CHAPTER 15 Arthroscopic Capsular Plication and Thermal Capsulorrhaphy
Basic science
The surrounding capsular envelope consists of three ligaments: the iliofemoral ligament (i.e., the Y ligament of Bigelow), the pubofemoral ligament, and the ischiofemoral ligament (Figure 15-1). The iliofemoral ligament has a medial and lateral limb proximally, and distally it forms a deep circular band that surrounds the femoral neck in a leash-like fashion; this area is called the zona orbicularis. This “Y ligament” is the strongest, and it prevents the anterior translation of the hip during extension and external rotation when its fibers tighten. In flexion, these fibers loosen, which leads to a “screw home” effect in full extension. The pubofemoral ligament is slightly inferior to the iliofemoral ligaments, and it also controls external rotation in extension. The ischiofemoral ligament is a posterior structure that controls internal rotation in flexion and extension. Other secondary hip stabilizers include the ligamentum teres and the psoas tendon, which may provide important stability in cases of dysplasia or static ligament deficiencies.
Brief history and physical examination
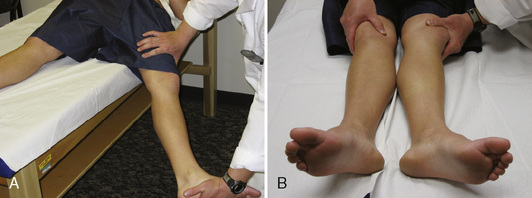
During the physical examination, the patient’s spine should first be examined to rule out other causes of hip pain. This should be followed by an examination of the elbows, hands, and knees to look for signs of hypermobility. Attention should also be paid to the patient’s skin and eyes. Next, the range of motion of both hips should be assessed. These patients often have an increased range of motion as a result of capsular laxity, but any significant increase in internal rotation should heighten one’s suspicion of increased femoral anteversion or other osseous abnormalities. This is followed by a thorough neurovascular examination that includes the reflexes. Next, specific hip testing should be performed, including the Ober test, the bicycle test, the psoas test, and the impingement test. In many cases, this process alters dynamic stabilizers (e.g., the iliopsoas) and leads to psoas and flexion contractures, internal coxa saltans, low back pain, and sacroiliac joint pain. Finally, hip-specific testing for capsular laxity should be performed. Patients with this condition will usually experience anterior hip pain while in the supine position with passive hip extension and external rotation (Figure 15-2, A). Patients may also have increased external rotation in full extension and distraction on the affected side (see Figure 15-2, B). Philippon and colleagues classified capsular laxity on the basis of these physical examination findings from grade 1 (mild) to grade 4 (severe), with grade 4 representing collagen vascular diseases.
Imaging and diagnostic studies
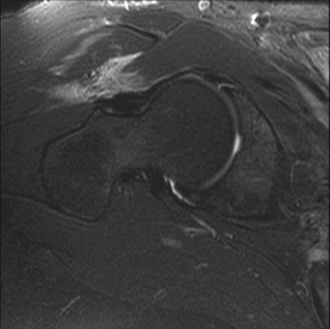
Magnetic resonance imaging (MRI) is critical for the evaluation of atraumatic instability. In the acute setting of traumatic hip injuries, numerous studies have demonstrated that MRI may aid in the diagnosis of chondral injuries, loose bodies, labral tears, femoral head contusions, sciatic nerve injuries, and ligament disruptions. Likewise, in the setting of chronic atraumatic injuries, MRI is also very useful to find subtle derangements in capsulolabral structures (Figure 15-3) as well as osteonecrosis.
Indications
Surgical technique
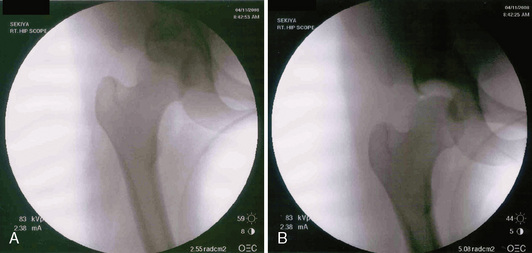
At this point, both of the patient’s feet are well padded, and the patient’s extremities are well secured to the fracture table. A well-padded perineal post is placed in between the patient’s extremities. The nonoperative limb is placed in full extension and mild abduction and then in minimal traction. The operative limb is put through a traction maneuver, which consists of abduction around the perineal post, axial traction, and adduction. Appropriate traction is then confirmed fluoroscopically. In cases of capsular laxity, minimal traction is usually needed to adequately distract the joint (Figure 15-4). The limb is then placed in internal rotation, which decreases the amount of hip distraction, reduces femoral anteversion, and subluxes the femoral head anteriorly, which enables the easy instrumentation of the joint. At this point, traction time is noted and documented.
