoroquinolones are thought to have greater biliary penetration, they do not change the mortality associated with this disease.36 Unless concomitant signs of infection are present, patients with primary sclerosing cholangitis do not experience improvement with antibiotics.
ERCP with sphincterotomy is the treatment with the lowest mortality.37 Percutaneous transhepatic cholangiography (PTC) with drainage is a consideration for patients in whom ERCP fails.38 Emergency common bile duct exploration with T-tube placement can be performed either by open means or laparoscopically.32 If emergency ERCP or PTC cannot be arranged in the ED, surgical consultation should be obtained.
Tumors of the Biliary Tree and Gallbladder
Epidemiology
Tumors of the biliary tree are relatively rare and range from benign tumors such as adenoma and papilloma to carcinoma of the gallbladder and cholangiocarcinoma. Because gallbladder carcinoma is closely associated with underlying gallbladder disease and chronic stasis, patient populations at risk for gallstone disease are also at higher risk for gallbladder carcinoma (see Box 44.1).39 The overall 5-year survival rate in patients with gallbladder cancer is approximately 12%.40
Pathophysiology
Carcinoma of the gallbladder is an uncommon malignancy associated with chronic cholecystitis and porcelain gallbladder (Fig. 44.10). It is most commonly an adenocarcinoma that arises in the fundus or neck. Physical examination usually demonstrates jaundice in an elderly patient, RUQ pain, and weight loss. An abdominal mass may be palpable.

Fig. 44.10 Computed tomography scan showing gallbladder carcinoma (arrowheads).
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 256.)
Cholangiocarcinoma refers to malignancy anywhere from the intrahepatic ducts to the common bile duct. It is an adenocarcinoma that spreads along and through the duct wall, with extension to the lymph nodes, peritoneum, gallbladder, and liver in 50% of patients. Associations with primary biliary cirrhosis (PBC), primary sclerosing cholangitis, ulcerative colitis, and C. sinensis infestation have been documented. One study found that the risk for bile duct carcinoma significantly decreases 10 years after cholecystectomy.41
Presenting Signs and Symptoms
Patients are most commonly seen in the ED with painless jaundice and pruritus, symptoms that suggest an obstructing mass in the distal biliary tree. Pain is present in only one third of patients and is generally mild.15 Those with malignancy have associated malaise and weight loss. Hepatomegaly without splenomegaly is often noted. Fever is uncommon, but if present, concurrent cholangitis should be considered.
Differential Diagnosis and Medical Decision Making
Both ultrasonography and CT have a sensitivity of 60% to 70% for detecting carcinoma42; when results are positive, they usually show a mass in the lumen. Spread via the venous and lymphatic systems prevents early detection, and metastasis is present at the time of diagnosis in 50% of cases.43 The 1-year survival rate after diagnosis is approximately 14%.44
Primary Biliary Cirrhosis
Epidemiology
PBC progressively destroys the intrahepatic bile ducts (Fig. 44.11). The disease is found in all races, with a 90% female preponderance. PBC is diagnosed in patients 20 to 80 years of age, although the majority of cases are found in patients 40 to 60 years old. A genetic predisposition is likely because family members of patients with PBC have a higher prevalence of mitochondrial antibodies associated with the disease. A medical history of an autoimmune disorder such as rheumatoid arthritis, systemic lupus erythematosus, or mixed connective tissue disease has an association with PBC.13
Differential Diagnosis and Medical Decision Making
The most common laboratory abnormality is an elevation in serum alkaline phosphatase and GGT. Total serum cholesterol is usually elevated and the serum bilirubin value only mildly elevated (generally less than 2 mg/dL).15 Complications of the disease result from liver cirrhosis (i.e., ascites, bleeding esophageal varices, coagulopathy). The diagnosis is suggested by antimitochondrial antibodies in the serum and confirmed by liver biopsy.
