CHAPTER 22 Arthroscopic Microfracture and Chondroplasty
Imaging and diagnostic studies
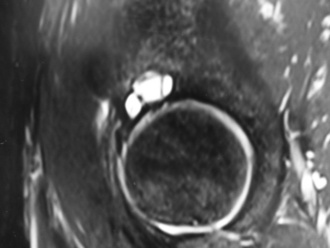
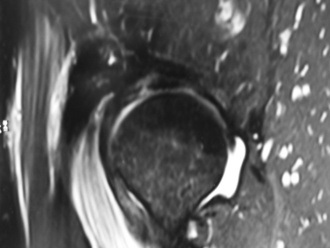
Magnetic resonance imaging may be helpful to obtain a cause of the pain; however, many authors have noted that articular cartilage defects are frequently not clearly identified by the imaging sequences and resolutions that are often used (Keeney CORR 2004). Secondary signs of articular cartilage damage may be identified, such as subchondral bony cysts, bone edema (Figure 22-1), and joint effusions. High-resolution images may demonstrate distinct defects (Figure 22-2), articular cartilage thinning, or heterogeneity of the articular cartilage signal (Figure 22-3). The use of a surface coil with high-resolution, cartilage-sensitive images in the axial, coronal, and sagittal planes may provide a higher spatial resolution that could be helpful for diagnosis. Magnetic resonance arthrography improves the ability to evaluate the articular surface, but current techniques lack reliable sensitivity. In the future, the use of delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) may provide additional information about the proteoglycan content of the articular cartilage.
Surgical technique
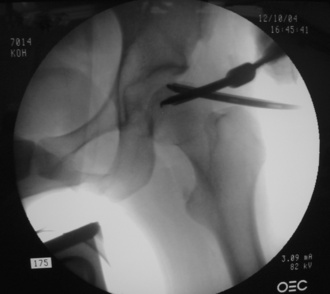
A spinal needle is then placed into the hip joint, and the stylet is removed; this breaks the vacuum seal and decreases the force needed to distract the joint. If necessary, the needle should be repositioned to avoid the labrum. This initial portal should be placed so that the tip of the needle enters the fovea of the acetabulum; this helps to ensure the good visualization of the joint. After the appropriate placement of the initial spinal needle and the guidewire, portal placement with the use of cannulated trocars can be performed to allow for access to the joint for visualization and instrumentation. A thorough diagnostic examination of the hip should occur, and this should involve the use of multiple portals. In some cases, defects on the femoral head are relatively medial (Figure 22-4), and careful instrument placement (Figure 22-5) is necessary to identify and treat defects (Figure 22-6, A and B).
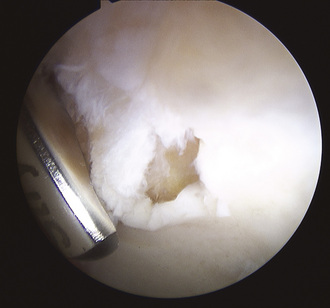
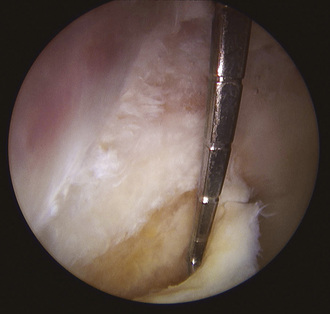
After a defect is identified, the area should be debrided thoroughly with a motorized shaver, curette, or arthroscopic knife. All unstable cartilage should be debrided down to exposed bone until smooth vertical walls of healthy cartilage remain (Figure 22-7). Delaminated articular cartilage flaps are common adjacent to cam-type labral detachment lesions and should be removed (Figure 22-8). Thorough chondroplasty helps to ensure that the fibrin clot that forms after the microfracture stays within the defect.
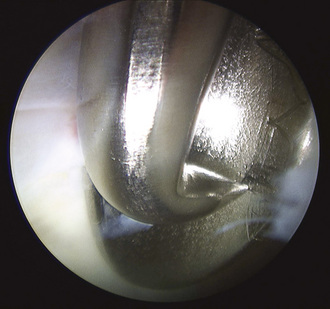
Arthroscopic awls should be placed through portals that allow for access to the defect. The insertion and positioning of these instruments are significantly aided by the use of a slotted cannula (Figure 22-9). The semicylindric shape of this cannula allows irregularly shaped tools to enter into the joint. Subsequently, the slotted cannula can be removed to allow for the freer movement of the awl. As a result of the direction of instrument insertion into the joint, higher-degree angle-tipped awls (i.e., up to 90 degrees) are often used (Figure 22-10). Gentle punctures through the subchondral bone are created and spaced 3 mm to 4 mm apart to cover the area of the defect. If they are placed closer to one another, a bone fragment may break off, and the clot may not be retained. In addition, excessive force can cause the fracture holes to spread. Special attention should be paid to the depth of the awl puncture. A puncture depth of 2 mm to 4 mm will ensure that blood and fat droplets are discharged from the holes. The verification of an adequate depth of penetration can be performed by the application of suction to the area to see if blood or fat emerges (Figure 22-11). When the surgeon is satisfied with the microfracture, the instruments and the arthroscopic fluid should be removed from the joint. The incisions should be closed in the surgeon’s preferred manner, and a sterile dressing is then applied.