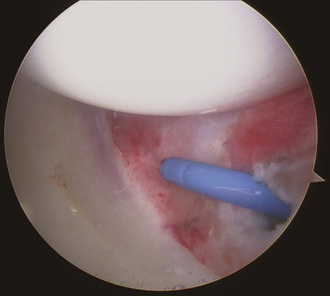
We currently perform three different arthroscopic techniques for atraumatic hip instability: central plication, peripheral plication, and thermal capsulorrhaphy. In many cases, a combination of techniques is performed. As stated previously, in most cases, we perform thermal capsulorrhaphy as an adjunct; rarely do we still use it as a primary mode of treatment. The technique begins as described previously. The capsule is then probed, and, if excessive laxity is present, a focal thermal capsulorrhaphy is performed. A flexible probe (Smith & Nephew, Andover, MA) is used at a temperature of 67 °C and a power of 40 W. We use a technique that is similar to that described by Philippon and colleagues, who used a three-pass cornfield pattern. Care is taken to avoid any charring of tissue, but capsular contraction should be visualized (Figure 15-5). If capsular redundancy is still present after this procedure, a plication may also be performed, which is described later in this chapter.
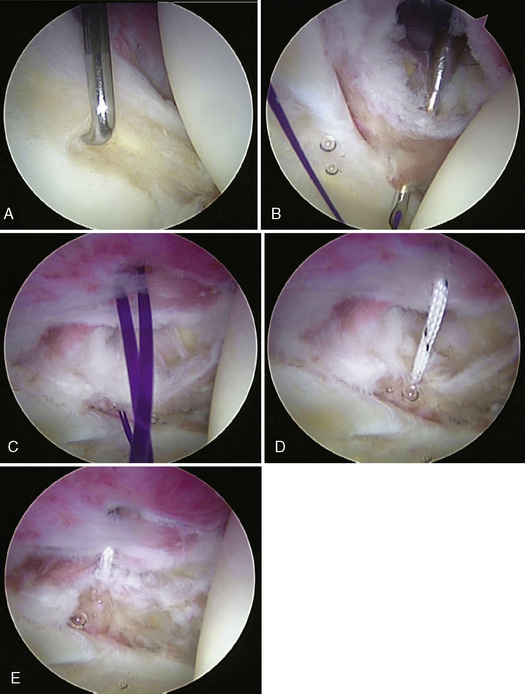
For the central compartment technique, a minimal capsulotomy is performed anteriorly around the anterior portal in the medial limb of the iliofemoral ligament with either a beaver blade or an arthroscopic shaver to create some working room, to improve visualization, to create bleeding edges to help with healing. Then an 8.25 mm × 9 cm cannula (Arthrex, Naples, FL) is placed through the anterior working portal. A soft-tissue penetrator (Spectrum Suture Hook, Largo, FL) is then inserted through the anterior cannula. The penetrator pierces the medial portion of the iliofemoral ligament at the most medial extent of the intended plication. A No. 1 polydioxanone (PDS) suture (Ethicon, Somerville, NJ) is then shuttled into the joint as the penetrator is removed. Next, a soft-tissue penetrator/grasper (Bird Beak; Arthrex, Naples, FL) is inserted through the working portal and used to penetrate the lateral aspect of the iliofemoral ligament at the level of the desired plication. The PDS suture that was previously passed through the capsule and into the joint is grasped and removed from the joint through the cannula. The PDS suture is then used to shuttle a FiberWire suture (Arthrex, Naples, FL) through the capsule as the working suture. A suture grasper is run along the length of the suture to ensure that no tangles exist. The FiberWire suture is checked to verify that it slides. Under direct visualization, the amount of tension and the ultimate plication are observed. Multiple passes, each being a separate plication, can be performed if more reduction in volume or a greater plication is desired. If not, then a blind, extracapsular, locking, sliding knot is tied with a knot pusher and followed by three half-hitch knots to back up the locking sliding knot; the suture is then cut (Figure 15-6, A through E).