Treatment
Treatment is initially aimed at controlling itching and steatorrhea. Vitamin D and calcium supplements are necessary because of the bile deficiency. The only drug shown to improve mortality in patients with PBC is ursodeoxycholic acid. Hepatic transplantation is the best treatment option to extend life, with a 5-year survival rate of 60% to 70%.45
Attasaranya S, Fogel E, Lehman G. Choledocholithiasis, ascending cholangitis and gallstone pancreatitis. Med Clin North Am. 2008;92:925–960.
Kalimi R, Gecelter GR, Caplin D, et al. Diagnosis of acute cholecystitis: sensitivity of sonography, cholescintigraphy, and combined sonography-cholescintigraphy. J Am Coll Surg. 2001;193:609–613.
Schiff ER, Sorrell MF, Maddey WC, eds. Schiff’s diseases of the liver, 8th ed, vol 1. Philadelphia: Lippincott-Raven, 1999.
1 Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin North Am. 2010;39:157–169.
2 Maclure KM, Hayes KC, Colditz GA. Weight, diet, and the risk of symptomatic gallstones in middle-aged women. N Engl J Med. 1989;321:563–569.
3 Weinsier RL, Wilson LJ, Lee J. Medically safe rate of weight loss for the treatment of obesity: a guideline based on risk of gallstone formation. Am J Med. 1995;98:115–117.
4 Angelico M, Della GP. Review article: hepatobiliary complications associated with total parenteral nutrition. Aliment Pharmacol Ther. 2000;14(Suppl):254–257.
5 Lammert F, Miquel JF. Gallstone disease: from genes to evidence-based therapy. J Hepatol. 2008;48(Suppl. 1):S124–S135.
6 Sarin SK, Negi VS, Dewan R, et al. High familial prevalence of gallstones in the first-degree relatives of gallstone patients. Hepatology. 1995;22:138–141.
7 Katsika D, Grjibovski A, Einarsson C, et al. Genetic and environmental influences on symptomatic gallstone disease: a Swedish study of 43,141 twin pairs. Hepatology. 2005;41:1138–1143.
8 Conte D, Fraquelli M, Fornari F, et al. Close relation between cirrhosis and gallstones: cross-sectional and longitudinal survey. Arch Intern Med. 1999;159:49–52.
9 Vitek L, Carey MC. Enterohepatic cycling of bilirubin as a cause of ‘black’ pigment gallstones in adult life. Eur J Clin Invest. 2003;33:799–810.
10 Trendle MC, Moertel CG, Kvols LK. Incidence and morbidity of cholelithiasis in patients receiving chronic octreotide for metastatic carcinoid and malignant islet cell tumors. Cancer. 1997;79:830–834.
11 Bickford CL, Spencer AP. Biliary sludge and hyperbilirubinemia associated with ceftriaxone in an adult: case report and review of the literature. Pharmacotherapy. 2005;25:1389–1395.
12 Portincasa P, Moschetta A, Palasciano G. Cholesterol gallstone disease. Lancet. 2006;368:230–239.
13 Schiff ER, Sorrell MF, Maddey WC, eds. Schiff’s diseases of the liver, 8th ed, vol 1. Philadelphia: Lippincott-Raven, 1999.
14 Glenn F, Becker CG. Acute calculous cholecystitis. Ann Surg. 1982;195:131–136.
15 Sherlock S, Dooley J. Diseases of the liver and biliary system, 10th ed, Oxford: Blackwell Science, 1997.
16 Kalimi R, Gecelter GR, Caplin D, et al. Diagnosis of acute cholecystitis: sensitivity of sonography, cholescintigraphy, and combined sonography-cholescintigraphy. J Am Coll Surg. 2001;193:609–613.
17 Roslyn JJ, Thompson Jr, JE., Darvin H, et al. Risk factors for gallbladder perforation. Am J Gastroenterol. 1987;82:636–640.
18 Shea JA, Berlin JA, Escarce JJ, et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med. 1994;154:2573–2581.
19 Harvey RT, Miller Jr, WT. Acute biliary disease: initial CT and follow-up US versus initial US and follow-up CT. Radiology. 1999;13:831–836.
