CHAPTER 16 Arthroscopic Iliotibial Band Lengthening and Bursectomy for Recalcitrant Trochanteric Bursitis and Coxa Saltans Externa
Indications
Operative intervention is indicated for the following patients:
Surgical technique
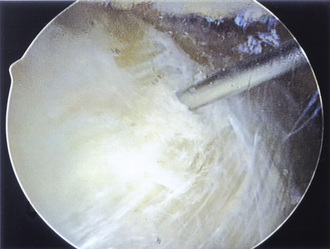
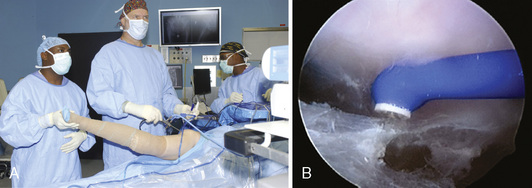
Our preferred surgical technique for recalcitrant trochanteric bursitis is an arthroscopic trochanteric bursectomy. Patients are positioned in the lateral decubitus position with the affected extremity facing up. A deflatable beanbag is used to stabilize the patient, and all bony prominences are well padded. The leg is draped freely so that the hip can be taken through a full range of motion (Figure 16-1). The greater trochanter is palpated and outlined on the skin with a marker. A spinal needle is then inserted directly onto the trochanteric prominence. The needle is then withdrawn slightly by several millimeters, and approximately 30 mL to 40 mL of normal saline is injected into the bursa, thus creating a space underneath the ITB. We prefer to leave the needle in for the purpose of localization. Next, a proximal portal is created 2 cm to 3 cm proximal to the trochanter, and a distal portal is created 2 cm to 3 cm distal to the trochanter. The skin is incised in line with the long axis of the femur. A 4-mm, 30-degree arthroscope is introduced directly into the subcutaneous tissues above the ITB. A 4.5-mm shaver is placed in the other portal and localized to the arthroscope with a triangulation technique (Figure 16-2). The fat directly above the ITB is removed to allow for full visualization of the ITB (Figure 16-3). An arthroscopic ablation probe can also be used to maintain hemostasis and concurrently to remove adherent tissues.

Figure 16–1 The patient is positioned in the lateral decubitus position, with the entire hip and leg draped free.
After the ITB is clearly identified, the arthroscopic ablator is used to create a longitudinal incision approximately 7 cm to 8 cm in length in line with the fibers of the ITB just slightly posterior to its midline and the trochanteric prominence; this exposes the trochanteric bursa (Figure 16-4). The surgical assistant abducts the leg to further relax the incised ITB (Figure 16-5) and to allow the surgeon to advance the arthroscope and instruments underneath the ITB. Next, the shaver and the ablator are used to thoroughly debride the bursa and its thick, fibrous adhesions. Having the assistant slowly internally and externally rotate the leg brings the posterior and anterior portions of the bursa, respectively, into view. Extreme internal rotation is avoided, because this maneuver places the posteriorly located sciatic nerve at risk. Coagulation is frequently necessary to maintain hemostasis and visualization.
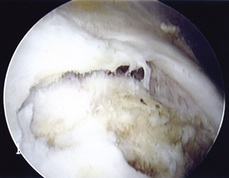
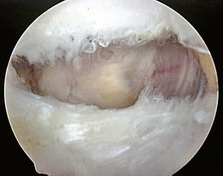
After the bursa has been completely excised, the tendinous attachments of the gluteus minimus and the gluteus medius to the greater trochanter can be seen. Occasionally, irritation and scuffing of the tendinous insertions are noted, and, infrequently, tears and avulsions of the tendons (so-called rotator cuff tears of the hip) are present (Figure 16-6). Early in our experience, we treated the tears with gentle debridement, but, more recently, we have repaired these tears with nonabsorbable sutures with the use of a technique that is similar to the marginal convergence repair technique used for rotator cuff tears in the shoulder. After bursal excision has been completed and hemostasis is ensured, the instruments are withdrawn, and excess fluid is expressed from the portals. The portals are then closed with nylon suture, and a compression dressing and ice pack are applied.
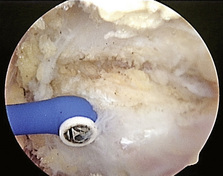
In patients with associated external coxa saltans, an ITB lengthening procedure is necessary in addition to the standard trochanteric bursectomy. After the usual slightly posterior longitudinal incision is made in the ITB, the arthroscopic ablator is used to gently resect its anterior and posterior edges. Additional tissue is removed near the center of the midline cut to create an elliptical resection of the ITB (Figure 16-7). The posterior resection is slightly greater than the anterior resection, because the snapping usually results from the thickened posterior portion of the ITB flipping over the greater trochanter. An alternative method is to perform a crisscross secondary transverse incision, thereby effectively creating a cruciate-type release. The hip is taken through a range of motion to ensure adequate decompression and resection. The bursa is then resected as previously described.