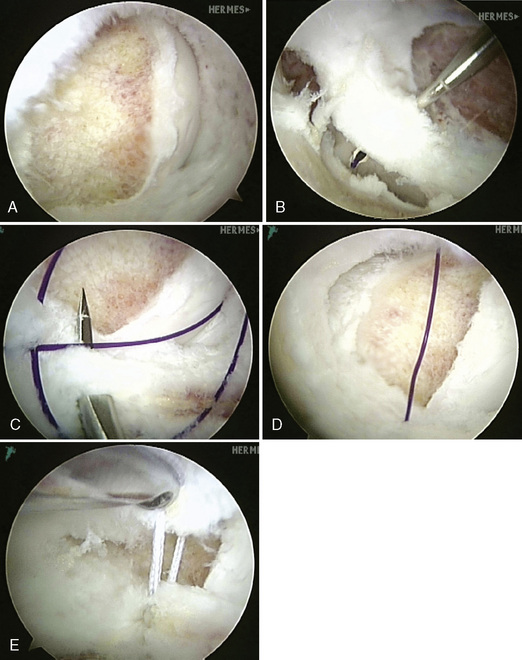
An arthroscopic cannula (Arthrex, Naples, FL) is placed in the anterior working portal. In an identical manner to the intra-articular plication technique, a curved soft-tissue penetrator (Spectrum Suture Hook, Largo, FL) passes a No. 1 PDS suture (Ethicon, Somerville, NJ) after piercing the medial portion of the iliofemoral ligament at the most medial extent of the intended plication. This is most commonly performed from an “outside-in” vantage point, unlike the central technique, which is “inside out.” Next, a Bird Beak (Arthrex, Naples, FL) captures the most lateral extent of intended plication, and a FiberWire (Arthrex, Naples, FL) is shuttled into position. As before, this process may be repeated through the same working portal until the desired amount of plication is achieved. Multiple configurations of capsular sutures can also be used, including a linear series of plications or even a crossing configuration like a “multi-pleat” technique. The plication is completed by tying a locking, sliding knot and backing it with three half-hitch knots. After sufficient capsular tension is achieved, stability is tested with gentle rotational testing. A technique similar to that of capsular plication may be used for posterior plication that involves the use of the appropriate posterior portals, but the posterior neurovascular structures must be carefully considered (Figure 15-7, A through E).
Results
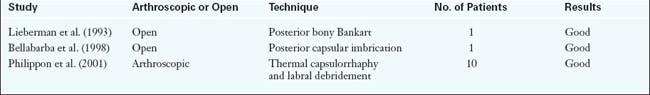
Overall, the literature is quite limited with regard to atraumatic instability and capsular laxity (Table 15-1). In terms of thermal capsulorrhaphy, the trend has been to move away from this modality because of the high rate of associated complications. Although the use of thermal energy as a means of shrinking redundant or lax connective tissues by collagen denaturation has been extensively studied in the shoulder, there are only a few available studies in the hip. Philippon reported about 10 patients who had intractable hip pain with subtle signs of instability on examination in combination with the visualization of redundant capsular tissue during arthroscopy and labral tears. These patients underwent labral tear debridement with thermal capsulorrhaphy. They were allowed to bear weight as tolerated, and they had rotation and extension precautions for 18 days. Preliminary results showed excellent outcomes with regard to the first 8 patients resuming their preinjury athletic activities with minimal or no pain.
Arnoczky S.P., Aksan A. Thermal modification of connective tissues: basic science considerations and clinical implications. Instr Course Lect.. 2001;50:3-11.
Bellabarba C., Sheinkop M.B., Kuo K.N. Idiopathic hip instability. An unrecognized cause of coxa saltans in the adult. Clin Orthop.. 1998;355:261-271.
Braly B.A., Beall D.P., Martin H.D. Clinical examination of the athletic hip. Clin Sports Med.. 2006;25(2):199-210. vii
Clarke M.T., Arora A., Villar R.N. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res. (406); 2003:84-88.
Dall D., Macnab I., Gross A. Recurrent anterior dislocation of the hip. J Bone Joint Surg Am.. 1970;52(3):574-576.
A case report of a recurrent traumatic anterior dislocation of the hip in an adult male..