20 Tint GS, Salen G, Colalillo A, et al. Ursodeoxycholic acid: a safe and effective agent for dissolving cholesterol gallstones. Ann Intern Med. 1982;97:351–356.
21 Sackmann M, Pauletzke J, Sauerbruch T, et al. The Munich gallbladder lithotripsy study: results of the first five years with 711 patients. Ann Intern Med. 1991;114:290–296.
22 Shea JA, Healey MJ, Berlin JA, et al. Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg. 1996;224:609–620.
23 Deziel DJ, Millikan KW, Economou SG, et al. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14.
24 Kiviluoto T, Siren J, Luukkonen P, et al. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321–325.
25 Sandha GS, Bourke MJ, Haber GB, et al. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc. 2004;60:567–574.
26 What if it’s acute cholangitis? Drug Ther Bull. 2005;43:62–64.
27 Cello JP. Acquired immunodeficiency syndrome cholangiopathy: spectrum of disease. Am J Med. 1989;86:539.
28 Devarbhavi H, Sebastian T, Seetharamu SM, et al. HIV/AIDS cholangiopathy: clinical spectrum, cholangiographic features and outcome in 30 patients. J Gastroenterol Hepatol. 2010;25:1656–1660.
29 Sebagh M, Farges O, Kalil A, et al. Sclerosing cholangitis following human orthotopic liver transplantation. Am J Surg Pathol. 1995;19:81–90.
30 Dilly SA, Sloane JP. An immunohistological study of human hepatic graft-versus-host disease. Clin Exp Immunol. 1985;62:545–553.
31 Wada K, Takada T, Kawarada Y, et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg. 2007;14:52–58.
32 Attasaranya S, Fogel E, Lehman G. Choledocholithiasis, ascending cholangitis and gallstone pancreatitis. Med Clin North Am. 2008;92:925–960.
33 Anciaux ML, Pelletier G, Attali P, et al. Prospective study of clinical and biochemical features of symptomatic choledocholithiasis. Dig Dis Sci. 1986;31:449–453.
34 Verma D, Kapadia A, Eisen GM, et al. EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc. 2006;64:248–254.
35 Yusoff IF, Barkun JS, Barkun AN. Diagnosis and management of cholecystitis and cholangitis. Gastroenterol Clin North Am. 2003;32:1145–1168.
36 Hanau LH, Steigbigel NH. Acute (ascending) cholangitis. Infect Dis Clin North Am. 2000;14:521–546.
37 Lai EC, Mok FP, Tan ES, et al. Endoscopic biliary drainage for severe acute cholangitis. N Engl J Med. 1992;326:1582–1586.
38 Burke DR, Lewis CA, Cardella JF, et al. Quality improvement guidelines for percutaneous transhepatic cholangiography and biliary drainage. J Vasc Interv Radiol. 2003;14:S243–S246.
39 Lazcano-Ponce EC, Miquel JF, Muñoz N, et al. Epidemiology and molecular pathology of gallbladder cancer. CA Cancer J Clin. 2001;51:349–364.
40 Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer. 1995;75:171–190.
41 Ekbom A, Hsieh CC, Yuen J, et al. Risk of extrahepatic bile duct cancer after cholecystectomy. Lancet. 1993;342:1262–1265.
42 Oikarinen H, Paivansalo M, Lahde S, et al. Radiological findings in cases of gallbladder carcinoma. Eur J Radiol. 1993;17:179–183.
43 Donohue JH, Nagorney DM, Grant CS, et al. Carcinoma of the gallbladder: does radical resection improve outcome? Arch Surg. 1990;125:237–241.
44 Gainant A, Cucchiaro G. Surgical treatment of 724 carcinomas of the gallbladder: results of the French Surgical Association Survey. Ann Surg. 1994;219:275–280.
45 Tzakis AG, Carcassonne C, Todo S, et al. Liver transplantation for primary biliary cirrhosis. Semin Liver Dis. 1989;9:144–148.