Technical Pearls
Results and outcomes
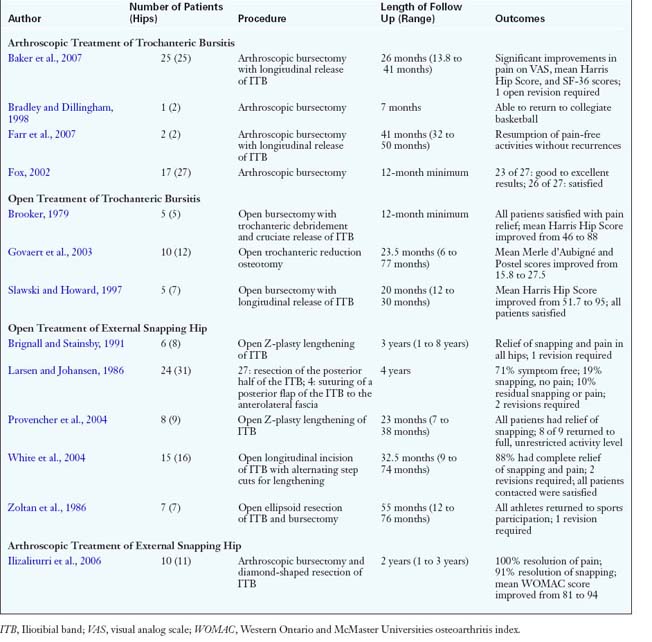
In general, both open and arthroscopic treatments of trochanteric bursitis result in a high percentage of good outcomes (Table 16-1). Physicians agree that, in the majority of patients with this condition, a conservative approach will be successful; only a select few patients will require operative intervention. For a successful result in patients with external coxa saltans, the ITB should be effectively lengthened by one of several open or arthroscopic methods, such as a Z-plasty, an ellipsoidal-shaped or diamond-shaped resection, a cruciate or cross-shaped incision, or a simple longitudinal release.
Baker C.L.Jr, Massie R.V., Hurt W.G., et al. Arthroscopic bursectomy for recalcitrant trochanteric bursitis. Arthroscopy.. 2007;23:827-832.
Bradley D.M., Dillingham M.F. Bursoscopy of the trochanteric bursa. Arthroscopy.. 1998;14:884-887.
Brignall C.G., Stainsby G.D. The snapping hip: treatment by Z-plasty. J Bone Joint Surg Br.. 1991;73:253-254.
Brooker A.F.Jr. The surgical approach to refractory trochanteric bursitis. Johns Hopkins Med J.. 1979;145:98-100.
Farr D., Selesnick H., Janecki C., et al. Arthroscopic bursectomy with concomitant iliotibial band release for the treatment of recalcitrant trochanteric bursitis. Arthroscopy.. 2007;23:905. e1–5. Epub 2007 Jan 25
Fox J.L. The role of arthroscopic bursectomy in the treatment of trochanteric bursitis. Arthroscopy.. 2002;18:E34.
Gordon E.J. Trochanteric bursitis and tendinitis. Clin Orthop.. 1961;20:193-202.
Govaert L.H., van der Vis H.M., Marti R.K., et al. Trochanteric reduction osteotomy as a treatment for refractory trochanteric bursitis. J Bone Joint Surg Br.. 2003;85:199-203.
Ilizaliturri V.M.Jr, Martinez-Escalante F.A., Chaidez P.A., et al. Endoscopic iliotibial band release for external snapping hip syndrome. Arthroscopy.. 2006;22:505-510.
Kagan A.II. Rotator cuff tears of the hip. Clin Orthop Relat Res.. 1999;368:135-140.
Larsen E., Johansen J. Snapping hip. Acta Orthop Scand.. 1986;57:168-170.
Provencher M.T., Hofmeister M.P., Muldoon M.P. The surgical treatment of external coxa saltans (the snapping hip) by Z-plasty of the iliotibial band. Am J Sports Med.. 2004;32:470-476.
Slawski D.P., Howard R.F. Surgical management of refractory trochanteric bursitis. Am J Sports Med.. 1997;25:86-89.
White R.A., Hughes M.S., Burd T., et al. A new operative approach in the correction of external coxa saltans: the snapping hip. Am J Sports Med.. 2004;32:1504-1508.
Zoltan D.J., Clancy W.G.Jr, Keene J.S. A new operative approach to snapping hip and refractory trochanteric bursitis in athletes. Am J Sports Med.. 1986;14:201-204.