97
B-Cell Lymphomas of the Skin
General
PCBCL
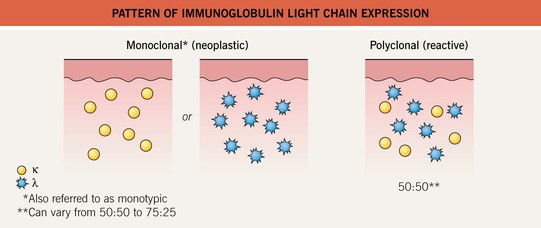
• B-cell lineage is identified by the presence of CD20 and CD79a and the absence of CD3 markers.
• Usually affects older adults and males > females.
• Once the diagnosis of a B-cell lymphoma in the skin has been made, complete staging (Table 97.1) is recommended to distinguish between primary and secondary cutaneous lymphoma.
Table 97.1
Recommended staging evaluation for patients with confirmed diagnosis of B-cell lymphoma involving the skin.
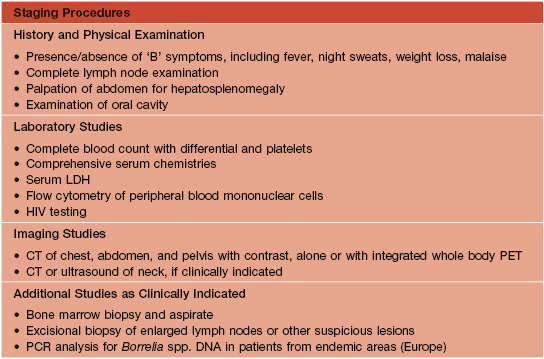
LDH, lactate dehydrogenase; CT, computerized tomography; PET, positron emission tomography; HIV, human immunodeficiency virus; PCR, polymerase chain reaction.
• The new World Health Organization–European Organization for Research and Treatment of Cancer (WHO–EORTC) classification provides the basis for a consistent classification of patients and divides PCBCL into four major types (Table 97.2).
Table 97.2
WHO–EORTC 2005 classification of B-cell lymphomas with primary cutaneous manifestations [corresponding entity in the WHO 2008 classification].
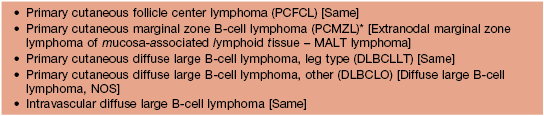
* Includes cases previously designated as primary cutaneous immunocytoma and primary cutaneous plasmacytoma.
NOS, not otherwise specified.
• Primary cutaneous marginal zone B-cell lymphoma (PCMZL) and primary cutaneous follicle center lymphoma (PCFCL) are indolent lymphomas with 5-year survival rates of ≥95% (Table 97.3).
Table 97.3
The primary cutaneous B-cell lymphomas (PCBCLs): clinical and diagnostic features and recommended treatment options.
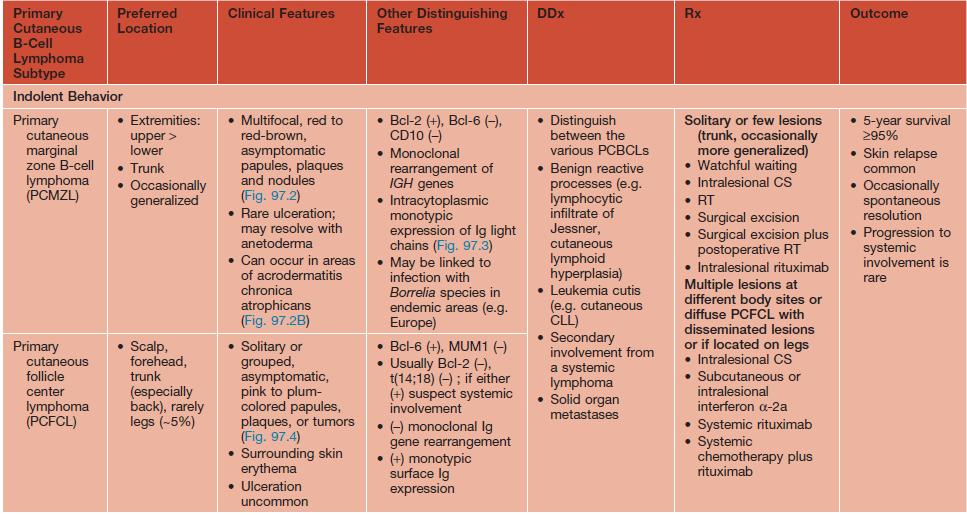
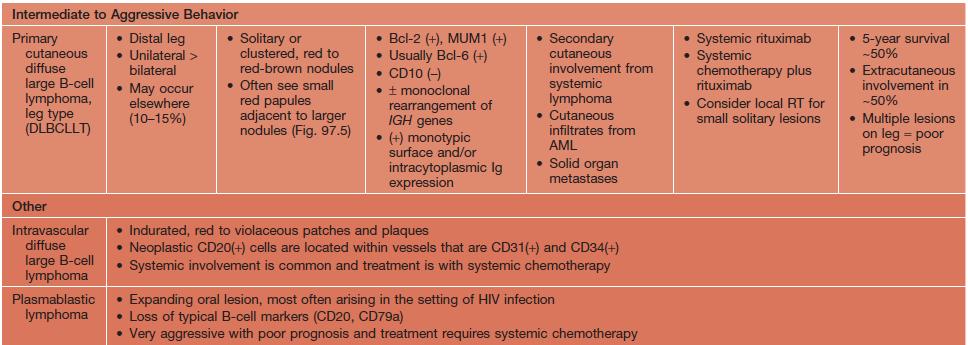
Ig, immunoglobulin; CLL, chronic lymphocytic leukemia; PCR, polymerase chain reaction; RT, radiotherapy; AML, acute myelogenous leukemia.