Elkousy H.A., Sekiya J.K., Stabile K.J., McMahon P.J. A biomechanical comparison of arthroscopic sliding and sliding-locking knots. Arthroscopy.. 2005;21(2):204-210.
Ferguson S.J., Bryant J.T., Ganz R., Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech.. 2003;36(2):171-178.
Ferguson S.J., Bryant J.T., Ganz R., Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech.. 2000;33(8):953-960.
Good C.R., Shindle M.K., Kelly B.T., Wanich T., Warren R.F. Glenohumeral chondrolysis after shoulder arthroscopy with thermal capsulorrhaphy. Arthroscopy.. 2007;23(7):797. e1–e5
Hawkins R.J., Krishnan S.G., Karas S.G., Noonan T.J., Horan M.P. Electrothermal arthroscopic shoulder capsulorrhaphy: a minimum 2-year follow-up. Am J Sports Med.. 2007;35(9):1484-1488.
Hewitt J.D., Glisson R.R., Guilak F., Vail T.P. The mechanical properties of the human hip capsule ligaments. J Arthroplasty.. 2002;17(1):82-89.
Kelly B.T., Williams R.J.3rd, Philippon M.J. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med.. 2003;31(6):1020-1037.
Larson C.M., Guanche C.A., Kelly B.T., Clohisy J.C., Ranawat A.S. Advanced techniques in hip arthroscopy. Instr Course Lect.. 2009;58:423-436.
A review of hip instability and peritrochanteric disorders..
Leunig M., Siebenrock K.A., Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect.. 2001;50:229-238.
Liebenberg F., Dommisse G.F. Recurrent post-traumatic dislocation of the hip. J Bone Joint Surg Br.. 1969;51(4):632-637.
Lieberman J.R., Altchek D.W., Salvati E.A. Recurrent dislocation of a hip with a labral lesion: treatment with a modified Bankart-type repair. Case report. J Bone Joint Surg.. 1993;75A(10):1524-1527.
Martin H.D., Savage A., Braly B.A., Palmer I.J., Beall D.P., Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy.. 2008;24(2):188-195.
McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br.. 1970;52(1):148-159.
Mintz D.N., Hooper T., Connell D., Buly R., Padgett D.E., Potter H.G. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy.. 2005;21(4):385-393.
Moorman C.T.3rd, Warren R.F., Hershman E.B., et al. Traumatic posterior hip subluxation in American football. J Bone Joint Surg Am.. 2003;85-A(7):1190-1196.
Nelson C.L. Traumatic recurrent dislocation of the hip. Report of a case. J Bone Joint Surg.. 1970;52A(1):128-130.
Philippon M.J. Debridement of acetabular labral tears with associated thermal capsulorrhaphy. Operative Techniques in Sports Medicine.. 2002;10(4):215-218.
This paper discusses the operative treatment of capsular laxity..
Philippon M.J. New frontiers in hip arthroscopy: the role of arthroscopic hip labral repair and capsulorrhaphy in the treatment of hip disorders. Instr Course Lect.. 2006;55:309-316.
Philippon M.J. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med.. 2001;20(4):817-829.
Philippon M.J., Schenker M.L. Athletic hip injuries and capsular laxity. Operative Techniques in Orthopaedics.. 2005;15(3):261-266.
This early paper discusses the diagnosis of capsular laxity..
Ranawat A.S., McClincey M., Sekiya J. Anterior hip dislocation after hip arthroscopy in a patient with capsular laxity of the hip: a case report. JBJS Am.. 2009;91(1):192-197.
Sekiya J.K. Arthroscopic labral repair and capsular shift of the glenohumeral joint: technical pearls for a multiple pleated plication through a single working portal. Arthroscopy.. 2005;21(6):766.
Sherlock D.A. Traumatic anterior dislocation of the hip. J Trauma.. 1988;28(3):411-413.
Shindle M.K., Ranawat A.S., Kelly B.T. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med.. 2006;25(2):309-326. ix-x
Shindle M.K., Voos J.E., Heyworth B.E., et al. Hip arthroscopy in the athletic patient: current techniques and spectrum of disease. J Bone Joint Surg Am.. 2007;89- A(suppl 3):29-43.
Tonnis D., Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am.. 1999;81(12):1747-1770.