Technical Pearls
Results
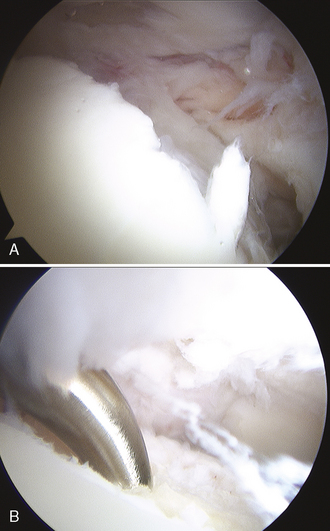
In our experience, extensive areas of delamination or articular cartilage lesions are indicative of degenerative disease and are typically not successfully treated with microfracture. In addition, we have observed that hip arthritis can progress extremely rapidly over a period of several months and that it is unlikely in these cases that the treatment of focal defects will alter the course of the disease. The most successful results are found among young patients with acute pathology without any degenerative condition. Articular cartilage lesions associated with labral pathology and femoroacetabular impingement have had less satisfactory results if the underlying impingement pathology is untreated. At times, this requires labral detachment, the debridement of a pincer lesion that typically encompasses part of the cartilage defect, and labral refixation (Figure 22-12).
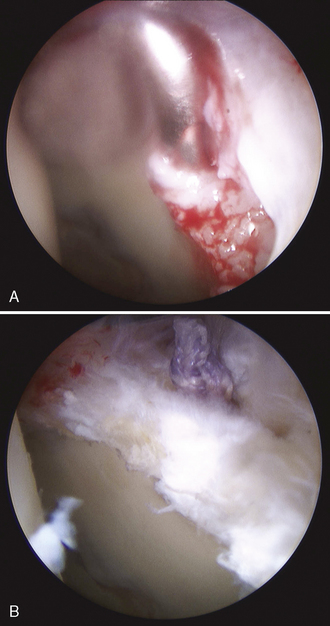
Figure 22–12 A, Anchor insertion into the debrided acetabular rim, as seen in Figure 22–7. B, The same area after repair with the arthroscopic mattress stitch.
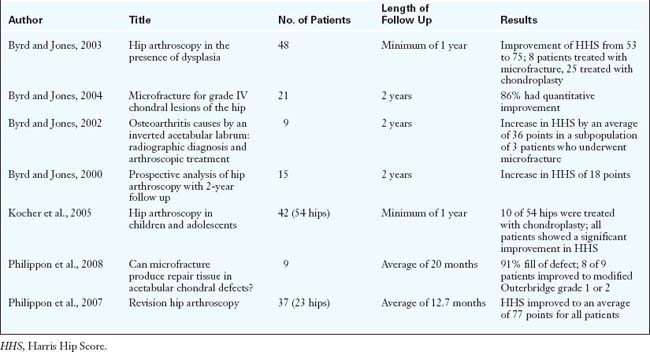
There are only a limited number of studies that have evaluated the efficacy of microfracture (Table 22-1). Byrd and Jones looked at 21 cases of microfracture (19 acetabular cases, 1 femoral head case, and 1 case that involved both of these areas) and found an improvement in the mean Harris Hip Score from 51.4 to 75.2. Magnetic resonance imaging and arthrography revealed the pathology in only 19% of cases, and the average defect size was 12.2 mm2 (range, 6 mm2 to 17.5 mm2). Labral tears were found in 17 of these cases, and degenerative ligamentum teres tears were found in 3 cases. The mean age of the patients was 35 years. At a minimum of 2 years of follow up, the authors found that 86% of patients had improved from the time of surgery. These authors also reported about 9 patients who were treated for inverted articular labrums. Three patients had chondral defects that were treated with microfracture, and these patients subsequently had the best outcomes of the group: they returned to their original baseline of activity and increased their Harris Hip Scores by an average of 36 points. In another study of arthroscopy and dysplasia, the investigators performed 8 microfracture procedures, with similar improvements seen in the Harris Hip Scores. Again, almost all of these patients had concomitant labral debridement.
Annotated references and suggested readings
Bharam S., Draovitch P., Fu F.H., Philippon M.J. Return to competition in pro athletes with traumatic labral tears in the hip. Abstract. In American Orthopaedic Society for Sports Medicine. FL: Orlando; June 2002. (AOSSM)
Byrd J.W.T., Jones K.S. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055-1060.
Byrd J.W.T., Jones K.S. Microfracture for grade IV chondral lesions of the hip. Arthroscopy. 2004;20:e41.
Byrd J.W.T., Jones K.S. Osteoarthritis caused by an inverted acetabular labrum: radiographic diagnosis and arthroscopic treatment. Arthroscopy. 2002;18:741-747.
Byrd J.W.T., Jones K.S. Prospective analysis of hip arthroscopy. Arthroscopy. 2000;16:578-587.
Crawford K., Philippon M.J., Sekiya J.K., Rodkey W.G., Steadman J.R. Microfracture of the hip in athletes. Clin Sports Med. 2006;25:327-335.
Frisbie D.D., Oxford J.T., Southwood L., et al. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop. 2003;407:215-227.
Keeney J.A., Peelle M.W., Jackson J., Rubin D., Maloney W.J., Clohisy J.C. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;249:163-169.
Kocher M.S., Kim Y.J., Millis M.B., et al. Hip arthroscopy in children and adolescents. J Pediatr Orthop. 2005;25:680-686.
McCarthy J., Barsoum W., Puri L., Lee J.A., Murphy S., Cooke P. The role of hip arthroscopy in the elite athlete. Clin Orthop Relat Res. 2003;406:71-74.
McCarthy J.C., Noble P.C., Schuck M.R., Wright J., Lee J. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25-37.
Mithoefer K., Williams R.J., Warren R.F., Wickiewicz T.L., Marx R.G. High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med. 2006;34(9):1413-1418. 3rd
Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918-1921.
Philippon M.J., Schenker M.L., Biggs K.K., Maxwell R.B. Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy. 2008;24:46-50.
Shindle M.K., Voos J.E., Heyworth B.E., et al. Hip arthroscopy in the athletic patient: current techniques and spectrum of disease. J Bone Joint Surg Am. 2007;89:29-43.