• Diffuse large B-cell lymphoma, leg type (DLBCLLT) and diffuse large B-cell lymphoma, other (DLBCLO) are in a group with intermediate clinical behavior, worse 5-year survival estimates, and require more aggressive treatment (see Table 97.3).
• An approach to the patient with a suspected diagnosis of cutaneous B-cell lymphoma is shown in Fig. 97.1.
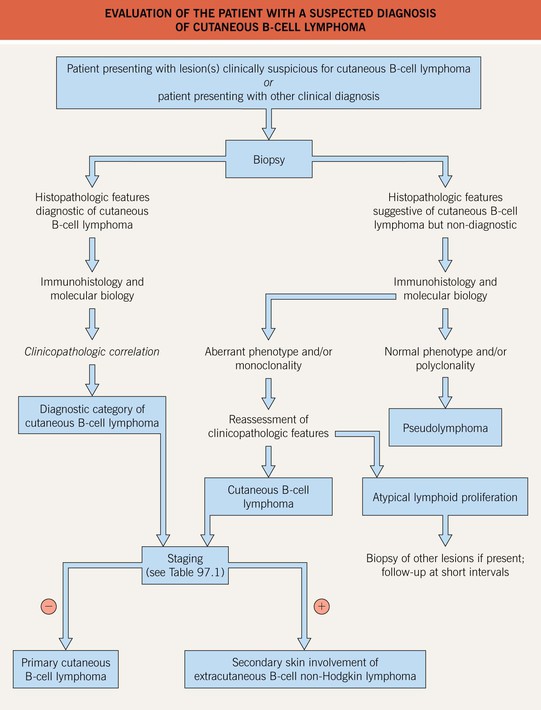
Fig. 97.1 Evaluation of the patient with a suspected diagnosis of cutaneous B-cell lymphoma. Algorithm outlining approach to the patient. Courtesy, Lorenzo Cerroni, MD.


Fig. 97.2 Cutaneous marginal zone B-cell lymphoma. A Two well-circumscribed, erythematous nodules on the shoulder. B Dome-shaped erythematous nodule with smooth surface. The surrounding area shows features of acrodermatitis chronica atrophicans. This tumor, which demonstrated prominent lymphoplasmacytic differentiation histopathologically, was classified as a cutaneous immunocytoma in the past. A, B, Courtesy, Lorenzo Cerroni, MD.


Fig. 97.4 Cutaneous follicle center lymphoma. A Large ulcerated tumors on the scalp surrounded by infiltrated erythematous nodules and plaques. B Large ulcerated tumor on the back. Note surrounding erythematous papules, patches, and plaques (Crosti’s lymphoma). A, B, Courtesy, Lorenzo Cerroni, MD.
Plasma Cell Dyscrasias, Including Multiple Myeloma
• While proliferations of plasma cells in the skin are unusual, cutaneous disorders associated with or thought to be related to a monoclonal gammopathy are more common (Table 97.4).
Table 97.4
Cutaneous conditions associated with a monoclonal gammopathy.
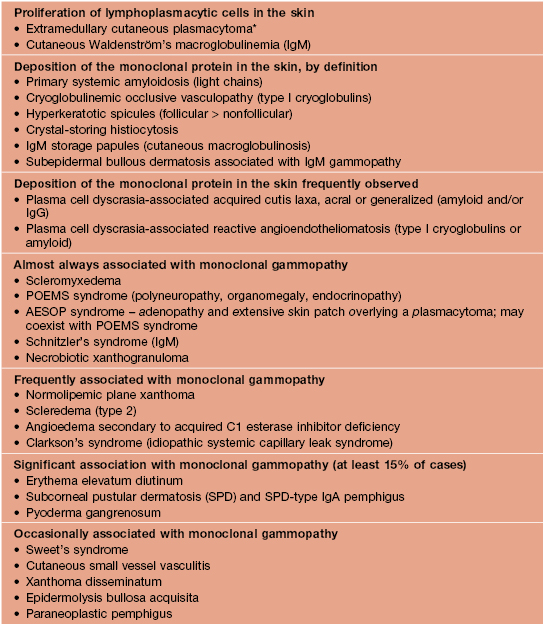
* In the current WHO–EORTC classification (see Table 97.2), primary cutaneous plasmacytoma is classified as primary cutaneous marginal zone B-cell lymphoma.
For further information see Ch. 119. From Dermatology, Third Edition.