Benzodiazepines
Benzodiazepines promote the binding of the major inhibitory neurotransmitter γ-aminobutyric acid (GABA) to GABAA receptors. The benzodiazepinergic enhancement of the inhibitory effect of GABA on neuronal excitability is the result of increased neuronal membrane permeability to chloride ions, leading to hyperpolarization and a less excitable state. Most of the effects of benzodiazepines (sedation, anxiolysis, muscle relaxation, anterograde amnesia, and anticonvulsant activity) are consequences of the impact of these drugs on the central nervous system. Benzodiazepines are used to treat insomnia, alcohol withdrawal, and seizures and, most importantly from the anesthesia provider’s perspective, are frequently used to provide sedation and amnesia in the perioperative setting. Major side effects can include lightheadedness, motor incoordination, confusion, and impairment of motor and mental functions. Benzodiazepines have recently been associated with the development of delirium in the intensive care unit (Table 85-1).
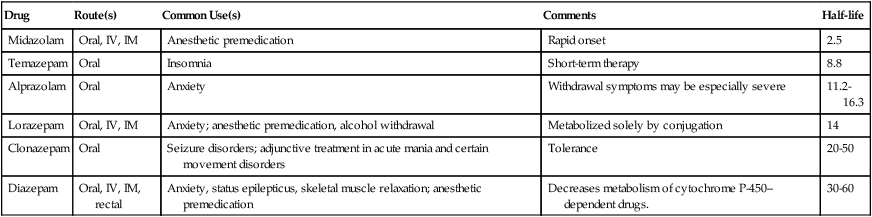
Table 85-1
| Drug | Route(s) | Common Use(s) | Comments | Half-life |
| Midazolam | Oral, IV, IM | Anesthetic premedication | Rapid onset | 2.5 |
| Temazepam | Oral | Insomnia | Short-term therapy | 8.8 |
| Alprazolam | Oral | Anxiety | Withdrawal symptoms may be especially severe | 11.2-16.3 |
| Lorazepam | Oral, IV, IM | Anxiety; anesthetic premedication, alcohol withdrawal | Metabolized solely by conjugation | 14 |
| Clonazepam | Oral | Seizure disorders; adjunctive treatment in acute mania and certain movement disorders | Tolerance | 20-50 |
| Diazepam | Oral, IV, IM, rectal | Anxiety, status epilepticus, skeletal muscle relaxation; anesthetic premedication | Decreases metabolism of cytochrome P-450–dependent drugs. | 30-60 |